Uterine polyps are local benign neoplasms growing from the endometrial mucosa. They look like tubercles located on a wide base, or round or oval formations on a thin stalk. There may be one or several of them in the uterine cavity; in the latter case they speak of polyposis. The size of polyps varies from a few millimeters to 8 or more centimeters.
- Signs of a polyp in the uterine cavity and their diagnosis
- When is polyp removal necessary?
- Methods for removing endometrial polyps
- What is hysteroscopy of the uterus for polyps
- Types of hysteroscopy
- Indications for hysteroscopy
- Features of the event
- Preparation
- Basic recovery recommendations
- Complications after polyp removal
- Contraindications
Signs of a polyp in the uterine cavity and their diagnosis
Often uterine polyps do not manifest themselves, but some patients have the following symptoms:
- Menorrhagia - heavy menstruation.
- Bleeding outside of menstruation.
- Spotting after sexual intercourse.
- Bleeding during menopause.
- Infertility and miscarriages.
- With large polyps, women may notice copious whitish discharge, discomfort and pain during intercourse, as well as periodic cramping pain in the lower abdomen.
To make a diagnosis, it is necessary to undergo a comprehensive examination, which includes the following procedures:
- Gynecological examination - particularly large polyps can be palpated during manual examination; cervical polyps can be detected during examination in the speculum.
- Ultrasound of the pelvis - in the uterus, growth of the endometrium with a local increase in its mucous layer is detected. The structure of this neoplasm is homogeneous.
- Separate diagnostic curettage followed by histological examination of the obtained material.
- Hysteroscopy - allows you to examine the endometrium from the inside, visualize single or multiple polyps and determine their location. The procedure is also therapeutic in nature, since it allows for the simultaneous removal of all identified tumors and their subsequent histological examination. This is the most effective method for diagnosing a polyp in the uterus.
Symptoms of endometrial polyp in the uterus
The pathology is characterized by:
- Menstrual irregularities such as hypermenorrhea
- Intermenstrual bleeding
- Uterine bleeding in the postmenopausal period
- Dyspareunia
- Pain when urinating
- Infertility
- Cramping pain in the lower abdomen
In some cases, there are no obvious signs of endometrial polyposis. It is characteristic that the intensity of clinical manifestations of endometrial polyposis increases in proportion to the woman’s age.
When is polyp removal necessary?
The choice of patient management tactics and determination of the need to remove the polyp is determined individually. If a woman is of reproductive age and has no symptoms of a polyp, conservative management tactics can be chosen. In this case, the patient should undergo regular monitoring.
In all other cases, removal of polyps is indicated:
- Presence of symptoms of the disease.
- Pre- and postmenopausal periods, even if there are no symptoms.
Methods for removing endometrial polyps
Surgical removal of endometrial polyps is called polypectomy. It involves curettage of the endometrium followed by histological examination of the resulting material. Curettage can be performed blindly, under visual control using ultrasound or hysteroscopy. The latter method is the most preferable because it allows you to control the completeness of polyp removal and avoid the development of surgical complications (uterine perforation, excessive curettage with damage to the basal layer of the endometrium, etc.).

If treatment does not help, and the patient is in menopause, she may be offered surgery to remove the uterus in the following cases:
- Persistent relapses of multiple polyposis.
- High risk of malignancy of polyps.
- The presence of severe symptoms that significantly worsen a woman’s quality of life.
Endometrial polyp (uterine polyp) - symptoms and treatment
The endometrium is a hormone-sensitive tissue that undergoes cyclic changes. The endometrium is the target organ for sex hormones, and therefore any hormonal disorders lead to pathological changes in the endometrium - disruption of the growth and differentiation of its cells and, as a result, the formation of polyps of the uterine cavity.
In the pathogenesis of endometrial polyps, the main role is played by ovarian dysfunction, leading to the development of hyperestrogenism - an imbalance of hormones in a woman’s body, in which there is an increase in the amount of female sex hormones - estrogens.
There are two types of hyperestrogenism: absolute and relative [6][9][20][25][31]:
- Relative hyperestrogenism - when, with a normal amount of estrogen, the production of gestagens decreases.
- Absolute hyperestrogenism - at any level of gestagens, a large amount of estrogens is produced.
A number of authors claim that the state of absolute hyperestrogenia prevails in the development of this process [18][34], but the majority considers the development of relative hyperestrogenia to be decisive [28].
Disorders of the endometrial receptor apparatus play one of the dominant roles in the development and formation of polyps. Studies devoted to the study of the endometrial receptor apparatus under normal conditions and with its pathological changes have shown that in the pathogenesis of endometrial polyps, an important role belongs to disturbances in the hormone-receptor system [1][6].
Changes in the receptor apparatus of endometrial cells occur as a result of traumatic damage to the uterine mucosa during abortion, curettage of the uterine cavity. Frequent inflammatory diseases of the female genital organs also play an important role in this process.
Work in recent years shows that changes in the “immune surveillance” function play a significant role in the pathogenesis of endometrial polyps. Normally, the immune system controls cell proliferation, correctly recognizes the cells of its own body and eliminates abnormal ones. The hyperplastic process of the endometrium occurs when this mechanism is disrupted, when the immune system does not “see” pathologically altered cells and does not destroy them. The identified shift can be either hereditarily determined or developed during the expression (transfer of genetic information) or mutations of the corresponding genes during the life of patients.
A feature of the endometrial immune system is that it has its own immune mechanisms and is in close contact with the flow of microbial and allergenic material. At the same time, in the endometrium of patients with confirmed adenomatosis (precancerous condition), in addition to a pronounced accumulation of leukocytes and lymphocytes, significant changes in the population composition of lymphocytes and cells of the monocyte-macrophage series were revealed. The literature also contains information about the occurrence of a secondary immunodeficiency state (manifested by a decrease in the content of the total number of T and B cells in the peripheral blood, especially their active fraction) and an interferon deficiency state [38][39][40][41][13].
In the pathogenesis of the development of this proliferative disease, not only cell proliferation (reproduction) takes place, but also suppression of apoptosis processes (a genetically programmed process of cell death). A decrease in apoptosis processes leads to the accumulation of altered cells and, as a consequence, the formation of endometrial pathology.
It has been established that the genetic factor plays one of the main roles in the formation of endometrial polyps. Currently, a hereditary predisposition to the formation of polyps has already been confirmed, since in most cases the disease is observed in several members of the same family. The presence of chromosomal aberration has been proven (changes in the structure of a chromosome caused by its rupture with subsequent redistribution, loss or partial doubling of genetic material). The aberration, in turn, is caused by a change in the structure of some chromosomes, which are associated with the gene responsible for the occurrence of polyps.
Thus, the complex interaction of general systemic processes (neuroendocrine, metabolic, immune) and local changes (receptor and genetic apparatus of endometrial cells), the participation of a number of biologically active compounds (growth and apoptosis factors, cytokines, prostaglandins), as well as hereditary predisposition determine the pathogenesis of pathological endometrial processes [1][6].
Types of hysteroscopy
There are diagnostic or surgical hysteroscopy. Diagnostic involves only examining the endometrium and endocervix for the presence of pathologies. The study is performed on an outpatient basis and does not require serious anesthesia (local anesthesia and sedation are sufficient) and a long recovery period. Therefore, it was called office hysteroscopy. Based on its results, the doctor draws up a plan for further management of the patient.
Surgical hysteroscopy allows for diagnosis and immediate treatment of identified pathologies. It is performed in an operating room and requires full anesthesia. The procedure is prescribed either when the diagnosis has already been established, or when the likelihood of detecting a pathology is extremely high.
We specialize in surgical hysteroscopy because we believe that invasive diagnostic techniques can be successfully replaced by safer tests. This will help make the correct diagnosis without the risk of surgical complications.
Polyps in the uterus: surgical treatment methods
In modern gynecological practice, there are several ways to remove polyps of the cervix and uterine cavity.
Hysteroresectoscopy
Hysteroresectoscopy is a modern technique that involves inserting an endoscope equipped with a video camera into the uterine cavity.
When performing this procedure, the doctor has the opportunity to assess the condition of the uterine cavity, visualize the polyp itself, and also remove it using mechanical, electrosurgical or laser instruments. Then a histological examination of the formation is carried out.
Advantages of hysteroresectoscopy:
- removal occurs under visual control and not blindly;
- the polyp is removed along with its stem, which prevents its re-formation in this particular place;
- there is no negative or harsh effect on the uterine mucosa, which is extremely important for women planning a pregnancy;
- the risks of trauma to the uterus and the addition of an infectious process are minimized;
- after the operation, the woman recovers quickly and can be discharged from the hospital in the near future;
- there is no pain;
- This minimally invasive intervention allows us to minimize risks for patients with somatic pathologies.
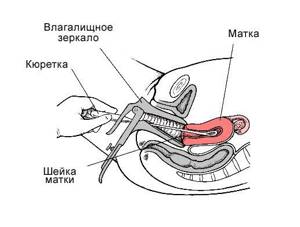
Fractional diagnostic curettage
This surgical intervention involves blind removal of a uterine polyp by curettage of the uterine cavity and cervical canal.
While conducting this study, the doctor is not able to exercise visual control over what is happening in the uterine cavity.
After separate curettage of the canal and the cervical cavity, the resulting material is also sent for histological examination.
According to statistics, after the procedure of curettage of the uterine cavity, recurrence of polyps occurs in more than 50% of cases. That is why in modern gynecology, if there is a diagnosis of “uterine cavity polyp” or “cervical polyp,” treatment involves hysteroresectoscopy of the polyp.
Features of the event
Therapeutic hysteroscopy is carried out on a hospital basis, including a one-day hospital in an operating room. An hour before the start of the intervention, premedication is performed - a sedative injection is given. After being delivered to the operating room, the patient is placed in a gynecological chair and given intravenous anesthesia. Next, proceed to the operation:
- Dilation of the cervical canal.
- A certain amount of sterile liquid is injected into the uterine cavity to “straighten” its walls.
- A hysteroscope is inserted through the cervical canal. As it is introduced, a step-by-step examination of all parts of the uterus is performed. First, the cervical canal is examined, then the uterine cavity and its angles.
- If necessary, surgical procedures are performed - taking a biopsy, removing polyps, dissecting synechiae, etc.
- At the end of the operation, fluid is removed from the uterine cavity.

How is the procedure performed?
Surgical intervention is carried out only in an operating room. A gynecological chair is used for this. The patient must be put under anesthesia. At the preparatory stage, the specialist treats the genitals with an antiseptic, after which the procedure for expanding the cervical canal begins. To do this, use special metal tools of different sizes.
After preparation, a hysteroscope tube is inserted into the uterus, through which fluid is supplied. The cavity should expand. The doctor carefully examines the walls of the organ and their relief. Determines whether the state corresponds to a given cycle period, etc.
After the specialist discovers the polyp, he removes it using special instruments, which he inserts through the hysteroscope tube. All obtained biological materials are sent for histological examination. After the operation is completed, the patient is removed from anesthesia, after which her condition is monitored for two hours. Doctors recommend not planning a pregnancy for 3-4 months after the operation.
Preparation
Preparation for hysteroscopy is similar to other surgical interventions in gynecology. First, an examination and, if necessary, certain treatment are carried out. The following tests are performed:
- General blood and urine analysis.
- Coagulogram.
- Blood type and Rh factor.
- Vaginal smear for flora.
- ECG.
- Test for STIs.
- Tests for HIV and parenteral hepatitis.
Hysteroscopy is planned at the beginning of the menstrual cycle (before day 10), since endometrial tumors are clearly visible during this period.

Immediately before surgery, it is recommended to follow these rules:
- Two days before hysteroscopy, avoid sexual contact.
- On the day of the operation, take a shower and then put on underwear made from natural fabrics.
- Remove jewelry and contact lenses.
- Immediately before entering the operating room, empty your bladder.
- Do not eat for at least 6 hours before anesthesia.
How safe is hysteroscopy?
The procedure itself, although minimally invasive, involves surgical intervention in the body. This means that the risks of complications still exist, although they do not exceed 1%. Possible negative consequences for a woman’s body:
- development of the inflammatory process;
- allergic reactions to anesthesia or a substance that is used to expand the uterine cavity;
- increased bleeding;
- formation of intrauterine adhesions;
- injuries to internal organs (bladder, uterus, intestines).
The risk of complications is directly related to the complexity of the manipulation. When performing an endoscopic examination, it is minimal, but when large nodes in the uterine cavity are removed, it increases significantly.
Basic recovery recommendations
- If an antibiotic is prescribed, take it for as long as your doctor recommends.
- To relieve pain after hysteroscopy, you can take antispasmodics or analgesics.
- Avoid sexual intercourse and heavy physical activity until the bleeding stops, but not less than 10 days.
- Perform hygiene measures in the shower. Taking a bath is not recommended.
- Toilet your genitals as needed, but at least 2 times a day.
- During the recovery period, it is not recommended to use tampons and menstrual cups; discharge should come out of the vagina freely.
Most women generally feel satisfactory after therapeutic hysteroscopy. The main complaints are nagging pain in the lower abdomen and weakness. The full recovery period takes about two weeks. However, if complications develop - fever, heavy bleeding, foul-smelling discharge, you should immediately consult a doctor.
The procedure is contraindicated if:
- there is the slightest suspicion of pregnancy (you did not use contraception this cycle)
- you have any acute infection,
- you have acute colpitis,
- metroendometritis,
- salpingoophoritis, i.e. inflammation of the vagina, uterus or uterine appendages.
Preparation for surgery:
- Maintain sexual rest.
- On the day of the examination, do not eat or drink!
- Shave your pubic hair 2-3 days before surgery.
- On the day of the operation, arrive at the clinic 30 minutes before the scheduled time, as there will be a consultation with the anesthesiologist.
Warn your doctor about bleeding tendencies, allergic reactions and seizures, as well as about all medications you are taking.
Need to know:
- You will be under the supervision of a gynecologist and anesthesiologist for at least an hour after the operation.
- During the first day after surgery, there may be slight bleeding from the genital tract.
- The next menstruation may come a little earlier or later than expected.
It is recommended to monitor body temperature every evening for 7 days after surgery. If your temperature rises above 37 degrees, severe pain, or heavy bleeding, you should immediately consult a doctor. - All doctor’s recommendations must be strictly followed: it is necessary to observe sexual rest for 7 days, then protect against pregnancy using the barrier method (condom) until the end of the cycle, do not douche, do not wash while sitting in the bathroom, only in the shower, do not take a steam bath, do not swim in open water, do not lift weights exceeding three kilograms, do not engage in physical exercise, avoid hypothermia and overheating.
Possible complications:
- Injury to the uterus, which manifests itself as abdominal pain radiating to the collarbone, nausea, dizziness, and bleeding from the genital tract.
- Bleeding from the genital tract - profuse, bright discharge, possibly with clots.
- Acute inflammation of the uterus, which can appear several hours or days after surgery and is manifested by high fever with chills, sharp pain in the lower abdomen, and general malaise.
- Exacerbation of a chronic process in the uterus and fallopian tubes, during which during the first week aching pain in the lower abdomen appears, the temperature rises to 37.2-37.3 degrees, and discharge from the genital tract increases.
- 2.40 Removal of cervical polyp with curettage of the cervical canal and vacuum aspiration of the contents of the uterine cavity (without anesthesia and histology) - see the price list for this procedure
- 2.41 Removal of endometrial polyp, with the cost of histological examination (Hysteroscopy, curettage of the uterine cavity, anesthesia, histology) - check the price in the price list
We will be happy to help you, make an appointment by phone: (843)276-95-35
Complications after polyp removal
As after any gynecological operation, the following complications may develop after hysteroscopy:
- Damage to the wall or cervix - treatment may require additional surgery to close the perforation.
- Damage to the cervix - may require stitches.
- Bleeding.
- Infectious complications.
It should be noted that complications after hysteroscopy are much less common than after other gynecological interventions performed “blindly”. But the possibility of their development cannot be completely excluded.
Treatment of endometrial polyps
A procedure such as removal of a polyp in the uterus is resorted to in most cases after confirmation of the appropriate diagnosis. Conservative therapy in most cases does not have any effect, that is, the hyperplastic formation in the uterine cavity remains.
Treatment involves the elimination of the polyp as a foreign body of the uterus and cervical canal, as well as subsequent histological examination of the removed tissue. This is necessary to prevent the development of oncological pathology against the background of hyperplastic processes of the cervix and endometrium.
Indications and contraindications
Removal of a cervical polyp is carried out only if there are certain indications. These include:
- large polyp size (over 10 millimeters in diameter);
- rapid progression of pathology according to control ultrasound examination;
- presence of intermenstrual bleeding;
- infertility. Problems with conception and a history of spontaneous abortion due to an endometrial polyp are an indication for surgical treatment;
- the presence of an adenomatous polyp (precancerous condition);
- malignant growth of formation.
The procedure of polypectomy (removal of a polyp) is contraindicated in the following conditions:
- with pathology of the cervix (cicatricial deformation, lack of patency of the cervical canal, malignant process);
- acute stage or exacerbation of chronic inflammatory process of the cervix (exocervicitis, endocervicitis);
- presence of uterine bleeding;
- colpitis (inflammatory processes in the vagina of various etiologies).
Preparation for surgery
If an endometrial polyp is detected in the uterus, treatment should begin as early as possible. The procedure to remove such a neoplasm of the cavity or cervix requires preparation.
Before undergoing a polypectomy, a woman undergoes an examination, including:
- blood tests: clinical, biochemical, coagulogram (blood clotting test), HIV, syphilis, and hepatitis markers;
- Analysis of urine;
- vaginal smear for flora and atypical cells;
- colposcopy;
- electrocardiography;
- fluorographic examination.
Since the manipulations are performed under anesthesia, the patient must obtain the opinion of such specialists as a therapist, anesthesiologist, or cardiologist. This is necessary to exclude contraindications for surgical removal of the polyp.
In addition to mandatory examinations, when preparing for polyp removal, a woman must adhere to some rules:
- seven days before the expected date of surgery, you should stop drinking alcoholic beverages;
- three days before the intervention, it is worth excluding foods that promote gas formation from the diet;
- You can eat food no later than 10 hours before the operation;
- on the day of surgery you should not eat or drink;
If a woman is taking any medications, this information must be reported to the attending physician/
Contraindications
- The presence of decompensated chronic diseases that may interfere with anesthesia, for example, cardiovascular pathology.
- Presence of STIs and vulvovaginitis.
- The presence of diseases accompanied by a tendency to bleeding.
Euroonco specialists closely monitor the condition of patients not only in the postoperative period, but also at the initial stage. In this regard, we perform the procedure only after we are convinced that the patient has no contraindications. You can make an appointment for a consultation about uterine polyps by calling:
Book a consultation 24 hours a day
+7+7+78
Unpleasant consequences and normal phenomena after removal of a uterine polyp
Despite the low level of trauma of the technique, after polypectomy the patient should especially carefully monitor her health and immediately report any unusual manifestations to her doctor. Women usually note the following features of the postoperative period:
- Uterine bleeding;
- Uncharacteristic vaginal discharge;
- Moderate pain;
- Changes in the menstrual cycle and the nature of menstruation;
- Increased body temperature.
Let's try to figure out which of the above is considered normal, and which manifestations should concern the patient.