When is a general clinical urine test prescribed?
A general (clinical) urine test is prescribed in the following cases:
- as part of an annual preventive examination (screening);
- during routine examination of pregnant women;
- during the initial diagnosis of any disease;
- for diseases of the urinary system (pyelonephritis, cystitis, etc.);
- if you suspect diabetes mellitus;
- to assess the course of the disease and the effectiveness of treatment;
- persons who have had a streptococcal infection (angina, scarlet fever), for monitoring in order to early detect possible complications.
Acid-base balance is important for the baby
It is also important for us to note and monitor the pH of the child’s urine and saliva; these data are indicative of the child’s health. Special pH testers will allow us to conduct research at home on our own. But you need to know the pH standards of children’s urine and saliva. The normal pH of a newborn's urine is from 4.8 to 5.9. If the baby is premature, the acidity reaches 4.5. Children under one year old who are breastfed have a neutral or alkaline urine pH, approximately 7 - 7.8. After cessation of breastfeeding, the reaction becomes the same as in an adult, from 6 to 7, on artificial feeding from 5.5 to 7.
The acidity of saliva in children is approximately 7.32, in an adult it is 6.40. Data may vary depending on the situation; with accelerated salivation, saliva becomes more alkaline.
The acid-base balance in early childhood is easily disturbed due to frequent respiratory diseases or anemia. In the first year of life, to maintain the acid-base balance, you need to avoid these health problems as much as possible and regularly check the acidity of your urine or saliva with a pH tester.
If you do not maintain the acid-base balance from childhood through a properly structured diet and physical activity, the body will inevitably react to this. At first, increased acidity will affect the general condition: children will be irritable, aggressive, capricious. At school age, they will begin to get tired quickly, nervousness will appear, concentration will decrease, insomnia and agitation will occur, which can lead to depression.
Then pain will appear, which is also not uncommon. Children complain of pain in the back, joints, when they experience cramps, diffuse muscle pain, arthritis, discomfort in the collar area, and so on. In puberty, with an increase in acidity, new skin problems begin with the removal of excess acid through the epithelium, and as a result, acne, increased greasiness, sweating, unpleasant odor, frequent blepharitis, conjunctivitis, and dandruff appear.
Decreased immunity in childhood against the background of increased acidity causes frequent diseases of the ENT organs, chronicity of opportunistic infections, growth of adenoids, frequent otitis media, sore throats, and so on. A child's digestive system is also unable to cope with increased acidity without certain symptoms, including constipation, bad breath, abdominal pain, dyspepsia, gum disease, and tooth decay.
Separately, it should be noted the prevention of osteoporosis in childhood. After all, lack of microelements in childhood leads to the destruction of the skeleton in adulthood. From statistical data it is known that only 30% of children receive microelements from fruits and vegetables, dairy products, and 50% of children receive calories from sugar. Calcium deficiency in a child’s diet acidifies the diet, which also leads to a violation of the blood hormone balance.
From all of the above, it becomes clear why so much attention is paid to acid-base balance. Because not only the child’s health, but also life itself depends on it.
Current methods for measuring pH include the colorimetric method using litmus papers to distinguish acids from alkalis. A more accurate method works with fluorescent dyes and allows intravascular pH measurements.
Indicators that are assessed during general clinical urine analysis
The study evaluates:
- color
– various shades of yellow are acceptable; - transparency
. Cloudiness of urine indicates the presence of pathological elements in it - leukocytes (indicate purulent processes), bacteria, precipitated salts (phosphates), etc. - specific gravity (density)
- depends on the concentration of dissolved substances (urea, uric acid, creatinine, salts. Reduced specific gravity can be a sign of pyelonephritis, increased - glomerulonephritis, diabetes mellitus, cardiovascular failure; - urine reaction (pH)
– assessment of acidity. There are weakly acidic, neutral and slightly alkaline reactions. It should be taken into account that this indicator can be affected by the use of certain vitamins and medications, as well as the nature of the diet: a meat diet increases acidity, a vegetarian diet, on the contrary, makes the reaction slightly alkaline. An increased pH value (alkalinization) may indicate kidney disease, inflammatory processes of various localizations and some other diseases. A low pH value (high acidity) is characteristic of dehydration of the body, which is typical in particular for febrile states, severe diarrhea, and may also indicate diabetes mellitus or some other pathologies; - Protein in urine
is not normally detected. Identified during inflammation and other pathological conditions; - glucose in urine
is normally absent. Glucose in the urine during pregnancy (in the second or third trimester) is gestational diabetes, which usually resolves immediately after delivery. It occurs due to increased stress on the body with high hormone activity. Glucose in the urine during pregnancy is a reason to optimize your lifestyle and diet, but first you need to make sure that the appearance of sugar in the urine is not pathological; - bile pigments - bilirubin and urobilinogen
; - blood cells (leukocytes and erythrocytes), epithelial cells, foreign agents (bacteria, fungi, parasites) and other indicators.
General urine analysis in children and adolescents
Collecting a urine sample.
Midstream urine can be obtained from any child who is holding urine. Washing the genitals and perineum with soap and water before urinating has been shown to reduce urine contamination by periurethral organisms and leukocytes.
Collecting urine samples from infants and toddlers - There are four ways to obtain urine samples from young children who cannot yet control their urination:
A bag of urine: the genitals are carefully examined. cleaned and dried.
The urine collection bag is securely attached. Ideally, the child should have a bowel movement after being given fluids, and the urine sample should be processed immediately. Packaged urine is not suitable for culture because contamination often leads to false-positive results.
Clean urine: To collect a fresh sample of bubbly urine, the child is held on the lap of an adult with the genitals exposed; urine that spontaneously comes out after drinking is collected in a sterile container. This method produces false positive results in 5–26% of cases.
Catheter urine: A suitable urine sample for culture can be obtained from a female infant or toddler by a single catheterization (not from an indwelling bladder catheter). In boys, suprapubic bladder puncture should be performed instead of transurethral catheterization.
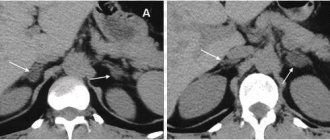
Suprapubic bladder puncture: This is a simple (though rarely performed), relatively non-invasive way of collecting a urine sample when pyelonephritis is suspected, especially in infants. Bladder puncture is indicated in cases where saccular urine contamination is expected, such as in patients with vulvovaginitis, anogenital dermatitis, or phimosis. The puncture is most likely to be successful if the degree of bladder filling is assessed in advance using ultrasound: in newborns and infants, ultrasound increases the likelihood of obtaining an adequate urine sample from 60% to almost 97%.
The first morning void sample is most suitable for biochemical testing, but the second void is more practical in an outpatient setting. Urine should always be collected at the same time of day from each patient so that test results are comparable. Spontaneously passed urine should not be stored for more than 1-2 hours at room temperature or 4 hours in the refrigerator (at 4 °C) before testing, otherwise the cells will disintegrate and the number of bacteria will increase. , and the pH will rise. Urine Collection Common indications for urine collection include determination of endogenous creatinine clearance, quantification and differentiation of proteinuria, and measurement of fluid and electrolyte excretion. The most important factor determining the validity of a test is accuracy, not the total length of time the urine is collected. Urine should be collected in a clean container stored in a cool place. The starting point for collection is the time of the last spontaneous void before collection, and the end point is the time of the last collected void. The duration and total volume of urine collection is documented, and 10–20 ml of mixed urine is analyzed. Accurate urine collection in infants or children with urinary incontinence is only possible with an indwelling bladder catheter. In such cases, single-void urine samples should be reported as the quotient of the parameter in question and the creatinine concentration and compared with age-specific norms. Leukocyturia Leukocyturia makes a urinary tract infection likely; as a single result, it is highly sensitive (83%) but not very specific. The authors recommend microscopic analysis of a freshly obtained native urine sample because, in our opinion, the leukocyte esterase reaction using a urine dipstick test is not a completely adequate replacement for microscopy, although there is controversy in the literature on this issue. A leukocyte esterase test may be positive for lysed leukocytes or subpreputial material even if microscopy does not detect leukocytes; it may also be negative despite positive microscopy if the urine is highly concentrated or contains “flattened” white blood cells. Whatever is tested, the instructions for using the probe should be followed carefully. The number of white blood cells per unit volume is affected by the variable amount of urine each time you urinate. This can change the results of not only strip tests, but also counting chambers and other cell counting methods. A white blood cell count of 5–10/µL is considered abnormal in boys over 3 years of age; in girls, a count in the range of 20–50/μL is suspicious for a urinary tract infection, and a count above 50/μL is considered clearly abnormal. Detection under a microscope of leukocyte casts in urine sediment along with severe bacteriuria is pathognomonic for pyelonephritis. Nitrite test Most pathogens in urine (except enterococci) can reduce nitrates to nitrites; thus, the presence of nitrites in the urine indicates bacteriuria. A nitrite indicator test may be falsely negative if urine is retained in the bladder for too short a time (less than 4 hours). As a result, the sensitivity of the nitrite strip test for clinically significant bacteriuria does not exceed 30–50% in infants who typically urinate every 1–4 hours. On the other hand, its sensitivity in girls under 3 years of age is 98%. The simultaneous manifestation of nitrituria and leukocyturia accounts for 93% of sensitivity for urinary tract infection. Bacteriuria. For urine culture, a fresh urine sample must be obtained and stored at 4–8 °C before and during transport to the laboratory. Alternatively, the sample can be pre-incubated in culture medium and sent directly at 36 °C. The number of bacteria per milliliter is determined; its interpretation depends on how the sample was obtained. The diagnosis of a urinary tract infection requires the presence of at least 105 organisms/ml; more recent studies require a minimum amount of 106 or 107/ml. Lower numbers in catheterized urine may be pathological, and any number of microorganisms detected is pathological in urine obtained by bladder puncture. Depending on how it is obtained, urine culture often has a false-positive rate of up to 25%, and the false-positive rate of bag urine culture ranges from 30% to 63%. A bladder puncture is better than a clean catch and thus provides a much more suitable sample than collecting urine in a bag.
In school-age children, typical clinical manifestations of a urinary tract infection include pain when urinating, increased frequency of urination, and difficulty urinating; pyelonephritis is characterized by flank pain and fever. In case of conflicting results, the urine test should be repeated before taking further, possibly inappropriate diagnostic or therapeutic measures. A history of recurrent or complicated urinary tract infection or recent antibiotic treatment should raise suspicion of a fungal or viral infection or a pathogen that requires special culture media for detection (chlamydia, trichomonas, ureaplasma).
One should critically ask whether the organism demonstrated is typical for the patient's age and sex. At any age and in both sexes, the most common pathogen is E. coli. In boys aged 1 year and older, Proteus species account for up to 30% of urinary tract infections, and Staphylococcus species are found in approximately 30% of urinary tract infections in girls aged 9 to 15 years. Signs of possible infection include low cell counts, mixed flora in one culture, different pathogens in serial studies, and organisms not typically found in urinary tract infections. Routine screening sometimes reveals significant bacteriuria without leukocyturia in apparently healthy children (0.2–2%). This is called asymptomatic bacteriuria and does not require treatment with antibiotics. Urethritis is common in sexually active adolescents. Urinary tract infections are classified as asymptomatic (bacteriuria and leukocyturia without clinical symptoms) or symptomatic (with symptoms, possibly but not necessarily including fever). They can also be classified as uncomplicated or complicated based on the patient's urinary tract anatomy (urinary tract malformations), urinary tract and renal function, and immune competence. In complicated urinary tract infections, culture often reveals multiple pathogens. Colony counts and resistance testing should be performed for each pathogen. Leukocyturia without bacteriuria may represent sterile leukocyturia; its differential diagnosis includes urolithiasis, renal tubular acidosis, interstitial nephritis, cystic kidney disease, glomerulonephritis, febrile illnesses, tuberculosis, appendicitis, vaginitis, meatus/urethral irritation, and dehydration.
Proteinuria. Proteinuria—excessive excretion of protein in the urine—is a sign of tubular or glomerular dysfunction. It is assessed using a midstream urine sample in school-aged children or a pouch urine sample in infants and toddlers. A second void of the day is often used; The first void of the day is the most concentrated, but often cannot be obtained on an outpatient basis. Proteinuria is defined as having a protein concentration of at least 30 mg/dL. Microalbuminuria is present in lower concentrations in 5–12% of asymptomatic children. Ideally, urinary protein should be quantified based on a 24-hour urine collection. Collected urine samples are considered the gold standard for diagnosis. For infants and toddlers, in whom collecting urine samples over time is particularly problematic, protein/creatinine and albumin/creatinine ratios in spontaneously voided urine can be measured instead. These values are independent of urine volume, since the amount of creatinine excreted per day is stable. For the coefficient to be reliable, the urine creatinine concentration must be at least 10 mg/dL; lower values in newborns (including premature infants) and children with polyuria may lead to misinterpretation. A low fraction of albumin in the total amount of protein excreted may indicate an extrarenal cause of proteinuria, such as hemoglobin, myoglobin, light chains (very rare in children), amyloids and other causes.