Pregnancy planning includes a whole range of examinations and activities that will allow a married couple to get pregnant correctly, carry and give birth to a healthy child. One of the important points of this program is the compatibility of blood groups for conception. More than one generation of specialists and ordinary people have experienced those unpleasant moments when such a seemingly trifle as blood grouping prevented the normal completion of pregnancy or the life of a newborn child.
Rh factor and blood group
A responsible approach to planning and bearing a baby can significantly reduce possible negative phenomena that sometimes happen during the 9 months of waiting for a replenishment. One of the preventive tests - determining the compatibility of partners by blood group - may not play a special role for conception, but for the further development of the toddler its importance can be very great.
A possible conflict between mother and baby in her womb due to the Rh factor is practically nothing new to anyone. But not everyone knows about the compatibility of blood in the mother-baby bond for conceiving and bearing a child. There are some combinations that can cause complications during pregnancy.
- Blood type 1
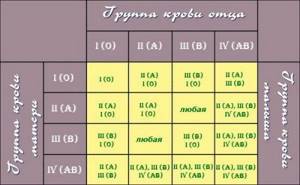
: compatibility for conception. If the mother has the first blood group, and the father of the child has any other, a conflict under the ABO system is possible. If a child has a blood type other than the first, then when they meet the mother’s blood cells, α and β antibodies destroy red blood cells with a foreign antigen. However, there is no need to panic in advance. The presence of the blood type situation described above does not always provoke a conflict, and even without outside intervention, healthy children are born. If the expectant mother wants to play it safe, then after the 30th week she can be tested (once a month) for group antibodies. This conflict (if detected) is less dangerous than the Rhesus conflict. Moreover, with each subsequent pregnancy, the risk of its occurrence decreases more often. - Blood type 2
: compatibility for conception. When the blood of the second group circulates in the expectant mother’s body, the likelihood of incompatibility with the baby arises if the father’s blood is of the third and fourth groups. - Blood type 3
: compatibility for conception. More careful attention is required when the child’s father has group A or AB (second and fourth, respectively), and the mother has the third group. - Blood type 4
: compatibility for conception. If a woman has this blood type, then there is no likelihood of conflict.
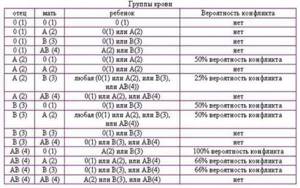
This information in no way suggests that people with “possibly incompatible” blood types should not have children or that such a pregnancy will obviously be problematic. It’s just that future mothers and fathers should know that a certain combination of blood groups may require additional attention (blood tests, ultrasound) on their part.
If antibodies are detected in the blood of a pregnant woman, treatment is not prescribed immediately and not always - the doctor monitors the dynamics of this indicator. If intervention is necessary, therapy is prescribed. The most effective and safe method is plasmapheresis, although it also has a number of contraindications. When a conflict is detected, the optimal therapy is selected by the doctor.
Ureaplasma is a bacterium that provokes inflammatory diseases in the genitourinary system. Urgent treatment of ureaplasmosis is necessary if a person is a carrier and mucosal damage is detected. Read more in the article: “how to treat ureaplasma in a woman with drugs.”
What does blood type affect?
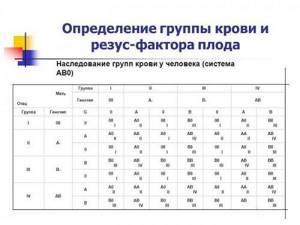
Blood type is an inherited trait that does not change throughout life. The most common system for dividing blood into groups is the AB0 system. Depending on the presence of certain proteins on the surface of red blood cells, called aglutinogens, and proteins found in the plasma - aglutinins, four blood groups are distinguished: 0 (zero) - first, A - second, B - third and AB - fourth. It is this system that is used to select blood during transfusion.
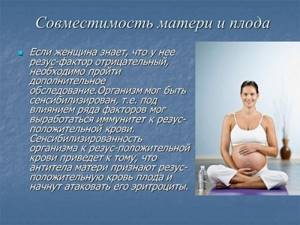
Another important protein, the presence of which determines blood identity, is the Rh antigen. Approximately 85% of people have this protein in their blood and are called Rh positive. The remaining 15% do not receive this blood protein from their parents and are called Rh negative.
The belonging of potential parents to one or another blood group and the Rh factor do not affect the ability to conceive. A much more important role is played by which blood type and Rh affiliation the fetus will inherit. If there is “incompatibility” (the more precise medical term is “isoserological incompatibility”) of the blood of the mother and fetus, complications may develop: spontaneous miscarriages and premature birth, hemolytic disease of the fetus and newborn.
Incompatibility problem
The Rh factor is checked using a blood test. “Rh−” poses a threat to the mother in labor if her Rh does not coincide with the baby’s Rh. Research has shown that some problems are related to blood type incompatibility between mother and fetus or between parents. As written above, markers (antigens) protect the body from external pests such as bacteria and viruses. When an antigen encounters a foreign object, it creates antibodies against it. The same thing can happen when trying to get pregnant. The body will react by producing antibodies to the appearance of sperm or a fetus, which will prevent conception.
Many migraine medications help manage the symptoms but do not cure the pathology. Triptans are a group of medications that are intended specifically for the treatment of the disease. Read more in the article: “triptans for migraines.”

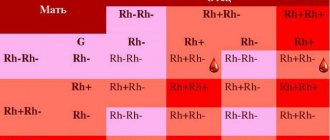
The problem appears when the Rh of the mother's blood does not match the Rh of the fetus, and the body begins to produce antibodies against proteins on the baby's red blood cells. An Rh-negative mother does not always pose a threat to fetal development:
- if both parents are Rh-negative and the child also receives “Rh−”, then no complications arise;
- if the mother has “Rh−” and the father “Rh+”, and the fetus receives Rh negative, then there is no threat of conflict;
- if the woman in labor has “Rh+” and the child has Rh negative, protein incompatibility will not occur.
The chance of a child inheriting Rh and the probability of conflict in the table.
Rh factor
| Father | Mother | Child | Probability of conflict |
| + | + | 75% + 25% — | No |
| + | — | 50% + 50% — | 50% |
| — | + | 50% + 50% — | No |
| — | — | — | No |
What can happen?
The influence of blood type on conception and the absence of Rh conflict is very large. A pregnancy complicated by the presence of a rhesus conflict between the parents, if appropriate treatment is not prescribed, may be interrupted and a miscarriage may occur. Antibodies produced in the woman’s body will strive to destroy the embryo. There is even an opinion that if the blood is compatible at conception according to the Rh factor, as well as if the future father has a blood group higher than that of the mother, then the chances of a quick conception increase greatly, such blood compatibility at conception contributes to a favorable pregnancy and the birth of a strong baby .
Most of the world's population has a positive Rh factor; a negative one can be found in 10-15% of people. The development of Rh conflict occurs when a woman is Rh negative and a man is Rh positive. Even in such a situation, Rh discrepancy may not be dangerous for the health of the mother and baby; the main thing is to constantly be monitored by a specialist. In other cases, Rh conflict will not occur. Most often, such compatibility of blood groups for conception, burdened by a Rh conflict, is extremely rare (up to 3% of women).

Rhesus conflict between mother and fetus during pregnancy
Rh conflict is a reaction of a pregnant woman’s immune system to the baby’s red blood cells. At the same time, they are destroyed, and hemolytic disease of the fetus develops. A large amount of bilirubin enters his blood, which has a toxic effect on all organs, including the brain. The most unfavorable outcome of Rh conflict is spontaneous termination of pregnancy.
Causes and mechanism of development of Rh conflict
Rh antigen is a protein that is found in the membrane of red blood cells (blood cells that transport oxygen). If a person has it, the Rh factor is considered positive (85% of the world's population); if not, it is considered negative (15% of people).
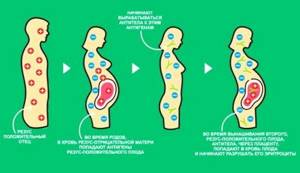
Rh conflict is possible if the mother is Rh negative and the child is Rh positive. It is also known that in a Rh-negative woman who is pregnant with an Rh-positive man, in 70% of cases the fetus will be Rh-positive. However, even with this combination, only 1.5% of pregnancies show an incompatibility reaction.
Rh immunization during pregnancy is the appearance of Rh antibodies in a pregnant woman in response to fetal red blood cells entering her bloodstream. Antibodies, passing through the placental barrier into the fetal bloodstream, destroy its red blood cells, causing hemolytic anemia and jaundice (due to an increase in the level of bilirubin, a pigment released after the breakdown of red blood cells).
During the first pregnancy there are usually no such problems. The immune system reacts slowly, so it simply does not have time to produce enough Rh antibodies to destroy the child’s red blood cells. But during the second and subsequent pregnancies, it is already ready to attack the blood cells of the fetus, so the likelihood of Rh conflict during a second pregnancy increases sharply.
Make an appointment

Antibody titer indicators in pregnant women:
Normally, there should be no antibodies to fetal red blood cells in the blood plasma.
If the antibody titer is 1:4 or more, then we can already talk about the beginning of the development of a Rh conflict situation.
If the antibody titer is 1:16 or higher, then this is already an indication for amniocentesis (examination of amniotic fluid).
In short, the higher the antibody titer level, the greater the risk of fetal hemolytic disease. The antibody titer may remain at the same level throughout pregnancy, or it may change abruptly. Therefore, regular monitoring is required.
Diagnosis of Rh conflict
A pregnant woman, as a rule, does not have any specific clinical symptoms when a Rh conflict occurs. In order to detect pathological changes in a timely manner, various non-invasive and invasive diagnostic studies are prescribed.
When managing a pregnancy with a risk of developing Rh conflict, it is suggested to determine the antibody titer in the woman’s blood plasma up to 32 weeks - monthly, from 32 to 35 weeks - once every two weeks, after 35 weeks - weekly.
The condition of the fetus is monitored using ultrasound. Starting from the 18th week of pregnancy, ultrasound is performed every month (if indicated, it can be done more often). With its help, you can see signs of Rh conflict: thickening of the placenta, increase in the diameter of the umbilical cord, enlargement of the heart, liver and spleen, double contour of the head, etc.
With Doppler and cardiotocography, it is possible to identify signs of fetal anemia associated with hemolytic disease.
If the antibody titer rapidly increases in dynamics or other non-invasive signs of fetal hemolytic disease are detected, invasive measures are taken to diagnose it.
According to indications, amniocentesis can be performed - sampling a small amount of amniotic fluid. They determine the level of bilirubin. The most common indications for amniocentesis are:
- antibody titer in the mother's blood is higher than 1:16;
- cases of Rh conflict in the anamnesis, which occurred with a severe form of hemolytic disease of the fetus.
Treatment of Rhesus conflict
There are two main areas of treatment that can improve the child’s condition. The first is a blood transfusion after birth or in utero. The second, early delivery, is the only method to stop the flow of maternal antibodies into the fetal blood and the destruction of red blood cells.
After birth, the baby often requires medical care in an intensive care unit.
A newborn may experience the following forms of hemolytic disease:
- anemic;
- icteric;
- edematous.
The mildest form is anemic, the most severe, characterized by a worse prognosis, is edematous. The higher the level of bilirubin in the blood, the more severe the damage to internal organs can be. The consequences of a severe form of hemolytic disease of newborns are often hearing loss or delayed intellectual development of the child.
Prevention of Rh conflict during pregnancy
If a woman has Rh negative blood, then during pregnancy, at 28 weeks, she is recommended to take preventive measures to avoid the development of Rh conflict. To do this, the woman will be asked to inject anti-Rhesus immunoglobulin D intramuscularly.
It will be able to prevent the formation of antibodies in her blood. Further, the determination of antibodies in the blood will no longer have clinical significance. If anti-Rhesus immunoglobulin was not administered at 28 weeks of pregnancy, it is necessary to continue to determine antibodies at the interval indicated above.
After the birth of an Rh-positive baby, in the first 72 hours, the postpartum mother should be given another injection of anti-Rhesus immunoglobulin in the maternity hospital. It is needed in order to reduce the risk of Rh conflict in subsequent pregnancies.
In addition, the administration of immunoglobulin to a Rh-negative woman during pregnancy is necessary in cases of possible entry of fetal red blood cells into her body.
These include:
- artificial termination of pregnancy or spontaneous miscarriage;
- ectopic pregnancy;
- hydatidiform mole;
- amniocentesis, chorionic villus biopsy, cordocentesis;
- bleeding from the uterus;
- closed abdominal injury to the mother (in a car accident);
- intrauterine fetal death.
IVF for Rhesus conflict
Pregnancy after In Vitro Fertilization proceeds in the same way as after conventional conception of a child through sexual intercourse. IVF is not prohibited if the woman has a negative Rh factor and the husband has a positive one. This fertilization technique can neither prevent Rh conflict nor increase its risk.
In order to prevent Rh conflict during IVF with donor sperm, a donor comparable to her Rh status is selected in advance for the patient. That is, if the patient has Rh-negative blood, then a donor will also be recommended for her with Rh-negative blood.
If you are monitoring your pregnancy at VitroClinic, our obstetrician-gynecologists will do everything possible to prevent the development of hemolytic disease of the fetus, which threatens not only the health of the child, but also his life. You will regularly undergo blood tests for antibodies and ultrasound diagnostics. In addition, there are prophylactic drugs to prevent immunization (anti-Rhesus immunoglobulin D).
Their timely administration helps prevent possible Rh conflict. If you had an Rh conflict in a previous pregnancy, then after IVF in our clinic everything possible will be done to prevent this from happening.
How to avoid problems
If incompatibility is detected, the doctor organizes several blood tests for the still pregnant woman to monitor the level of antibodies. After birth, the baby's blood is also tested. If the baby is “Rh+”, then the mother is offered an injection of anti-D (immunoglobulin) within a few days after birth. Anti-D prophylaxis is taking a drug that prevents a woman’s body from producing antibodies against Rh+ cells. Today, Rh sensitization during pregnancy and after childbirth can be largely prevented. This is achieved through prophylaxis with anti-D immunoglobulin.
All Rh-negative expectant mothers are offered anti-D immunoglobulin injections. This procedure prevents harm from Rh incompatibility
.
Typically, all pregnant women who are Rh-negative and do not have antibodies to the D antigen are recommended prophylaxis with anti-D immunoglobulin. This is either one injection between 28-30 weeks of pregnancy, or two - at 28-34 weeks. This kind of prevention is called ongoing prenatal (antenatal).
The process by which the mother's body begins to produce antibodies against antigen D is called potentially sensitizing. Sometimes, after such circumstances arise, additional injections of anti-D immunoglobulin are necessary. Such situations include the following:
- threatened miscarriage or miscarriage;
- ectopic (ectopic) pregnancy;
- abortion;
- vaginal bleeding;
- obstetric intervention;
- abdominal trauma, such as after a fall or car accident.
Any event, be it vaginal bleeding or abdominal trauma, should be reported to your midwife or doctor as soon as possible.
A timely consultation with your doctor is the right step towards a trouble-free pregnancy and the birth of a healthy baby.
What complications most often occur?
“Complicated childbirth” is a very specific medical and legal term. All possible situations in which it can be used are spelled out in a special document - Instructions of the Ministry of Health of the Russian Federation dated April 23, 1997 No. 01-97.
The word “complicated” does not always mean that something terrible will definitely happen during the birth of a child. For example, this term is used for multiple pregnancies. If a woman carries twins in her tummy, then her body experiences higher stress, and there is a higher chance that something will go wrong. Naturally, the doctors at the antenatal clinic pay more attention to such expectant mothers, and all necessary measures are taken in the delivery room. The premature birth of a baby is also actually a complication.
Ministry of Health document No. 01-97 lists the following situations and complications:
- Chronic diseases and various pathologies in the expectant mother: preeclampsia and eclampsia, serious kidney damage, pathologies of the cardiovascular system, lungs, high blood pressure, arrhythmias, complications associated with the formation of blood clots, cancer, liver damage, etc.
- The need for caesarean section and other obstetric operations.
- Significant blood loss during labor and postpartum anemia.
- Severe ruptures of the cervix, perineum, pubic symphysis (the joint between the pubic bones, which is located in the lower abdomen). The most severe complication is uterine rupture. During it, very heavy bleeding occurs, so doctors prescribe a cesarean section to all expectant mothers who are at high risk of this.
- Postpartum diseases: thrombophlebitis, endometritis (inflammation in the uterus), purulent mastitis (inflammation of the mammary gland), sepsis (“blood poisoning”), inflammation of the peritoneum and tissue in the pelvic area.
- The premature birth of a baby, its immaturity.
- In vitro fertilization (IVF), when an egg is artificially fertilized with a sperm in the laboratory, the embryo is cultured “in vitro”, and then transferred into the uterine cavity.
How important is compatibility?
Planning a pregnancy is a conscious step for future parents. The desire to have a child is inextricably linked with responsibility for the health and future of the baby. Therefore, many couples, before conception, undergo a number of medical examinations in order to eliminate risk factors for both the expectant mother and the child, including taking tests to find out about blood compatibility for conception. This examination is extremely important for the positive course of pregnancy throughout the entire period, the health and well-being of the child.
The essence of a blood group compatibility test before conception is that a couple's blood is taken to determine the Rh factor. The results of the analysis are assessed by a doctor, and the best answer for the couple will be that the Rh factors of their blood coincide, in which case the chances of safely carrying and giving birth to a healthy child are significantly increased.