Uterine polyps are local benign neoplasms growing from the endometrial mucosa. They look like tubercles located on a wide base, or round or oval formations on a thin stalk. There may be one or several of them in the uterine cavity; in the latter case they speak of polyposis. The size of polyps varies from a few millimeters to 8 or more centimeters.
- Signs of a polyp in the uterine cavity and their diagnosis
- When is polyp removal necessary?
- Methods for removing endometrial polyps
- What is hysteroscopy of the uterus for polyps
- Types of hysteroscopy
- Indications for hysteroscopy
- Features of the event
- Preparation
- Basic recovery recommendations
- Complications after polyp removal
- Contraindications
Signs of a polyp in the uterine cavity and their diagnosis
Often uterine polyps do not manifest themselves, but some patients have the following symptoms:
- Menorrhagia - heavy menstruation.
- Bleeding outside of menstruation.
- Spotting after sexual intercourse.
- Bleeding during menopause.
- Infertility and miscarriages.
- With large polyps, women may notice copious whitish discharge, discomfort and pain during intercourse, as well as periodic cramping pain in the lower abdomen.
To make a diagnosis, it is necessary to undergo a comprehensive examination, which includes the following procedures:
- Gynecological examination - particularly large polyps can be palpated during manual examination; cervical polyps can be detected during examination in the speculum.
- Ultrasound of the pelvis - in the uterus, growth of the endometrium with a local increase in its mucous layer is detected. The structure of this neoplasm is homogeneous.
- Separate diagnostic curettage followed by histological examination of the obtained material.
- Hysteroscopy - allows you to examine the endometrium from the inside, visualize single or multiple polyps and determine their location. The procedure is also therapeutic in nature, since it allows for the simultaneous removal of all identified tumors and their subsequent histological examination. This is the most effective method for diagnosing a polyp in the uterus.
What is this procedure?
Hysteroscopy is an examination of the uterine cavity using special equipment, which is also capable of performing some manipulations - such as removing endometrial polyps, submucosal myomatous node, monitoring possible remnants of the fertilized egg after an abortion, etc.
A gynecologist, examining the uterine cavity using a hysteroscope, can easily determine existing pathologies in an enlarged image displayed on the screen. Such an examination greatly simplifies the diagnosis. This procedure has proven its effectiveness in case of various menstrual cycle irregularities, with minor uterine bleeding and as an additional measure before complex surgical interventions on the uterus. However, hysteroscopy also has some contraindications, such as pregnancy, acute diseases of the genital organs, cervical cancer or stenosis, various infectious diseases (pyelonephritis, pneumonia, etc.), and excessive uterine bleeding.
When is polyp removal necessary?
The choice of patient management tactics and determination of the need to remove the polyp is determined individually. If a woman is of reproductive age and has no symptoms of a polyp, conservative management tactics can be chosen. In this case, the patient should undergo regular monitoring.
In all other cases, removal of polyps is indicated:
- Presence of symptoms of the disease.
- Pre- and postmenopausal periods, even if there are no symptoms.
Methods for removing endometrial polyps
Surgical removal of endometrial polyps is called polypectomy. It involves curettage of the endometrium followed by histological examination of the resulting material. Curettage can be performed blindly, under visual control using ultrasound or hysteroscopy. The latter method is the most preferable because it allows you to control the completeness of polyp removal and avoid the development of surgical complications (uterine perforation, excessive curettage with damage to the basal layer of the endometrium, etc.).

If treatment does not help, and the patient is in menopause, she may be offered surgery to remove the uterus in the following cases:
- Persistent relapses of multiple polyposis.
- High risk of malignancy of polyps.
- The presence of severe symptoms that significantly worsen a woman’s quality of life.
results
The study has high reliability and detects pathology in 63-97% of cases. The gynecologist examines the uterine cavity and identifies various changes; based on a visual examination, a diagnosis is made. Each disease has its own clinical picture:
- Hyperplasia . Thickened and folded endometrium, swelling. The color of the mucous membrane is pale pink with an abundance of transparent dots.
- Polypoid formations. Lumpy surface, presence of pits and bumps, up to 1.5 cm in diameter.
- Atypical hyperplasia . The presence of cysts and a large number of glandular ducts. Sometimes the formations are dull yellow or gray.
Even the color and shape of polyps have diagnostic value and help identify the disease.
The result of office-type hysteroscopy should be an accurate diagnosis. Histological analysis takes approximately 7 days. The result of the operation using a hysteroscope is the removal of pathology (neoplasms, endometrial layer).
Types of hysteroscopy
There are diagnostic or surgical hysteroscopy. Diagnostic involves only examining the endometrium and endocervix for the presence of pathologies. The study is performed on an outpatient basis and does not require serious anesthesia (local anesthesia and sedation are sufficient) and a long recovery period. Therefore, it was called office hysteroscopy. Based on its results, the doctor draws up a plan for further management of the patient.
Surgical hysteroscopy allows for diagnosis and immediate treatment of identified pathologies. It is performed in an operating room and requires full anesthesia. The procedure is prescribed either when the diagnosis has already been established, or when the likelihood of detecting a pathology is extremely high.
We specialize in surgical hysteroscopy because we believe that invasive diagnostic techniques can be successfully replaced by safer tests. This will help make the correct diagnosis without the risk of surgical complications.
Features of the event
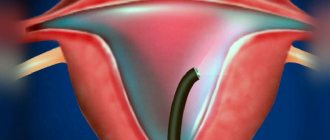
Therapeutic hysteroscopy is carried out on a hospital basis, including a one-day hospital in an operating room. An hour before the start of the intervention, premedication is performed - a sedative injection is given. After being delivered to the operating room, the patient is placed in a gynecological chair and given intravenous anesthesia. Next, proceed to the operation:
- Dilation of the cervical canal.
- A certain amount of sterile liquid is injected into the uterine cavity to “straighten” its walls.
- A hysteroscope is inserted through the cervical canal. As it is introduced, a step-by-step examination of all parts of the uterus is performed. First, the cervical canal is examined, then the uterine cavity and its angles.
- If necessary, surgical procedures are performed - taking a biopsy, removing polyps, dissecting synechiae, etc.
- At the end of the operation, fluid is removed from the uterine cavity.

What procedures can a gynecologist perform during hysteroscopy?
Hysteroscopy is a diagnostic procedure, however, during it some additional manipulations can be performed, including therapeutic ones:
- Biopsy is a procedure during which a piece of pathologically changed tissue is removed and sent to the laboratory for histological and cytological examination. This allows you to establish a more accurate diagnosis, confirm or exclude the presence of a malignant tumor in the uterus.
- Hysteroscopy allows you to remove various pathological formations protruding into the uterine cavity, such as polyps and fibroids.
- The source of bleeding can be eliminated using electrocoagulation and low temperature (cryosurgery).
- Place contraceptive devices in the fallopian tubes.
The Euroonko clinic in Moscow offers special comprehensive programs for women, for example, hysteroscopy with separate diagnostic curettage of the cervix and uterine body. The cost of the service includes a 6-hour stay in a comfortable hospital, meals, and all related procedures.
Preparation
Preparation for hysteroscopy is similar to other surgical interventions in gynecology. First, an examination and, if necessary, certain treatment are carried out. The following tests are performed:
- General blood and urine analysis.
- Coagulogram.
- Blood type and Rh factor.
- Vaginal smear for flora.
- ECG.
- Test for STIs.
- Tests for HIV and parenteral hepatitis.
Hysteroscopy is planned at the beginning of the menstrual cycle (before day 10), since endometrial tumors are clearly visible during this period.

Immediately before surgery, it is recommended to follow these rules:
- Two days before hysteroscopy, avoid sexual contact.
- On the day of the operation, take a shower and then put on underwear made from natural fabrics.
- Remove jewelry and contact lenses.
- Immediately before entering the operating room, empty your bladder.
- Do not eat for at least 6 hours before anesthesia.
How long does disability last for gynecological interventions?
The average length of sick leave after surgery is 10 days. The reduction of this period or its extension depends on the severity of the operation and the presence of associated complications. According to severity they are distinguished:
- Lungs - the patient is fully able to work and can start work the next day. BL is not issued. In some cases, a period of up to 3 days is provided.
- Moderate – it takes time to recover, some bodily functions are impaired. Duration of BL is up to 30-45 days.
- Severe – after the main stage of treatment, a long rehabilitation period is required. BL for more than 45 days.
Gynecological operations are classified as light and moderate surgical interventions . Conditions after removal of oncology are considered severe if, according to histology (examination of removed tissue), a malignant tumor is confirmed. In this case, the doctor refers the patient to medical examination, where a disability group is assigned.
A certificate of incapacity for work is not issued only for minor types of operations. They are usually performed on an outpatient basis, without hospitalization and do not involve complications. All cases are considered privately by the attending physician and the medical commission.
Basic recovery recommendations
- If an antibiotic is prescribed, take it for as long as your doctor recommends.
- To relieve pain after hysteroscopy, you can take antispasmodics or analgesics.
- Avoid sexual intercourse and heavy physical activity until the bleeding stops, but not less than 10 days.
- Perform hygiene measures in the shower. Taking a bath is not recommended.
- Toilet your genitals as needed, but at least 2 times a day.
- During the recovery period, it is not recommended to use tampons and menstrual cups; discharge should come out of the vagina freely.
Most women generally feel satisfactory after therapeutic hysteroscopy. The main complaints are nagging pain in the lower abdomen and weakness. The full recovery period takes about two weeks. However, if complications develop - fever, heavy bleeding, foul-smelling discharge, you should immediately consult a doctor.
What complications can hysteroscopy cause?
As with any invasive intervention, complications may develop after hysteroscopy. The most formidable and dangerous of them is perforation of the uterine wall, which is accompanied by bleeding. To eliminate the perforation, repeated surgery is required to suturing the defect. If left untreated, peritonitis may develop.
There may also be other complications:
- Hematometra is the accumulation of blood in the uterine cavity due to the impossibility of its drainage. Clinically manifested by increasing spasmodic pain in the lower abdomen and deterioration in general well-being. For treatment, conservative methods can be used (prescription of drugs that improve uterine contraction or antispasmodics for pathological contraction of the cervix), or surgical methods, in which repeated intervention is performed with evacuation of the intrauterine contents.
- Infectious complications. They are manifested by an increase in body temperature, symptoms of intoxication, and pain in the lower abdomen. A little later, pathological discharge appears, which may have a foul odor.
- Bleeding. Possible after therapeutic hysteroscopy, when, for example, myomatous nodes or polyps are removed. If you experience heavy bleeding, especially if it lasts several days, you should consult your doctor.
In general, hysteroscopy is a low-traumatic intervention and the likelihood of complications after it is much lower than with other, more extensive treatment methods.
Complications after polyp removal
As after any gynecological operation, the following complications may develop after hysteroscopy:
- Damage to the wall or cervix - treatment may require additional surgery to close the perforation.
- Damage to the cervix - may require stitches.
- Bleeding.
- Infectious complications.
It should be noted that complications after hysteroscopy are much less common than after other gynecological interventions performed “blindly”. But the possibility of their development cannot be completely excluded.
Menstruation after hysteroscopy: likelihood of irregularities
Not all types of procedures change menstrual function. Menstruation after hysteroscopy should come on time or recover within 30 days, although it all depends on the reactivity and individual characteristics of each woman.
Diagnostic hysteroscopy does not violate the integrity of the endometrium, so menstruation comes at the right time. Menstruation after surgical hysteroscopy depends on the degree of intervention. A biopsy, removal of one or two polyps, synechiae and other small formations cause minor damage to the endometrium, which can lead to minor disruptions, although not always. But if it is necessary to remove most of the endometrium or the entire layer, then menstruation after hysteroscopy may change its character.
The reason why the surgical procedure was performed also affects the woman’s condition: if the diagnosis causes a hormonal imbalance in the patient, then menstruation after hysteroscopy is highly likely to change.
Contraindications
- The presence of decompensated chronic diseases that may interfere with anesthesia, for example, cardiovascular pathology.
- Presence of STIs and vulvovaginitis.
- The presence of diseases accompanied by a tendency to bleeding.
Euroonco specialists closely monitor the condition of patients not only in the postoperative period, but also at the initial stage. In this regard, we perform the procedure only after we are convinced that the patient has no contraindications. You can make an appointment for a consultation about uterine polyps by calling:
Book a consultation 24 hours a day
+7+7+78