Urogenital chlamydial infection (urogenital chlamydia) is the most common sexually transmitted infection (STI). According to the World Health Organization (WHO), about 90 million new cases of chlamydial infection are registered annually in the world. And, apparently, this is just the “tip of the iceberg.”
The causative agent of urogenital chlamydia is Chlamydia trachomatis , an intracellular parasite close to gram-negative bacteria, but, unlike bacteria, they have lost the ability to produce metabolic energy. This determines their intracellular growth. Belongs to the Chlamydiaceae family.
The source of infection is a person with an acute or chronic form of urogenital chlamydial infection (both with clinical manifestations and asymptomatic).
The main routes of transmission of chlamydial infection:
- Sexual;
- Vertical (infection of the fetus from the mother in utero or during the passage of an infected birth canal).
Susceptibility to urogenital chlamydial infection ranges from 60 to 100%, and is especially high in immunodeficiency of any origin.
Urogenital chlamydial infection predominantly affects the sexually active part of the population (age 17-25 years). Among sexually active, clinically healthy women, chlamydia infection is, according to various sources, 8-40% (on average about 15%), among men - approximately 10%. The number of mixed infections caused by a combination of several microorganisms (gonococci, trichomonas, ureaplasma, mycoplasma, etc.) is also increasing.
Urogenital chlamydia is characterized by a long asymptomatic course, which leads to widespread infection. Since the carrier of the causative agent of chlamydial infection does not suspect anything for a long time and passes it on to sexual partners. The development of pronounced clinical manifestations of chlamydial infection often occurs already at the stage of complications. This leads to late diagnosis and long-term, not always successful treatment.
Possible complications of chlamydia when spreading beyond the urogenital tract include:
- chlamydial conjunctivitis;
- chlamydial pharyngitis;
- chlamydial hepatitis;
- Reiter's disease is the most severe complication of chlamydia. It occurs in people with a genetic predisposition and is manifested by a triad of clinical manifestations - arthritis, urethritis and conjunctivitis. Men get sick 20 times more often than women.
Urogenital chlamydia in women
Uncomplicated urogenital chlamydia in women occurs in the form of mucopurulent cervicitis - inflammation of the cervix.
Symptoms of chlamydia in women: tingling, itching or burning when urinating, pain in the lower abdomen and groin area, slight vaginal discharge between menstruation or during sexual intercourse, slight bleeding from the genital tract, conjunctivitis. The temperature may rise to subfebrile levels. Symptoms are generally nonspecific and laboratory testing (chlamydia testing) is required to make a diagnosis. In addition, up to 75% of cases of chlamydia in women are asymptomatic and manifest themselves already at the stage of complications.
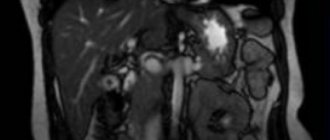
Chlamydia can also affect other organs, spreading upward - “ascending” chlamydia - and leads to pelvic inflammatory diseases (PID): endometritis, salpingitis, salpingo-oophoritis, perihepatitis (Fitz-Hugh-Curtis syndrome), urethritis, cervicitis, proctitis.
In turn, PID often causes serious reproductive dysfunction. Women with a history of PID have a 7-10-fold risk of developing an ectopic pregnancy. In 40% of such women, pregnancy in the future is impossible, and in 60% of women who become pregnant again, an ectopic pregnancy develops again in 12% of cases, and spontaneous abortion in 15-20% of cases.
In approximately 50% of women suffering from infertility, the causative factor is chlamydial infection.
Analysis for chlamydia during pregnancy: with chlamydia in women during early pregnancy, the formation of infectious embryopathies, which are manifested by congenital malformations of the fetus and primary placental insufficiency, is possible. This often ends in a non-developing pregnancy or spontaneous miscarriage.
During pregnancy at a later stage, secondary placental insufficiency, impaired production of amniotic fluid (amniotic fluid), and premature birth may develop.
Detailed description of the study
Detection of chlamydia DNA in scrapings from the urogenital tract using polymerase chain reaction.
Chlamydia (Chlamydia trachomatis) is one of the causative agents of sexually transmitted diseases (STDs). They are tiny bacteria that tend to penetrate the epithelial cells of the genitourinary system and multiply in them, thus hiding from the human immune system. As a result, chlamydia infection can be asymptomatic for a long time.
Infection occurs mainly through sexual intercourse during any form of sexual intercourse in the absence of barrier contraception. In addition, transmission of infection from mother to child during childbirth is possible.
In the life cycle of chlamydia, it is customary to distinguish two main forms of existence: the so-called elementary bodies and reticular bodies. The former are an extracellular form, the latter - intracellular, or vegetative. Some scientific works have noted the existence of a third variety of these bacteria - aberrant bodies, due to which, according to scientists, the pathogen can remain in the body in a latent form for a long time. Due to the fact that chlamydia can only reproduce inside a human cell.
When the immune defense is suppressed due to severe chronic diseases, stressful situations, hormonal imbalance, and also during pregnancy, an infected person develops chlamydia.
In men, its clinical manifestation is mainly inflammation of the urinary tract - urethritis. Its symptoms include pain and burning when urinating, copious discharge from the penis. Less commonly, chlamydia causes inflammation of the testicles and their appendages.
For women, infection with chlamydia can have more negative consequences. In addition to affecting the urethra and vagina, Chlamydia trachomatis penetrates the uterus and fallopian tubes, into the pelvic organs, including the rectum. As a result, a complex of symptoms develops, referred to as pelvic inflammatory diseases. Women turn to a gynecologist and other specialists about pain in the lower abdomen, menstrual dysfunction, inflammation of the rectum and many other complaints. However, one of the most unfavorable outcomes of this disease is the occurrence of adhesions inside the organs, as well as in the pelvis, which prevent pregnancy.
If chlamydia infection occurs during pregnancy, there may be an increased risk of premature birth, fetal pathologies, and postpartum complications in the mother.
There are varieties (serotypes) of chlamydia that affect the organs of vision, which is especially dangerous for newborns. These same serotypes are responsible for pneumonia in a newborn child.
Identification and treatment of chlamydia is carried out by a dermatovenerologist. Modern diagnosis of Chlamydia trachomatis is carried out by taking a smear from the urogenital tract, followed by analysis of the presence of genetic material of bacteria in the sample.
Urogenital chlamydia in men
In 25-30% of cases, chlamydia in men occurs with unexpressed clinical manifestations and remains unrecognized for a long time.
Uncomplicated chlamydial infection occurs in men most often in the form of urethritis - inflammation of the urethra.
Symptoms of chlamydia in men: itching or burning during urination, pain in the scrotum, redness around the external opening of the urethra, slight bleeding during ejaculation or at the end of urination, conjunctivitis. The temperature may rise to subfebrile levels. Symptoms are generally nonspecific and laboratory testing (test for chlamydia) is necessary to make a diagnosis.
The most common complication of urogenital chlamydia in men is epididymitis (inflammation of the epididymis). Epididymitis can lead to the development of infertility due to damage to the tissue of the spermatic cord or suppression of normal testicular secretion due to autoimmune processes.
Diagnostics.
Due to the high likelihood of complications, screening for chlamydia and other STIs is recommended:
• Sexually active women aged 25 years or younger . The incidence of chlamydial infection is highest in this group, so an annual screening test is recommended. Even if you have been tested recently, get tested again if you have a new sexual partner.
• Pregnant women . Should be tested for chlamydia during the first prenatal examination. In case of a high risk of infection (when changing sexual partners or when a regular partner is infected), testing must be repeated.
• Women and men at high risk of infection . Frequent screening for chlamydia is recommended if you have multiple sexual partners or unprotected sex (oral, vaginal or anal). And also in case of infection with another STI or the presence of one in a sexual partner.
Screening and diagnosing chlamydia is relatively simple. Tests include:
• Analysis of urine. A laboratory urine test can reveal the presence of this infection.
• Smear. The doctor takes a smear of cervical discharge for culture or for chlamydia antigens. This can be done during a regular Pap test (with a PAP test, the doctor removes a sample of cells from the cervix using a small, cone-shaped brush and a tiny spatula. The doctor then rinses the brush and spatula in a vial filled with a special liquid and sends the vial to a laboratory for analysis).
For men, the doctor inserts a thin tip into the urethral canal of the penis to obtain a sample from the urethra. In some cases, a smear is also taken from the anus.
After recovery from the initial chlamydial infection, it is necessary to undergo a follow-up examination after three months.
Laboratory diagnosis of chlamydial infection
Early detection of chlamydial infection makes it possible not only to prevent its further spread and transmission to offspring, but also to significantly reduce the risk of complications leading to reproductive dysfunction.
Indications for testing for chlamydia:
- preventive examination;
- presence of characteristic complaints;
- pregnancy planning;
- examination of pregnant women;
- complicated obstetric and gynecological history;
- suspicion of urogenital chlamydia;
- before surgical interventions on the genitals and pelvic organs;
- suspected conjunctivitis or arthritis of chlamydial etiology.
Treatment.
Chlamydia trachomatis infection is treated with certain types of antibiotics. You may receive a single dose, or you may need to take the medication daily or several times a day for five to ten days.
In most cases, the infection clears up within one to two weeks. During this time, you must abstain from sex. In addition, simultaneous treatment of the sexual partner or partners is mandatory, even if they do not show signs of infection or severe symptoms. Otherwise, the infection may return from an untreated sexual partner.
Having had chlamydia does not develop immunity against re-infection in the future.
PCR analysis for chlamydia
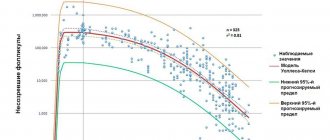
In diagnosing chlamydia, of all existing methods, the polymerase chain reaction (PCR) method is recognized as the most reliable.*
Advantages of PCR diagnostics for chlamydia:
- Direct determination of chlamydia in biomaterial . PCR is a molecular biological method that is aimed at identifying DNA fragments specific to chlamydia and directly indicating the presence of infection
- High specificity . In the biomaterial subjected to analysis, the genetic material of chlamydia is detected - a DNA fragment. It is specific and not the same among DNA-containing organisms.
- High sensitivity. To perform PCR analysis, the presence of single chlamydia cells in the biomaterial is sufficient. The sensitivity of PCR analysis is 10-100 cells in a biomaterial, when other tests have 103-105 cells (microscopic, bacteriological methods). These methods do not allow identifying the pathogen in 20-40% of infected individuals, while the PCR method allows identifying chlamydia in 98-100% of patients.
- The versatility of the PCR method. Along with the detection of chlamydia DNA in the biomaterial under study, the PCR method allows the simultaneous detection of several pathogens, for example, Trichomonas, gonococci, etc.
- Speed of obtaining results. PCR analysis is fully automated, which allows you to obtain results in a short time, from 1 to 3 calendar days.
- Diagnosis of latent and sluggish forms of chlamydia. The PCR method can detect chlamydia, even if it is asymptomatic.
To test for urogenital chlamydia using the PCR method, you can submit: scrapings from the urethra, urine, prostate secretions in men, scrapings from the cervical canal, vagina in women.
For diagnostic activities, we use reagent kits from the Federal Budgetary Institution Central Research Institute of Epidemiology of Rospotrebnadzor, which have an EU certificate of conformity and are used not only in our country, but also abroad.
How to prepare for a urethral smear (for infection, flora, PCR)
To examine a smear, material is taken directly from the urethra. To do this, a special instrument is carefully inserted into it a few centimeters, after which a couple of rotational movements are made and the taken material is applied to a glass slide. In the future, it can be used for various studies, including the study of flora, PCR and ELISA.
Preparation for a urethral smear in men is as follows:
- A week before the procedure, stop taking antibiotics.
- Avoid intimacy for 1-2 days before the procedure.
- Take a shower the night before.
- Give up alcohol in 1-2 days.
- In the morning before taking a smear, do not urinate for at least 2-3 hours, since urine washes away the flora from the mucous membrane.
- Do not use antiseptics for toileting the genitals during the day before the test.
Since the taken material can be used for various studies, you can prepare for them according to the listed rules. They will act to prepare men for a smear for flora, for PCR from the urethra.
Diagnosis of chlamydial infection in CMD
- Chlamydia, qualitative DNA determination, PCR
- Chlamydia, DNA quantification, PCR
- Chlamydia, qualitative determination of ribosomal RNA using the NASBA method
- Chlamydia, semi-quantitative determination of IgG antibodies, ELISA
- Chlamydia, semi-quantitative determination of IgA antibodies, ELISA
- Chlamydia, qualitative determination of IgM class antibodies, ELISA
Considering the high frequency of mixed infections, in addition to testing for chlamydia, it is advisable to use a wider range of studies, and in women, a mandatory determination of the quantitative ratio of vaginal microflora:
- Comprehensive STI research, DNA quantification, PCR
- Urogenital infections in men, DNA quantification, PCR
- Urogenital infections in women, DNA quantification, PCR
- Florocenosis
- Florocenosis and Microscopy
- Florocenosis and NCMT
- Florocenosis and NCMT and Microscopy
For the best choice of tests, consult your doctor.
*Federal clinical guidelines. Skin diseases. Sexually transmitted infections. 2021
References
- https://www.cdc.gov/std/russian/stdfact-chlamydia-russian.htm
- Federal clinical guidelines. diagnosis and treatment of diseases accompanied by pathological discharge from the female genital tract. Ed. Prilepskoy V.N. M.: 2013.
- Manzenyuk I. N., Vorobyova M. S. Chlamydiatrachomatis. Modern ideas about the pathogen. Serodiagnosis. State Research Institute for Standardization and Control of Medical Immunobiological Preparations named after. L. A. Tarasevich. 2021.
What do the test results mean?
“Not detected” - a negative result indicates the absence of antibodies to chlamydia in the blood.
“Doubtful result” - low number of antibodies, in the so-called “gray zone”. It can be detected both at the onset of the disease and can be an individual feature of the body. In case of such a result, the study should be repeated after 2-3 weeks. In case of illness, antibodies will grow and will be detected in a repeat study.
“Detected” indicates the presence of antibodies to chlamydia of the IgG class, which can be a sign of both current and past disease.
Preparing for a visit to the clinic.
If you think that you have a hidden sexually transmitted infection, make an appointment with a venereologist at our clinic for a comprehensive examination and consultation on treatment.
What should be done:
Before your visit, be prepared to answer the following questions:
• When did you first start having symptoms?
• What can strengthen or weaken them?
• What medications or supplements do you take regularly?
You can also make a list of questions to ask your doctor. For example:
• Should I be tested for other sexually transmitted infections?
• Should my partner be tested or treated for chlamydia infection?
• Should I abstain from sexual activity during treatment and for how long?
• How can I prevent chlamydia infection in the future?
What to expect from a doctor?
Your doctor will likely ask you a number of questions, such as:
• Do you have a new sexual partner or several partners?
• Do you always use condoms?
• Do you have pain in the pelvic area?
• Do you experience painful urination?
• Do you have any unusual genital discharge?