09/19/2017 Olga Migunova 0 comments
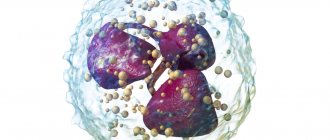
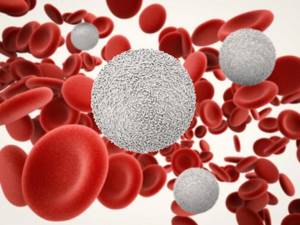
Monocytes are a type of white blood cells (leukocytes) that are responsible for protecting the human body from tumor cells and pathogenic microorganisms, as well as for the resorption and elimination of dead tissue. Thus, these cells cleanse the body, which is why they are also called “janitors”.
The clinical significance of monocytes in a blood test is that their level can suggest the presence of a particular disease. Experts recommend that both adults and children undergo a general blood test twice a year for prevention in order to promptly identify deviations from the norm.
Today we want to tell you why a child may have elevated monocytes and who to contact in this case.
Functions of monocytes in the body
In the medical literature you can also find other names for monocytes, for example, mononuclear phagocytes, macrophages or histiocytes.
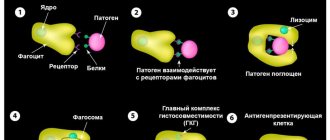
Macrophages are one of the main immune cells. Their role for the body is to fight pathogenic microorganisms (viruses, bacteria, fungi), waste products of microbes, dead cells, toxic substances and cancer cells.
Macrophages remain working in the pathological focus even after neutralizing the foreign agent in order to process dead pathogenic microorganisms and decayed tissues of the body, due to which they are called “orderlies”, “cleaners” or “janitors” of the body.
In addition, macrophages prepare the body for recovery by enclosing the lesion with a “wall” that prevents the spread of infection to intact tissues.
Average cost of analysis in Russia
A general clinical blood test with calculation of the leukocyte formula can be done free of charge under the compulsory medical insurance policy at your medical organization.
You can also get tested for a fee. On average, a general clinical blood test along with a leukocyte count will cost between 400 and 600 rubles. You can only request a white blood cell count. Such a study will cost 250–350 rubles.
I would recommend examining the level of leukocytes along with a general clinical blood test. The indicators together help to choose the right direction for further diagnostic measures.
The norm of monocytes in the blood of children: table
In most cases, the relative number of monocytes in the blood is determined, that is, the number of a given type of leukocyte is indicated as a percentage (%) in relation to other types of white blood cells.
| Child's age | Monocyte count, % |
| from 0 to 28 days | from 3 to 12 |
| from 1 month to a year | from 4 to 10 |
| from 1 to 15 years | from 3 to 9 |
| teenagers | from 1 to 8 |
As you can see, the levels of monocytes in the blood change with the age of the child.
Also, the doctor who ordered a general blood test may require the laboratory technician to provide the absolute number of monocytes, which also depends on the age of the child.
| Child's age | Monocyte count, g/l |
| up to 12 months | from 0.05 to 1.1 |
| 1-2 years | from 0.05 to 0.6 |
| 3-4 years | from 0.05 to 0.5 |
| Over 4 years old | from 0.05 to 0.4 |
What to do if deviations from the norm are detected?
First of all, don’t panic or get upset. It is worth showing your test results to a competent doctor.
A hematologist specializes in blood tests and more. He will be able to answer all your questions, give competent advice, and prescribe a proper examination of the body.
To further examine and search for the true causes of abnormal monocyte levels, specialists resort to various studies: from X-ray examination to studying the material obtained after bone marrow puncture. The main thing is to promptly identify breakdowns that have occurred in the body (both in adults and children) and prescribe adequate treatment.
Level of monocytes in the blood: how to determine?
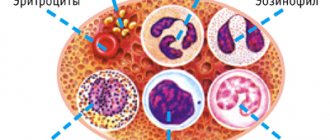
The content of monocytes in the blood is determined using a general blood test. This study allows you to count the total number of all white blood cells and calculate the leukocyte formula.

The leukocyte formula is the percentage of individual types of white blood cells, such as neutrophils, basophils, lymphocytes, monocytes and eosinophils. Changes in the leukocyte formula are markers of various diseases.
Blood for analysis is taken from a child’s toe or heel, depending on his age, and in rare cases, from a vein.
Benchmark analysis
As therapy progresses (whatever it may be), it is imperative that the child undergo a control blood test until all values return to normal, and then for prevention at least once more after six months. Immunity is the most valuable thing for a person from all that nature has endowed him with, and in no case should you joke with it.
How to prepare for a general blood test?
The well-known television pediatrician Komarovsky focuses in his program on a general blood test on the fact that the objectivity of the results depends on the correct preparation for the study, so it is important to observe the following principles:
- blood is donated exclusively on an empty stomach, since after eating the white blood cells in the blood increase. If a blood test is performed on an infant, the interval between the last feeding and the blood draw should be at least two hours;
- the day before blood sampling, the child must be ensured calm and protected from stress, as well as from physical activity and active games;
- It is not recommended to give your child fatty foods on the eve of a blood test;
- If the child is taking any medications, this should be reported to the doctor who referred him for a blood test, since some drugs can provoke monocytosis.
Treatment
As is already clear, no one treats low monocytes. Therapy should not be aimed at increasing the volume of these particles, but at eliminating the reason why the baby’s body does not resist the external threat as it should. If this cause is an independent diagnosis (the development of sepsis, leukemia, etc.), then a reduced level of this element will help to identify it in time and, thus, the treatment will be successful.
When it comes to the consequences of something that arose earlier, the doctor’s task should be aimed at helping the patient return to normal as quickly as possible. Sometimes for this it is enough just to prescribe the right diet along with general recommendations for adjusting your lifestyle. In more difficult situations, drug therapy may be required (or, conversely, urgent withdrawal of medications that were previously prescribed), and sometimes surgical intervention is necessary.
What is monocytosis?
Monocytosis is an increase in the level of monocytes in the blood, which can be determined by a general blood test.
Monocytosis is not a separate nosological form, but a symptom of many diseases.
Elevated monocytes in a child, depending on the reasons, can be accompanied by a variety of symptoms, namely:
- general weakness;
- fast fatiguability;
- increased body temperature;
- cough;
- nasal congestion;
- swollen lymph nodes;
- stomach ache;
- nausea and others.
It is customary to distinguish between absolute and relative monocytosis.
Absolute monocytosis is diagnosed when there is o.
With relative monocytosis, there is an increase in the percentage of monocytes against the background of a normal number of leukocytes due to a decrease in the number of other types of white blood cells.
Consequences of relegation
Monocytes in a child’s body perform a variety of functions and their reduction is fraught with certain cavities:
- Weak fight against pathogenic bacteria.
- Insufficient regulation of the immune response and inflammatory reactions.
- Insufficient control over the restoration of damaged tissue.
- Weak antitumor effect.
- Dysregulation of bone marrow functions to produce all blood cells.
- Poor digestion of defective cells.
Elevated monocytes in a child’s blood: reasons
The following diseases can lead to an increase in monocytes in children:
- Infectious mononucleosis;
- brucellosis;
- malaria;
- toxoplasmosis;
- roundworm infestation;
- syphilis;
- lymphoma;
- leukemia;
- rheumatoid arthritis;
- systemic lupus erythematosus;
- inflammation of the mucous membrane of the digestive tract (gastritis, enteritis, colitis and others);
- intoxication with phosphorus or tetrachloroethane.
Monocytosis can also be detected in children who have had an infectious disease, removal of tonsils, adenoids, as well as during the period of teething and changing teeth.
Carrying out diagnostics

In some cases, monocytosis syndrome in children is detected completely by accident. This usually happens during hospital treatment with regular tests for a completely different reason.
If the examination is carried out for the presence of monocytosis, then it is necessary to properly prepare for the tests. The baby should be protected from increased physical activity. Taking medications is also not recommended.
If these factors are excluded, the test results will be more accurate.
Monocytes are elevated in a child: examples of interpretation of the results of a general blood test
Of clinical significance is not only the increased content of monocytes in the blood, but also the combination of monocytosis with deviations of other hematological parameters. Let's look at examples.

- Lymphocytes and monocytes are increased. The combination of lymphocytosis and monocytosis can often be observed in children with acute viral infections, childhood infectious diseases and indicates the viability of the immune system. In cases where, against the background of elevated monocytes, lymphocytes are reduced, a weakening of the immune system can be assumed, since these cells are responsible for cellular immunity.
- Monocytosis and eosinophils are increased. This combination of indicators is characteristic of pathological processes of an allergic and parasitic nature. Monocytosis and eosinophilia can be detected in the blood of children suffering from atopic dermatitis, hay fever, bronchial asthma, ascariasis, giardiasis, etc. In rare cases, such changes can occur as a result of more serious diseases such as leukemia and lymphoma.
- Basophils and monocytes are increased. The main role of basophilic leukocytes is the destruction of foreign agents (viruses, bacteria, fungi), and this type of cell is the first to migrate in areas of inflammation. Basophils and monocytes can simultaneously increase in diseases of allergic or autoimmune origin.
- An increase in monocytes in a child against the background of high neutrophils. This combination is quite common and occurs in diseases caused by various bacteria and sometimes fungi. Also in such cases, lymphopenia is often observed.
- Increased monocyte count and high ESR (erythrocyte sedimentation rate) . Erythrocytes, or red blood cells, are cells that carry oxygen on their surface from the lungs to organs and tissues. Various infectious, allergic or autoimmune diseases affect erythrocyte sedimentation, in most cases accelerating it.
Monocytosis in children
An increase in monocytes in childhood is also often associated with infectious pathologies, mainly of a viral nature. If monocytosis is diagnosed based on a blood test, this means that the body is actively fighting disease-causing processes.
Also, a similar condition is observed with helminthic lesions - enterobiasis, ascariasis and others. After the destruction of helminths, the content of monocytes returns to normal. The cause may also be associated with tuberculosis, but such pathologies are rare. Monocytosis can be observed due to oncological processes. The most common are leukemia and lymphogranulomatosis.
Other common reasons:
- poisoning;
- allergic reactions;
- inflammation in the gastrointestinal tract;
- autoimmune pathologies;
- rheumatoid type arthritis;
- Crohn's disease;
- infections due to surgical interventions.