Complexes with this research
Future dad Comprehensive examination to prepare a couple for conception 5,600 RUR Composition
Entry into IVF Examination when a woman enters the IVF procedure 15,090 RUR Composition
Preparation for IVF for a man Examination to prepare a man for the IVF procedure RUR 4,010 Composition
IN OTHER COMPLEXES
- Examination during pregnancy. 1st trimester 10,260 RUR
- Pregnancy planning. Clinical indicators RUB 3,890
- Expanded hospital complex 4,390 RUR
1.Blood group analysis
Blood group test
and Rh factor is one of the most common blood tests. It can be performed for various reasons: before a blood transfusion, organ transplant, or surgery. A person’s blood type depends on special indicators, antigens, on the surface of red blood cells.
AB0 system
The AB0 system is a letter nomenclature of blood groups: 0 (first group), A (second group), B (third group), AB (fourth group).
The AB0 system allows blood to be divided into four groups as follows.
- If you have neither antigen A nor antigen B, then you have blood type O;
- If you have antigen A, then you have blood type II;
- If you have antigen B, then you have blood type 3;
- If you have both antigen A and antigen B, then you have blood type IV. This is the rarest blood type.
Not all blood types are compatible due to antigens.
For example, the first negative blood group is universal donor, because it has no antigens. While the fourth positive, rare blood group is only suitable for transfusion to people with a fourth positive blood group.
Detailed description of the study
The formed elements of human blood - red blood cells - may have some markers on their surface, called antigens.
There are two main such antigens - A and B. Based on their presence, 4 blood groups are distinguished: O(I) - absence of antigens A and B on the surface of the cell A(II) - antigen A is present on the surface of the erythrocyte B(III) - present on the surface of the erythrocyte antigen B AB (IV) - both antigens are found on the surface of the erythrocyte
These antigens have no physiological role, but determine the compatibility of blood during transfusion. When incompatible blood is transfused, an immune reaction of rejection of the foreign protein develops, which leads to the destruction of red blood cells - hemolysis.
Another marker of blood compatibility during transfusion is the Rh factor. This is a protein that is produced in 85% of Caucasians and 99% of people of the Mongoloid race. It is present on the surface of red blood cells, but does not play a significant role in the life of the body.
When blood containing the Rh factor enters the bloodstream of a person who does not have this protein on the surface of red blood cells, the human immune system perceives it as foreign. As a result, hemolysis develops. Therefore, blood transfusion requires taking into account compatibility not only by blood group, but also by the Rh factor.
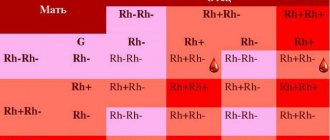
It is especially important to know your Rh status for women planning a pregnancy. If a woman with no Rh factor becomes pregnant with an Rh positive man, there is a chance that the child will also have an Rh factor.
In such a case, antibodies to the Rh factor may appear in the mother, which will cause hemolysis of the fetus, which is called Rh conflict. The formation of these antibodies can occur when fetal blood enters the mother's bloodstream. Factors that increase the risk of Rh conflict are:
- Complications of a previous pregnancy in the early stages (ectopic pregnancy or its termination);
- Abdominal injury during pregnancy;
- Vaginal bleeding during pregnancy;
- Medical interventions during pregnancy that require the removal of cells or fluid from the amniotic sac, such as amniocentesis and chorionic villus sampling.
With increasing gestational age, the risk of developing Rh conflict increases. Its appearance in the first trimester leads to missed pregnancy and its early loss; in the case of late Rh conflict, premature birth is possible. The newborn has hemolytic jaundice, which is accompanied by damage to internal organs and requires treatment.
It is important that antibodies to the Rh factor take time to form. Often the first pregnancy with Rh conflict proceeds favorably, since the immune system is just beginning to produce antibodies. The risk of complications in the second and subsequent pregnancies is much higher.
Studying your blood group and Rh factor helps you avoid complications associated with blood transfusions. With regard to the Rh factor, its determination is also important for assessing the risk of Rh conflict during pregnancy.
Determination of the main groups according to the AB0 system and the D antigen of the Rhesus system (Rhesus factor)
A comprehensive study that allows you to assess whether a patient’s blood belongs to one of the groups according to the ABO system and determine the presence/absence of the Rh antigen.The ABO system is the main blood compatibility system. It is represented by agglutinogens A and B, which are glycoproteins located on the surface of red blood cells, and agglutinins alpha and beta, which belong to the class of IgM immunoglobulins and circulate in the blood plasma. Depending on the combination of these agglutinogens and agglutinins, 4 blood groups are distinguished according to the ABO system.
The first (I) blood group (the most common in the European population, 42% of the population) is also called O-group, in which agglutinogens A or B are absent on the surface of red blood cells, agglutinins alpha and beta are detected in the plasma.
The second (II) blood group (37%) is also called A-group; agglutinogen A is present on the surface of red blood cells; agglutinin beta is detected in the plasma.
The third (III) blood group (13% of the population) is also called B-blood group; agglutinogen B is present on the surface of red blood cells; agglutinin alpha is detected in the plasma.
The fourth (IV) blood group (the rarest, only 8% of the population) is also called AB blood group; agglutinogens of both types A and B are present on the surface of red blood cells; agglutinins alpha and beta are absent in the plasma.
The Rh system also consists of several antigens, the main one of which is called antigen D, or Rh factor. In approximately 85% of people, the Rh factor (Rh-positive blood) can be detected on the surface of red blood cells. The belonging of a person’s blood to a certain group according to the ABO system and the Rh system is genetically determined and does not change throughout life.
Determining the blood group and Rh factor is of greatest importance when preparing for blood transfusion. Such a need may arise in case of severe blood loss, severe forms of hemolytic anemia, bone marrow diseases with disruption of normal red blood cell production, as well as during major surgical operations. The blood group according to the ABO system and the Rh system is taken into account not only when transfusing red blood cells, but also when transfusing other blood components (platelet mass, leukocyte suspension, etc.). Blood group determination is a mandatory test during pregnancy. In this case, data on the patient’s blood group and, in some cases, on the blood group of the child’s father are taken into account for timely diagnosis and treatment of an immunological conflict (caused by the incompatibility of the blood of the fetus and mother) and the resulting hemolysis of fetal red blood cells. Military personnel, soldiers of the Ministry of Emergency Situations and other law enforcement agencies are also subject to mandatory examination for blood type and Rh factor.
Since the laboratory method for determining blood groups is based on the agglutination reaction, the presence in the patient’s serum of specific proteins (M-protein, cold antibodies) or some bacteria that interfere with this reaction can lead to false-positive or false-negative results. Also, taking certain medications may affect the results of determining the Rh factor. Therefore, special attention should be paid to preparing for the test.
Rh (Rh) is one of the most important systems of erythrocyte antigens (along with the AB0 system), clinically significant not only for safe blood transfusion, but also during pregnancy management (when assessing the possibility of a Rh conflict and the risk of developing hemolytic disease of the fetus and newborn).
The RhD antigen is the most immunogenic (i.e., capable of causing an immune response (formation of antibodies) in individuals who do not have this antigen) of the Rh system antigens; its presence on the surface of erythrocytes determines Rh-positive status. The presence of this structural protein of the red blood cell membrane is a genetically inherited trait. The RhD antigen contains structural units called epitopes (currently 36 structural units have been identified). Rh-negative patients develop an immune response, accompanied by the production of anti-Rh antibodies, when they are transfused with Rh-positive blood. The presence of anti-Rh antibodies leads to the destruction of red blood cells carrying the Rh antigen and to severe post-transfusion reactions during repeated transfusions of Rh-positive blood into Rh-negative recipients. A similar immune response can develop in an Rh-negative woman during pregnancy with an Rh-positive fetus. Despite the fact that usually during pregnancy the fetal blood does not mix with the mother’s blood, in some situations (not the first pregnancy, pathological conditions associated with changes in placental permeability, sensitization after a previous transfusion of Rh-positive blood) the mother’s immune system produces antibodies to fetal erythrocyte antigens. Antibodies destroy Rh-positive red blood cells, which leads to various clinical manifestations (early fetal loss, chronic miscarriage) and hemolytic disease of the fetus and newborns. Pregnant women who are Rh positive do not have problems with Rh compatibility with the child. Assessment of Rh status during pregnancy or preparation for pregnancy, as well as monitoring the presence of alloimmune anti-erythrocyte antibodies, including antibodies to the RhD antigen, are important for the proper management of pregnancy in Rh-negative women. The risk of developing hemolytic disease of the fetus and newborn during repeated pregnancies can be prevented by timely administration of Rh-immunoglobulin.
Rh factor inheritance:
An individual's genotype consists of two inherited haplotypes: one from the father, the other from the mother. Each haplotype can determine the presence of an antigenic determinant (D) or its absence (d). The presence of an antigenic determinant is dominant, therefore:
| DD | Rh - positive |
| Dd | Rh - positive |
| dd | rh - negative |
Thus, parents who are Rh positive can give birth to children who are Rh negative.
Problems in determining Rh status: Most Rh positive individuals express a sufficient number of antigenic determinants containing all epitopes. In this case, when determining Rh status, regardless of the test systems used, no problems arise, and Rh status is clearly defined as positive.
However, for a number of individuals (no more than 1% in the European population), difficulties may arise when determining Rh status for the following reasons: 1. The number of antigenic determinants is reduced by 3-10 times, but they are not structurally changed. This version of the antigen is called weak, D weak. The degree of reduction in the number of determinants varies, so the agglutination reaction in such patients can occur with varying degrees of severity. 2. The number of antigenic determinants may be normal, but they are structurally altered. The determinants of the D antigen lack some epitopes (up to 5 epitopes may be absent at the same time). This version of the antigen is called incomplete, variant or partial, D partial . More than 10 such forms of antigen D have been identified in humans. The most common is the DVI antigen variant (occurrence of no more than 0.1% in the European population). 3. The variant of the Rh antigen D el is typical for the Asian population, the occurrence is up to 30%. Manifested by very low expression of antigen D on the surface of red blood cells. Most often, by conventional methods it is determined as Rh-negative. From a clinical point of view, it is important to distinguish between these options, especially in women of childbearing age and when planning blood transfusion. With the “incomplete” variant (D partial), it is possible to form antibodies to the “complete” D antigen through transfusion of Rh-positive blood or hemocomponents. With the “weak” variant (D weak), the formation of Rh antibodies is unlikely. The approach to performing the study and interpreting the results of the Rh status of potential recipients and potential donors is different.
| Antigen variant | Interpretation for the recipient | Interpretation for the donor |
| D weak | Rh positive, but for blood transfusion it is recommended to use Rh negative red blood cells | Rh positive |
| D partial, including D VI (D partial) | Rh negative | Rh positive |
| Del | Rh negative | Rh positive |
What is the research used for?
— To determine whether a person’s blood group belongs to one of the groups according to the ABO system and the Rh system.
When is the study scheduled?
— When transfusing blood components to a recipient;
- when donating blood by a donor;
— in preparation for surgical operations;
- when planning pregnancy or during pregnancy;
— Hemolytic disease of newborns (detection of incompatibility of the blood of mother and fetus according to the Rh factor);
— in preparation for transplantation of bone marrow, kidney, liver and other organs and tissues;
- upon entering military service, into the ranks of the Ministry of Emergency Situations and other law enforcement agencies.
What is needed to determine blood type and Rh factor?
Anyone can determine the Rh factor and blood group. For this purpose, venous (from a vein) or capillary (from a finger) blood is taken, after which its parameters are examined using specialized equipment. Preparation for the procedure only includes limiting food intake for 3 hours before the study. These studies are usually performed in urgent mode, “cito” mode, so you can find out your blood type and your Rh status on the same day.
Get tested for the Rh factor and determine your blood group in ABC - faster, more pleasant and more reliable!
4. Risks of analysis and what can affect the result?
Risks of blood group testing
If you are taking a blood group test, then possible risks may only be associated with taking blood from a vein. In particular, the appearance of bruises at the site of blood sampling and inflammation of the vein (phlebitis). Warm compresses several times a day will relieve phlebitis. If you are taking blood thinning medications, you may bleed at the puncture site.
What can change the blood type result?
If you have had a blood transfusion or bone marrow transplant, your blood type test results may change.
2.Test for Rh factor
The Rh factor test allows you to determine whether you have another antigen in your blood. If you have it, your blood type is assigned a positive Rh factor; if not, it is assigned a negative Rh factor.
Determining the Rh factor is especially important for pregnant women,
because If a woman has a negative blood type, and the child has a positive blood type, then during childbirth or pregnancy the blood may mix, and the antibodies in the mother’s blood will destroy the child’s red blood cells, perceiving it as an object foreign to the body.
Why is a blood group test performed?
Blood group analysis is carried out:
- Before blood transfusion;
- Before donating blood;
- Before organ transplantation from the donor and recipient;
- Before surgery;
- When planning pregnancy;
- To check whether two people could be blood relatives.