Blood biochemistry
05/05/201801/24/2019 Yulia Martynovich (Peshkova) 2310 Views bilirubin, biochemistry
An article about bilirubin; the norm for men by age is presented, a summary table for convenience. Bilirubin is a yellow-green bile pigment that functions as an antioxidant in the human body and is part of bile. A blood test to determine the norm of total (direct + indirect) bilirubin in men is the first stage in diagnosing pathologies of the liver and bile ducts.
The study is of particular importance for elderly patients over 60 years of age and those who abuse alcohol, since their liver’s detoxifying ability is reduced. Deviation of the criterion from the norm always indicates pathology.
- 1 Types of bilirubin: direct, total and indirect
- 2 What are the indications for bilirubin testing in men?
- 3 How can a man prepare for a bilirubin test?
- 4 Norm of bilirubin in blood in men and summary table
- 5 Increased indicator: a variant of the norm or a sign of pathology?
- 6 How to return bilirubin levels to normal?
Types of bilirubin
Total bilirubin is divided into two parts - bound (conjugated) and free (unconjugated). They differ in their ability to dissolve in water.
Unconjugated bilirubin:
- It is formed in the spleen, which ensures the utilization of red blood cells. In the process of their destruction, bilirubin appears. Due to its inability to dissolve in water, free bilirubin is not excreted from the body by the kidneys.
- In the blood it interacts with albumin and in the liver it is converted into bound albumin.
- It accumulates in adipose tissue and, in excess, has a toxic effect on the body: it disrupts protein synthesis and negatively affects cellular respiration.
Conjugated bilirubin is water-soluble, formed in the liver, low-toxic, and practically harmless. The bound pigment is excreted in urine and feces.
General information
The renewal of red blood cells circulating in the blood is a physiological process. When they are destroyed, hemoglobin turns into indirect bilirubin. It is transported to the liver. Here the pigment combines with a sugar-containing substance. This compound is able to dissolve in liquid and is called direct bilirubin. It enters the intestines. Here the compound breaks down and a pigment is formed, which is excreted in the feces.
The direct fraction of the pigment is normally present in the blood only in small quantities. If bilirubin is not removed from the body in a timely manner, its concentration in the blood increases. The cause of this may be liver damage or blockage of the bile ducts. In the second case, bilirubin cannot enter the intestines and turn into brown pigment. Instead, it goes into the urine. Therefore, with this pathology, urine becomes dark, and feces, on the contrary, become lighter.
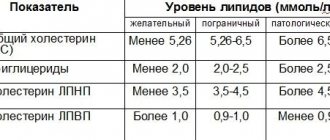
Norm of bilirubin for men
Direct bilirubin makes up approximately 1/5 of the total pigment in the blood of men. Normal bilirubin levels are as follows:
- general - up to 20.5 µmol/l;
- bound - up to 4.2 - 4.5 µmol/l;
- unbound - up to 15.3-17.1 µmol/l.
In different laboratories, indicators of the normal amount of bilirubin in the blood may differ slightly: the error is 10-15%. The approximate ratio of unconjugated and conjugated bilirubin is 3:1, 4:1.
In men over 50 years of age, the concentration of pigment in the blood changes.
Normal bilirubin content in the blood of men of different age groups:
| 17-20 years old | 3.7 - 18 µmol/liter; |
| 21-30 years old | 3.8 - 19 µmol/liter; |
| 31 - 40 years 3.8 | 8.5 µmol/liter; |
| 41-50 years | 3.9 - 18.7 µmol/liter; |
| 51 - 60 years | 3.8 - 18.5 µmol/liter; |
| 61 - 70 years | 3.7 - 18.5 µmol/liter; |
| 71 years and older | 3.5 - 18.2 µmol/liter. |
The amount of bilirubin in the blood is a marker of changes in the body and allows for the timely detection and elimination of various diseases. This is what the change in pigment concentration indicates.

Increased bilirubin
Often indicates accelerated breakdown of red blood cells. An increase in bilirubin in the blood may be associated with cirrhosis of the liver, hepatitis, anemia, and diseases of the pancreas. Unconjugated bilirubin negatively affects the functioning and functionality of the nervous system. A high concentration of pigment indicates its accumulation in the body.
Bound bilirubin increases when:
- liver cirrhosis;
- gallstone disease;
- hepatitis;
- helminthiasis;
- drug intoxication;
- Rott syndrome;
- blockage of the biliary tract.
An increase in the concentration of unbound bilirubin is observed in the following diseases and conditions:
- Gilbert, Lucy-Driscoll syndrome;
- congenital or acquired anemia;
- typhoid fever;
- sepsis;
- syphilis;
- internal hemorrhages.
Exceeding the norm of bilirubin in the above diseases may be associated with impaired bile outflow, increased destruction of red blood cells, or deterioration in the processing of pigment in the liver.

Taking insulin, aspirin, and chloramphenicol can also cause an increase in bilirubin.
In addition, bilirubin increases due to alcohol abuse, tattooing, poor diet, and smoking.
Direct bilirubin
Other names: Direct bilirubin, conjugated bilirubin, conjugated bilirubin, newborn bilirubin, Direct bilirubin, Conjugated bilirubin.
Service code for ordering 1049 (direct bilirubin) in the Sinevo medical laboratory.
general information
Bilirubin is a pigment found in bile. It is formed during the breakdown of waste hemoglobin, the main component of red blood cells. This is due to the constant renewal of red blood cells. The body reuses iron, which is part of hemoglobin, and the protein part of the molecule is converted into bilirubin.
Initially, when hemoglobin is broken down, indirect (unbound, unconjugated) bilirubin is formed. This bilirubin is toxic and to neutralize it, it is transported in the blood to the liver using a special protein - albumin. There it binds to a special component - glucuronic acid - and turns into direct (bound, conjugated) bilirubin, which, in turn, is non-toxic and is excreted with bile into the intestines and kidneys for excretion from the body. Total bilirubin determined in the blood is the sum of indirect and direct bilirubin.
Normally, direct bilirubin is practically not found in the blood. Its amount increases in cases where the liver is able to form direct bilirubin from indirect bilirubin, but cannot remove it in a timely manner. Most often this happens due to blockage of the bile ducts, as well as due to damage to liver tissue due to hepatitis or cirrhosis.
When the outflow of bile is obstructed (impaired outflow), bilirubin does not enter the intestines and, accordingly, does not turn into a brown pigment, so the stool becomes lightened. Excess amounts of direct bilirubin, penetrating into the urine, begin to give it a dark color.
In the Sinevo laboratory, total and direct bilirubin . The difference between them is the amount of indirect bilirubin.
Bilirubin is a marker of liver biliary tract dysfunction.
Indications for use:
- routine medical examination;
- preparation for surgical operations;
- alcohol abuse;
- jaundice of unspecified etiology;
- when symptoms appear (symptoms appear): weakness, loss of appetite, nausea, vomiting, abdominal pain (especially in the right hypochondrium), darkening of urine and lightening of stool, itching;
- assessment of the degree of bilirubinemia;
- differential diagnosis of various types of jaundice (jaundice) (study of bilirubin fractions);
- diseases of the liver and biliary tract;
- hemolytic anemia.
Method: colorimetric diazo method
Analyzer: Cobas 6000
Units: µmol/l
Material for research: venous blood serum
Preparation:
- Take on an empty stomach (after sleep and 8–12 hours of fasting). It is permissible to drink only clean non-carbonated water (up to 200 ml) (with the exception of glucose testing);
- do not consume spicy, fatty, fried foods and alcohol 1–2 days before the test;
- exclude physical and emotional stress 1 day before the analysis;
- do not smoke for at least 1 hour before the test;
- It is not recommended to take (take the test) after radiography, physiotherapeutic procedures and instrumental examinations.
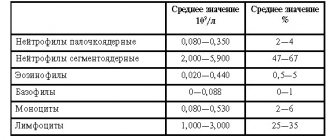
Interpretation of results: (analysis results)
The result of laboratory tests is not a sufficient basis for making a diagnosis. Interpretation of the results and diagnosis is carried out only by the attending physician.
Reference values:
less than 5.0
Level up:
- hepatitis of various etiologies (acute viral hepatitis, hepatitis caused by cytomegalovirus, infectious mononucleosis, amoebiasis, opisthorchiasis, actinomycosis, secondary and tertiary syphilis, acute toxic hepatitis);
- taking hepatotoxic medications;
- pathology of the biliary tract (cholangitis, cholecystitis);
- oncopathology (primary hepatocarcinoma, metastatic liver lesions);
- hereditary hyperbilirubinemia (Dabin-Johnson syndrome, Rotor syndrome);
- hypothyroidism in newborns;
- obstructive jaundice (gastrointestinal tract disease, tumors of the head of the pancreas, helminthic infestation);
- biliary cirrhosis (primary or secondary);
- jaundice of pregnant women.
Downgrade:
- anemia of a non-hemolytic nature (CRF, tuberculosis, acute leukemia, post-hemorrhagic anemia);
- in premature babies (prematurity in children);
- smoking;
- the effect of sunlight or ultraviolet rays on a blood sample.
Factors influencing the result:
Promotion:
Substances that increase bilirubin levels: acebutolol, acyclovir, allopurinol, amitriptyline, antifungal drugs, antimalarial drugs, antipyretics, barbiturates, captopril, carbamazepine, cephalosporins, clindamycin, cyclosporine, diclofenac, doxorubicin, doxycycline, enalapril, furosemide, methotrexate, methyldopa, papaverine, penicillin, rifampicin, streptomycin, thiazides, hepatitis B vaccine, BCG vaccine, etc.
Demotion:
Substances that affect the decrease in bilirubin levels:
- alcohol,
- barbiturates,
- caffeine,
- prednisolone,
- penicillin,
- amikacin,
- anticonvulsants,
- theophylline, etc.
Where to get tested for direct bilirubin
take a blood test for direct bilirubin at any Synevo point in Minsk, Baranovichi, Bobruisk, Borisov, Brest, Vitebsk, Gantsevichi, Gomel, Grodno, Zhlobin, Lida, Mogilev, Mozyr, Molodechno, Novogrudok, Novopolotsk, Orsha, Pinsk, Polotsk, Rechitsa, Svetlogorsk, Slutsk, Smorgon, Soligorsk.
Signs of increased pigment in the blood
When the concentration of bilirubin in the blood increases, the following symptoms are observed:
- itchy skin;
- yellowness of the skin and mucous membranes;
- feeling of heaviness in the right hypochondrium;
- bitterness in the mouth;
- hyperthermia;
- general weakness, headaches;
- dyspeptic disorders;
- discoloration of stool;
- change in urine color.
Skin color with increased bilirubin depends on the type of “jaundice”. Thus, adrenal jaundice is caused by the accelerated destruction of red blood cells and gives the skin a yellowish-lemon tint. Hepatic jaundice occurs when bilirubin metabolism is disrupted and gives a yellowish-saffron color. Subhepatic jaundice appears when there is a change in the transport of bile and is distinguished by a yellow-greenish tint.
Sometimes an increase in bilirubin has no clinical manifestations and is detected by chance during testing.

Detailed description of the study
The liver is an organ in which complex metabolic processes occur. The functional activity of the liver is provided by hepatocyte cells, they are responsible for:
- Bilirubin exchange and bile formation;
- Regulation of carbohydrate metabolism;
- Regulation of fat metabolism;
- Formation of many proteins, including enzymes;
- Neutralization of toxic substances (medicines, alcohol, etc.).
Bilirubin is an orange-yellow pigment formed during the breakdown of heme (a component of hemoglobin). Every day, the human body synthesizes about 350 mg of indirect (free) bilirubin. Most of it is formed during the breakdown of red blood cells, a smaller part (about 20%) is formed from other heme proteins in the liver and bone marrow.
Free bilirubin is insoluble in water; it is transported in human blood plasma in combination with a protein - albumin. Next, the liver captures free bilirubin, and after a series of transformations it is converted into direct (associated with glucoronic acid) bilirubin, which is soluble in water.
Bound bilirubin in bile is sent to the gallbladder and released into the small intestine during food digestion. In the small intestine it is metabolized by bacteria to urobilinogen. Most of the urobilinogen is transformed into stercobilin, which turns the stool brown. A small amount of urobilinogen is reabsorbed by the liver and returns to the bile. A small part is excreted in the urine.
Normally, the level of indirect bilirubin in the blood is very low. If the concentration of bilirubin and its fractions increases, a person may develop yellowness of the skin and whites of the eyes. This condition is called jaundice.
Depending on the cause of bilirubin metabolism disorders, there are three types of jaundice:
- Hemolytic;
- Parenchymatous;
- Mechanical.
1) Hemolytic, or suprahepatic, jaundice is associated with increased release of bilirubin into the blood due to increased breakdown of red blood cells. The pigment formed during destruction is not captured by hepatocytes, but remains in the blood (having a toxic effect). A similar pathology can be observed in newborns when their Rh factor is incompatible with that of the mother (Rh conflict).
In rare cases, a congenital disorder of bilirubin metabolism known as Gilbert's syndrome occurs. This disorder is associated with reduced activity of the enzyme glucuronyl transferase, which converts indirect bilirubin into direct bilirubin. As a rule, it is determined by chance and has a favorable clinical course.
Hereditary diseases associated with defects in the functioning of enzymes responsible for bilirubin metabolism also include Dubin-Johnson syndrome and Rotor syndrome.
Increased release of indirect bilirubin into the blood accompanies hemolytic anemia. This condition is also associated with the premature breakdown of red blood cells and the inability to fully metabolize this pigment in liver cells due to its excess.
May be caused by internal defects in the red blood cells themselves (hereditary pathology) or:
- Taking certain medications (methyldopa, penicillin, quinine, etc.);
- Immunological disorders;
- Infections;
- Mechanical damage to blood vessels;
- Toxic effects (copper, lead).
2) Hepatic, or parenchymal, jaundice occurs due to lesions of the liver tissue. Such conditions are diagnosed with viral hepatitis, poisoning, sepsis, etc.
3) Mechanical, or subhepatic, (obstructive) jaundice occurs due to the presence of mechanical obstacles (stones, tumors) in the bile ducts, which impairs the outflow (excretion) of bile.
A bilirubin test may be used as part of an annual physical to evaluate liver health. It is also used to determine the causes of jaundice and helps the specialist determine the tactics of further therapy.
The study is also carried out in newborns with jaundice to determine its causes.
Nutrition to normalize bilirubin
To normalize bilirubin levels, men are advised to exclude salt from their diet and reduce the amount of meat and bread. Doctors also do not recommend eating the following foods:
- mushrooms;
- mayonnaise, mustard;
- lemon, onion;
- smoked products, sausages;
- seafood;
- canned foods;
- alcohol;
- products containing dyes or sweeteners.
You should eat small meals; you should not eat fast foods. Doctors recommend drinking more fluid - up to 2.5 liters per day. This includes not only water, but also green tea and unsweetened compotes.
List of allowed foods and dishes to normalize bilirubin levels:
- cottage cheese, milk;
- non-acidic fruits;
- chicken and quail meat, rabbit meat;
- soups with vegetable broth or milk;
- herbal infusions.
Traditional medicine recommends drinking beet juice, decoctions of various herbs, and motherwort.