General information
As a result of the breakdown of hemoglobin in red blood cells, bilirubin is released, which is a very toxic component. By binding to glucuronic acid (this process occurs in the liver), bilirubin loses the ability to negatively affect the body. Together with bile, it enters the intestine, where it is fermented, oxidized, metabolized (breaks down), resulting in the appearance of urobilinogen.
The resulting bile pigment is partially sent through the bloodstream to the kidneys and excreted in the urine, giving it a characteristic yellow color. The remaining part of urobilinogen, when moving into the large intestine, is transformed into stercobilin and excreted in the feces, giving them a natural brown tint.
Normally, a small amount of urobilinogen is always present in the urine, although it may not be detected in the laboratory. The increase in concentration is due to:
- intensive breakdown of hemoglobin in erythrocytes and, as a consequence, the formation of large amounts of bilirubin;
- functional pathologies of the liver, for example, the inability to “process” bilirubin;
- various pathological processes in the intestines, as a result of which bilirubin metabolism is disrupted.
The absence of urobilinogen in the urine indicates that bilirubin does not enter the intestinal lumen. As a rule, a similar situation is observed with blockage of the bile ducts, fistulas, hepatitis, liver failure, destructuring of liver tissue, etc.
General urine analysis: table of average values, interpretation of indicators, rules for delivery
A general or clinical urine test is a set of diagnostic tests aimed at studying the physicochemical and biochemical properties of the patient’s urine and its microscopic examination.
Conducting a general urine test is advisable if you suspect kidney and urinary tract diseases of various etiologies, endocrine disorders, acidosis and alkalosis, dehydration, poisoning, gout, hemolytic anemia, hepatitis and a number of other pathologies, and is also prescribed for preventive purposes. The subjects of the study are organoleptic indicators (volume, color, smell, transparency, foam formation), physicochemical characteristics (density, acidity), biochemical characteristics (protein, bilirubin), sediment composition. Table of reference values for general urine analysis indicators
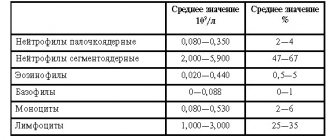
| Index | Designation | Norm | Units |
| Organoleptic properties | |||
| Color | COLOR | Straw yellow to yellow | |
| Smell | Specific, unobtrusive | ||
| Foaminess | There is virtually no foam when shaking | ||
| Transparency | TURB | Absolute | |
| Physicochemical characteristics | |||
| Density | S.G. | 1003–1030 | g/l |
| Acidity, reaction | pH | 5–7,5 | |
| Biochemical composition | |||
| Protein | PRO | 0–0,033 | g/l |
| Glucose | G.L.U. | 0–0,8 | mmol/l |
| Bilirubin | BIL | 0–8,5 | µmol/l |
| Urobilinogen | URO, UBG | 0–17 | µmol/l |
| Ketone bodies | KET | 0–0,5 | mmol/l |
| Nitrites | NIT | none | |
| Sediment microscopy | |||
| Epithelium | SQEP, NSE | Men: 0–9 Women: 0–15 | cells/µl |
| Slime | MUCS | missing or traces | |
| Red blood cells | RBC, BLD | 0–11 | cells/µl |
| Leukocytes | WBC, LEU | Men: 0–16.5 Women: 0–27.5 | cells/µl |
| Hemoglobin | HGB | Absent | |
| Cylinders (hyaline, granular, waxy) | HYAL, UNCC. | None | |
| Salts | None | ||
| Bacteria | BACT | None | |
| Parasites | None | ||
| Fungi | BYST | None |
Interpretation of the results of a general urine test
Before proceeding to the interpretation of the results of a general urine test, we must remind you that all the information presented in the article is advisory and informational in nature and cannot be used to make a diagnosis or prescribe treatment. Consultation with a doctor is required! Now let's look at each of the points in the table and find out what the difference between your results and the reference ones, that is, from the average statistical indicators, may indicate.
Color. A straw-yellow color is considered normal, but even in a healthy person, depending on diet and other factors, the shade can vary from colorless to amber. The idea of pathology is suggested by a clear change in color. A dark, beer-colored color, even brown and brown, indicates an increase in bilirubin or urobilinogen. If it looks like milk, leukocytes are elevated; Black urine indicates the presence of hemoglobin or myoglobin. Red color is a dangerous sign, hinting at the release of blood in the urine; in rare cases, bluish-green shades are observed, explained by the processes of decay in the intestines and the subsequent release of special coloring substances into the blood.
Smell. Ammonia smells after urination due to bacterial infections and inflammatory processes in the urinary system; smells like rotten fruit due to an increase in the concentration of ketone bodies, which is usually a symptom of diabetes; Diabetes can also smell like acetone.
Transparency. Cloudy urine is caused by the deposition of salts, crystals, white and red blood cells, mucus and pus. Severe thread-like and flocculent joints often accompany pyelonephritis and lower urinary tract infections. But urine collected for analysis often becomes cloudy due to the laboratory’s failure to comply with the sample storage conditions.
Foaminess . If a lot of persistent foam is formed during shaking, then this hints to the specialist that there is a possibility of jaundice or an increased protein content. Other explanations may be the patient’s poor psycho-emotional state, concussion, poor circulation in the brain, advanced diabetes mellitus, heart failure and a number of endocrine disorders.
Relative density. Specific gravity characterizes the ability of the kidneys to concentrate and dilute urine. If the indicator exceeds the lower limits of the reference values, it indicates renal failure, polyuria, tubular pathology, or diabetes insipidus of various etiologies. Elevated relative density values often indicate the development of glomerulonephritis, nephrotic syndrome, diabetes mellitus, dehydration, or result from the intravenous administration of a number of drugs and radiocontrast agents.
Acidity. In a healthy person, the urine reaction is slightly acidic; it shifts toward the alkaline side (pH > 7) when consuming large amounts of products of plant and dairy origin, and toward the acidic side (pH < 5) when consuming products of animal origin. Pathological acidification of urine is also caused by hypokalemia, diabetes mellitus, gout, and alkalization is caused by kidney and urinary tract diseases of an inflammatory or infectious nature, diarrhea, vomiting.
Squirrels. The presence of protein in urine samples - proteinuria - can be a consequence of physical and emotional stress, a symptom of heart failure, arterial hypertension, elevated body temperature, gestosis in pregnant women, nephroptosis, injuries. The activity of kidney filters can be disrupted due to prolonged standing, so sometimes protein penetrates from the blood into the urine of hairdressers, salespeople, the military and people in other professions with stationary work. Renal causes of proteinuria include damage to the tubules and glomeruli, nephrosclerosis. Neoplasms can also make this test item positive.
Glucose. There should be no sugar in urine. If a glucose value in the results of about 0.1 mmol/l may be a consequence of an excess of sweets in the diet, then values of 0.9 mmol/l and above clearly indicate a high probability of diabetes. Other relatively common causes of glycosuria include pancreatitis, Cushing's syndrome, Fanconi syndrome and pregnancy.
Ketone bodies. The appearance of ketone bodies in the tests of a patient with diabetes mellitus indicates the progress of the disease. In patients without diabetes, ketone bodies are detected during fasting, due to a sharp decrease in carbohydrates in the diet, or a prolonged fever.
Bilirubin. Determining the amount of bilirubin in urine becomes possible in case of damage to the liver parenchyma, disruption of the processes of bile outflow, cirrhosis of the liver, viral hepatitis and metastasis of neoplasms to the liver.
Urobilinogen. Traces of urobilinogen in the urine may indicate blood diseases (hemolytic and pernicious anemia, hemolysis, polycythemia, consequences of extensive hematomas), diseases of the gastrointestinal tract (inflammatory and obstructive diseases), liver diseases (viral hepatitis, chronic hepatitis, cirrhosis, secondary failure, neoplasms), disorders of the cardiovascular system (myocardial infarction, heart and circulatory failure) or intoxication of the body with alcohol, infection or organic compounds.
Nitrites. Normally, there are no nitrites in the urine; their presence indicates an infection of the urinary tract.
Red blood cells. The correct interpretation of erythrocyturia requires taking into account the medical history and the results of a blood test, since there are many reasons for the increase in erythrocytes. The increase in concentration may have a physiological explanation and be temporary (long standing, exhausting walking and physical activity), and may accompany the use of medications. If the causes of erythrocyturia are still pathological, then the specialist may suspect hypertension, diathesis, glomerulonephritis, urolithiasis, pyelonephritis, neoplasm, systemic lupus erythematosus, vasculitis, infective endocarditis, heart failure, trauma or infarction of the kidney.
Leukocytes. The level of leukocytes in the urine increases in almost all diseases of the kidneys and genitourinary system: all forms of pyelonephritis, glomerulonephritis, cystitis, urethritis, prostatitis, urolithiasis, lupus nephritis, etc. Another explanation may be fever.
Hemoglobin. Hemoglobin accumulates in the urine in parallel with erythrocyturia, with myositis, massive damage to muscle tissue, thrombus formation in muscle vessels, myocardial infarction, hemolytic anemia, burns, mushroom and phenol poisoning.
Epithelium. There are elements of squamous, transitional and renal epithelium. The appearance/increase of squamous epithelial cells is observed with infection of the urinary tract, transitional epithelium - with cystitis, pyelonephritis and urolithiasis, renal epithelium - with glomerulonephritis, pyelonephritis, poisoning with salts of heavy metals, pathology of the blood circulation of the kidneys.
Cylinders. The detection of hyaline casts in the urine indicates kidney pathology, heart failure or overheating of the body (fever, heatstroke, sunstroke). In some cases, they are detected after excessive physical exertion, taking diuretics and exacerbations of arterial hypertension. Granular casts are excreted in the urine during glomerulonephritis, pyelonephritis, diabetic nephropathy, viral diseases, fever and lead intoxication. Increased waxy casts indicate amyloidosis, renal failure, or nephrotic syndrome.
Salt. Almost absent in the urine of a healthy person, their appearance hints at a violation of mineral metabolism, the development of urolithiasis, nephrolithiasis, dehydration of the body, and chronic renal failure.
Slime. The mucus content in the sample is most often explained by a banal violation of the rules for collecting urine. But mucus is also actively secreted in the urine during inflammatory processes.
Bacteria, fungi, parasites. Their appearance in the urine is explained by a corresponding urinary tract disease.
How to prepare for and take a urine test
- The day before collecting urine, you should avoid foods that contain strong natural dyes: beets, blueberries, carrots, etc. It is also recommended to avoid alcohol, coffee and strong tea.
- On the eve of submitting the sample, you should refrain from visiting the bathhouse or sauna, from strenuous physical activity and from taking diuretics (possibly after consulting a doctor).
- Girls are not recommended to take the test during menstruation, as even minor traces of blood in the urine can make the test results inconclusive.
- If you are undergoing a course of drug treatment, you should notify your doctor or laboratory technician about the medications you are taking. You should do the same if you had invasive tests or procedures on your urinary tract in the week before your urine collection.
- A urine sample must be brought to the laboratory in a special disposable sterile container, which is cheap and sold at any pharmacy. But samples from glass containers will simply not be accepted in the laboratory.
- If no other instructions are received from the doctor, then the first morning portion of urine is collected to perform the tests. A small volume should be released into the toilet and then, without stopping urination, draw about 50 ml of urine into the container. Try to avoid contact of the sterile container with skin and mucous membranes.
- Before collecting urine, you must take a shower with hygienic treatment of the external genitalia, but without using antibacterial and disinfectants.
- It is not recommended to stimulate urination with copious amounts of water, tea and other diuretic liquids - this may affect the results.
- Results may be affected by strong emotional stress.
- High blood pressure can also cause inaccurate testing.
Indications for analysis
A test for urobilinogen is carried out as part of a general urine test; you especially need to pay attention to the results for the following symptoms:
- Urination problems: feeling of incomplete emptying of the bladder;
- frequent urge;
- urinary incontinence, etc.;
The interpretation of the results of the urobilinogen test is carried out by a nephrologist, infectious disease specialist, urologist, gynecologist, family doctor, pediatrician, therapist, and functional diagnostician.
How to prepare and how the analysis is carried out
The urobilinogen test does not require preliminary preparation. The only thing doctors ask is that on the eve of urine collection, avoid foods that can change its color. These are beets, carrots, pumpkin. You should also not use medications (unless absolutely necessary) that give urine an unnatural color - analgin, acetylsalicylic acid, otherwise the analysis for urobilinogen will be biased.
To collect urine, prepare a disposable container purchased at a pharmacy or a well-washed dry jar with a volume of up to 200 ml with a lid. In the morning after sleep, you need to rinse the area of the external genitalia and dry it with a clean towel. Fill the container with 80-100 ml of urine.
The material is delivered for analysis no later than 2 hours after collection.
Urobilinogen norms
Values not exceeding 34 mmol/l are considered normal.
Factors of influence
- In pregnant women, fluctuations in urobilinogen concentration are allowed throughout pregnancy. However, the appearance of “brown urine” is considered as a variant of liver pathology and requires consultation with a specialist;
- In newborns, an increase in the level of urobilinogen in the urine is observed in combination with physiological jaundice. The condition stabilizes after the symptoms disappear;
- In children 3-4 months of age, urobilinogen may be completely absent due to functional inferiority of the intestine. The introduction of complementary foods normalizes the intestinal microflora, as a result of which the concentration of urobilinogen in the urine returns to normal;
- With dehydration and/or insufficient fluid intake, the concentration of urine increases, along with which the level of urobilinogen also increases;
- Against the background of severe dysbacteriosis, beneficial bacteria that convert bilirubin into urobilinogen die, so the concentration of the latter in the urine decreases.
How to collect urine: advice to patients
It is not difficult to correctly submit urine for analysis:
- urine should be collected in the morning, after hygiene procedures, bypassing the beginning and end of the act of urination,
- collect an average portion of urine, it is advisable to choose a dark-colored jar (it is very important to comply with this wish, because urobilinogen is destroyed under the influence of light),
- carry out the analysis quickly, oxygen will not have the best effect on the test results.
The modern pharmacological industry produces special test strips that carry out research in a screening manner. This method is preferable for mass poisonings, in places where there is no laboratory nearby.
Initially, screening strips have a white or cream tint; after exposure to urine, they change color due to chemical reactions. The strips come with instructions, a multi-colored scale that allows you to determine the level of urobilinogen in urine.
The results obtained have high diagnostic accuracy; the doctor supplements them with other studies, makes a diagnosis, and prescribes the necessary course of therapy.
Urobilinogen and bilirubin
If repeated OAM reveals increased urobilinogen, the presence of bilirubin in the urine must also be taken into account.
- A decrease in urobilinogen values in urine with a simultaneous increase in bilirubin concentration occurs as a result of a violation of the outflow of bile (obstruction of the bile ducts);
- Moderately increased urobilinogen against the background of a complete absence or decrease in bilirubin concentration is observed in various liver injuries/pathologies;
- Hemolytic diseases are characterized by high concentrations of urobilinogen and a complete absence of bilirubin in the urine.
What analysis shows urobilinoids in urine
The level of urobilinogen is determined during a general clinical analysis (CCA). But you can suspect an increase or decrease in their number by visually assessing the color of the biological fluid. With a high content of urobilinoids, the color of urine changes - it becomes dark; with a low concentration of bile breakdown products, it becomes almost colorless.
Both phenomena should be a reason to see a doctor and undergo an examination. First you will have to pass the OAM. The result form will indicate the amount of urobilinogen (UBG, URO). Based on this, the doctor will prescribe further diagnostics or allay concerns regarding the patient’s health condition.
Increasing values
- Excessive secretion of bilirubin or slow rates of bilirubin breakdown;
- Liver diseases; failure;
- cirrhosis;
- hepatitis;
- hepatic vein thrombosis;
- oncology;
- enterocolitis (inflammation of the large intestine);
conclusions
A urine test for urobilinogen is informative for the doctor and the patient because:
- makes it possible to learn about the state of metabolism, the function of the liver, biliary tract, intestines, blood and kidneys (a person is healthy or not);
- helps to exclude certain pathologies or make a diagnosis if assessed together with other indicators of urine, blood and feces tests;
- necessary to monitor the condition of a pregnant woman, because urobilinogen increases during this period;
- in patients with chronic pathology of internal organs associated with the metabolism of bile acids (bilirubin and its derivatives), it helps to identify periods of exacerbation, monitor the effectiveness of prescribed treatment and the dose of drugs;
- necessary when following a diet, choosing the right diet that does not disrupt metabolism;
- during blood transfusions, infections, poisoning, indicates the degree of destruction of red blood cells and how organs cope with the function of neutralizing byproducts of red blood cell breakdown;
- analysis values may vary depending on age, food intake, physiological conditions requiring heavy load (pregnancy);
- the study is indicative, to diagnose the causes of increased urobilin, you need to take additional tests and undergo a full examination;
- Treatment of diseases that cause changes in the level of urobilin bodies in the urine may require consultation with several doctors.
Lowering values
This fact usually does not have diagnostic value for specialists. But if urobilinogen is reduced/absent against the background of increased bilirubin, then a number of pathologies should be excluded:
- obstruction of the biliary tract (common causes are spasm of the bile ducts, obstruction by stones in gallstones);
- hepatitis A (non-infectious liver damage, accompanied by yellowness of the skin and mucous membranes);
- impaired filtration function of the kidneys;
- other kidney diseases: oncology;
- glomerulonephritis;
- pyelonephritis, etc.
Correction of indicators
To normalize liver functions and reduce pathological levels of urobilin, a number of drugs with targeted action are used:
- essential phospholipid hepatoprotectors (Essliver, Gepagard, Phosphogliv, Eslidin, Enerliv, Phosphonciale, Essentiale Forte N);
- plant-based hepatoprotective agents (Liv-52, Bonjigar, Silimar/Karsil, Diapana, Galstena, Cyrinax);
- hepatoprotectors-lipotropics (Heptral, Hepa-Merz, Betargin);
- Dietary supplements and vitamin complexes for the liver (Tiogamma, Berlition 300, Thiolepta, Lipothioxone, lipoic acid, Thiolipon);
- bile acids of synthetic origin: Ursosan and analogues of the drug.
All medications must be prescribed by a doctor.
Urobilinogen in pregnant women and children
For expectant mothers, the same reference values are determined as for everyone else. A temporary increase in urobilinogen levels is allowed, which is associated with the growth of the uterus and an increase in the load on the kidneys and gastrointestinal tract.
Important!
In case of sudden darkening of urine, it is necessary to urgently take a test for urobilinogen to exclude liver pathologies or acute intoxication. The likelihood of developing diseases of the hepatobiliary system increases in women with a hereditary predisposition.
In most cases, the concentration of urobilinogen increases due to dehydration. At the same time, urine becomes denser and richer. Dehydration can be caused not only by insufficient fluid intake, but also by changes in the daily diet, taking dietary supplements and vitamins, as well as some other medications. Dehydration is also observed in the early stages of pregnancy (toxicosis of the first half). This condition is accompanied by a significant increase in urobilinogen in the urine (2-3 times).
In children, urobilinogen normally should not exceed 3.2 mmol/l. In case of increased concentration, differential diagnosis of the following diseases is carried out:
- cholelithiasis;
- hepatitis of various etiologies;
- physiological jaundice (destruction of specific hemoglobin and associated red blood cells);
- liver cirrhosis in acute or chronic form;
- dysbacteriosis (often observed in children of the younger age group);
- anemia (anemia, low blood hemoglobin);
- colitis and enterocolitis caused by pathogenic bacteria or helminths;
- poisoning with food, drugs, etc.
Clinical symptoms requiring testing for bilirubin
- An increase in the size of the spleen and/or liver and associated pressing pain in the left/right hypochondrium;
- High fever (increased body temperature) for a long time (up to several days);
- Change in the color of urine (a dark brown, almost black tint is often observed);
- Tachycardia (increased heart rate);
- Weakness, increased fatigue, sweating;
- Loss of appetite, belching, nausea, diarrhea, flatulence;
- Bitterness in the mouth after eating (due to a violation of the outflow of bile);
- Discoloration of stool;
- Skin itching and rashes of unknown origin;
- Yellowing of the mucous membranes and skin.