Full text of the article:
Esophagogastroscopy
(from Latin-Greek, where oesophagus - esophagus gaster - stomach, duodenum duodenum, skopeo - look) - a type of endoscopic highly specialized examination of the upper gastrointestinal tract (esophagus, stomach, duodenum) using a flexible endoscope. Endoscopy is performed for diagnostic and therapeutic purposes. The unique optical capabilities of the device allow you not only to examine all areas of the mucous membrane of the diseased organ, to examine the pitting and vascular pattern, but also to take photos and videos of it.
This procedure allows you to study the condition of the organs of the upper gastrointestinal tract in one go, and if necessary, makes it possible to carry out additional diagnostic (test for Helicobacter pylori, chromoscopy, acidity determination, manometry) and therapeutic manipulations (stop bleeding, perform blood sampling). piece of tissue for histological examination and remove neoplasms).
How is gastroscopy (esophagogastroduodenoscopy) performed?
To conduct the examination with the greatest information content, it is important to know how to prepare for the gastric endoscopy procedure:
- To reduce the manifestations of the gag reflex, the patient’s mouth and throat are treated with a solution for local anesthesia (usually lidocaine spray 10%). In exceptional cases, anesthesia is necessary;
- The patient should lie in a left lateral position with knees bent and relaxed;
- Remove dentures from the oral cavity, remove piercings
- The nurse will install a special mouthpiece/guide that you will clamp between your teeth or gums; it is needed to make it easier for you not to “close” your mouth during the procedure and will protect the expensive endoscope from damage during the examination
- For better visualization and smoothing out all wrinkles, a small amount of air or carbon dioxide is introduced through the endoscope.
What is gastroscopy
Gastroscopy is a type of study in which a visual examination of the gastrointestinal tract is performed. For these purposes, a special probe is used - a gastroscope, inserted into the stomach through the mouth. This is a flexible tube with a soft coating on the outside and fiber optics inside, designed in such a way as not to damage the internal organs of a person.
There are three types of gastroscopy:
- FGDS (Fibrogastroduodenoscopy ) . Examination of the stomach and duodenum.
- FGS (fibrogastroscopy ) . Stomach examination.
Which type of endoscopy will be required should be determined by the doctor during a preliminary consultation.
How is the endoscopy procedure performed?
During esophagogastroduodenoscopy, a thin flexible endoscope tube with an optical system (video camera) at the end is gradually guided from the mouth of the esophagus to the initial parts of the small intestine. Endoscopes equipped with a fiber optic system and lens transmit the image to an online monitor, which allows the doctor to immediately diagnose the condition of the subject. Then carefully remove the device.
Capsule gastroscopy differs in that instead of a probe, the patient swallows a plastic capsule containing a video camera (after 8 to 15 hours it is removed from the body naturally during bowel movements).
The duration of the procedure is determined individually. With local anesthesia, the procedure takes 7-10 minutes
.
With general anesthesia, the examination lasts about 30 minutes
.
IMPORTANT!
After endoscopy of the esophagus and stomach, it is not recommended to drink or eat for 30 minutes. After anesthesia/sedation, refrain from driving on this day.
Stages of endoscopy under anesthesia
Endoscopy under anesthesia includes three important stages - preparation, immediate implementation and subsequent recovery. The procedure must be carried out with the participation and supervision of an anesthesiologist. Consultation with this specialist is carried out before the study. The doctor determines the type and amount of anesthetic based on the patient’s health status. During the preliminary examination, the doctor also identifies the presence of contraindications to the procedure. The anesthesiologist then monitors the patient's condition during and after the procedure, until the patient fully recovers from anesthesia.
Before the procedure, depending on the age and health status of the patient, mandatory diagnostic tests are performed. Preparation includes the following steps.
- Examination before the procedure. Before endoscopy, under anesthesia, a general and biochemical blood test, a coagulogram (blood clotting test), the Rh factor is determined, a chest x-ray (fluorography) and an electrocardiogram are performed. In the presence of chronic diseases, consultation with specialized specialists and a therapist is necessary.
- 2 days before endoscopy under anesthesia, you should stop using aspirin, iron-containing and non-steroidal anti-inflammatory drugs (in consultation with your doctor).
- For 2-3 days before the study, you need to adhere to a gentle diet, avoid spicy, fatty, fried foods, sweets and alcohol. On the eve of the study, the last meal should be no later than 10-12 hours before the procedure.
- The day before the colonoscopy, you need to cleanse the rectum with laxatives.
- On the day of the examination, you should not smoke or take medications (as agreed with your doctor).
You should not drive after an endoscopy with sedation or anesthesia. After FGDS, you should not eat or drink for 1-2 hours. Subsequently, if you experience a sore throat, do not eat solid food.
How to prepare for gastroscopy?
Before undergoing gastroscopy, you need to follow some recommendations. It is advisable, first of all, to consult a specialist (gastroenterologist):
- Based on your medical history, he will determine indications or contraindications for gastric endoscopy. If necessary, he will prescribe additional tests for FGDS;
- Determine the type of anesthesia based on the patient’s response to certain medications;
- The doctor will find out bad habits that may affect the outcome of the endoscopy;
- Prescribe a diet before the procedure;
- The doctor will warn you about symptoms that may occur after the procedure;
- Will answer all your questions (for example, does it hurt).
Two to three days before the procedure, you should not eat spicy foods, smoked or fried foods. But lean meat, steamed, light soups with vegetable broths and porridges, on the contrary, are welcome. The bread should be slightly dry.
On the day of gastroscopy, if the procedure is scheduled for the first part of the day, you should not eat. And if in the second half of the day, then you can allow yourself a light breakfast (well-cooked porridge or cottage cheese is optimal for this), but no later than 8-10 hours before the test.
Particular attention should be paid to the drinking regime! Drinking is prohibited before the examination. And during preparation, alcohol, soda and coffee are excluded.
On the day of the study
In the morning on the day of the examination, in preparation for gastroscopy, do not drink, do not eat, do not smoke, brush your teeth without toothpaste, do not chew gum. The tablets you usually take should not be taken unless specifically directed by your doctor. All tablet preparations contain so-called fillers, such as chalk, which give the tablet its shape. When it comes into contact with the gastric mucosa, this filler swells and spreads over almost all parts of the stomach in the form of white smears, which will complicate a precise examination of the gastric mucosa or can even imitate erosive lesions of the mucosa. Therefore, regarding the morning intake of tablet drugs in preparation for gastroscopy, additionally consult with your doctor or endoscopist. Patients with bronchial asthma take an inhaler with them. Patients with diabetes are allowed, if necessary, sugar under the tongue.
On the day of the test, you can rinse your mouth with water.
What are the possible complications of gastroscopy?
If a Doctor prescribed a gastroscopy for you, then he analyzed your state of health and believes that with your state of health, the risks of complications are minimal (i.e., heart attack, stroke, and other serious “general” negative manifestations that can be provoked by the study are excluded)
Directly from the procedure itself, complications are extremely rare; possible complications during endoscopy of the stomach and duodenum include perforation (perforation) of organ walls and bleeding caused by trauma. But such side effects are extremely rare, and if you are properly prepared, do not regurgitate, and comply with all the requirements and commands of the endoscopist, then the risks are minimal.
As a rule, gastroscopy is prescribed during examination by a specialist doctor if there are complaints about the gastrointestinal tract, i.e. "on demand". some are forced to undergo “preventive gastroscopy” 2 times a year during periods of exacerbation of diseases and as part of a “dispensary examination” if this item is checked for your age. But if pathologies are detected, the gastroenterologist or attending physician prescribes this examination individually, depending on the severity of the disease.
If you care about maintaining your health, we recommend that you undergo gastroscopy and colonoscopy every 4-5 years, in the absence of pathology. Ask your endoscopist what interval he recommends for you!
Prepare a summary of your medical information for your appointment:
- Reason for visiting a doctor (this is where the conversation with the doctor begins).
- The statute of limitations of the complaints that are bothering you, the sequence of their occurrence, the presence of any diagnosis and the effectiveness of treatment earlier (ideally, you can provide all previous documentation, this will help the doctor restore the entire chronology of events).
- Concomitant diseases (not related to the gastrointestinal tract), as well as complaints not related to the gastrointestinal tract. remember if you have had any surgeries or injuries.
- Names of medications, vitamins, dietary supplements, combined oral contraceptives (COCs) (with dosage) that you have taken recently or are currently taking. You can take a photo of the packaging/blister.
- It would be good to know your height and current weight.
- Think about any allergies you have or have had.
- If alternative treatments have been used, tell your doctor (herbs and supplements, non-drug treatments).
- Think about how to answer the question about your usual diet and diet.
- Be sure to tell your doctor about other life events that affect your physical or mental health and your plans for the future (for example, you are planning a pregnancy, working in a stressful job or about to retire, planning to travel or a business trip).
Prepare questions for the reception in advance. Think about the problem in advance and write down questions as they arise. A few days before your appointment, review the questions and prioritize them. This list will be a useful tool for your doctor and will help you get the answers you need faster.
Breathing techniques
#1 – Call on the parasympathetic nervous system!

You can summon it with the help of breathing - short inhalation, slow exhalation. This technique will help you relax while inserting the endoscope into the oral cavity:
- We take a short breath through the nose to the count of 1 and 2.
- On the count of 3,4,5,6, we exhale slowly through the nose.
- Counting in your head will allow you to take your mind off a stressful situation and control your breathing.
- Try to track your breathing during the procedure and control it. And you won’t notice how the procedure ends!
Exhaling slowly helps slow your heart rate, which also creates a feeling of calm.
No. 2 – Square of Calm
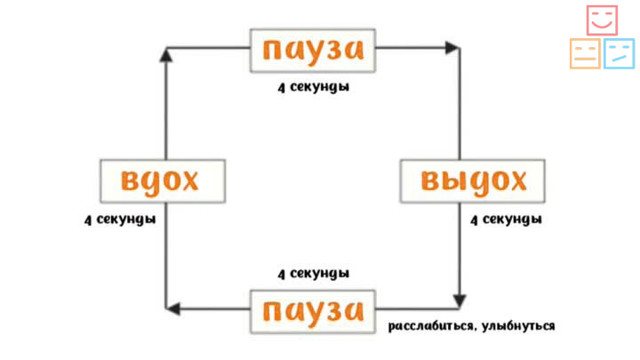
- You should start by taking a deep, leisurely breath through your nose. Mentally, a square appears before your eyes. The gaze turns to its lower left corner and moves towards the upper left corner for 4 seconds.
- Then we hold our breath and draw a horizontal line from the upper left corner to the right. We count down 4 seconds.
- We exhale for 4 seconds and look vertically from the upper right corner to the lower.
- And we finish drawing the square with our eyes for 4 seconds while holding our breath.
- Can be repeated throughout the entire procedure. If you do this exercise before the procedure. Drawing 5 squares is enough.
#3 – A place where I won’t be disturbed

Visualization of images helps to get rid of stress during FGDS and drive away bad thoughts. By creating an imaginary picture in your mind, you can go to a calm place and “wait out” the unpleasant procedure there.
Technique:
- To begin, close your eyes and inhale deeply through your nose, feeling your lungs fill with air.
- Next, without opening your eyes, you need to imagine yourself in any pleasant place, for example, in a forest grove, on the ocean shore or in the cozy living room of your own apartment.
- For better visualization, you need to use as many senses as possible: try to catch an imaginary smell, hear the sound of the surf, the rustle of leaves, feel the blow of the wind.
- During the procedure, you should concentrate as much as possible on the sensations created, while not forgetting to follow the doctor’s instructions.