Detailed description of the study
Bilirubin is a yellow-orange pigment. It is found in bile and in small amounts in the blood. Bilirubin is formed from heme during the destruction of red blood cells - erythrocytes.
Initially, an insoluble form, or fraction of bilirubin, which is also called indirect, appears in the blood. Once in the liver cells (hepatocytes), it is transformed through a chemical reaction into a soluble form (direct or bound) and is excreted in the same form in the bile. In the large intestine, with the participation of bacteria, the following chemical transformation of bilirubin occurs into a brown pigment (stercobilin), which gives the characteristic color to feces and is excreted from the body. Part of the bilirubin is converted back into indirect bilirubin and absorbed into the blood.
Liver diseases lead to metabolic disorders within hepatocytes, as well as to the destruction of these cells, which contributes to the entry of large amounts of bilirubin through the bloodstream into organs and tissues, into the skin and mucous membranes, which gives them a characteristic yellow color. At the same time, the concentration of this pigment in bile decreases. Its excretion through the intestines decreases, which is manifested by discoloration of stool. At the same time, darkening of the urine is noted due to the fact that the body seeks to remove excess bilirubin through the excretion of urobilin by the kidneys.
As a result of a violation of bilirubin metabolism, a person develops signs of jaundice: yellowing of the skin, mucous membranes and sclera of the eyes, darkening of urine and discoloration of feces.
The following types of jaundice are distinguished:
- Hemolytic (suprahepatic): increased breakdown of red blood cells;
- Parenchymal (liver): dysfunction of hepatocytes;
- Mechanical (subhepatic): violation of the outflow of bile.
However, a high level of bilirubin in the body is observed in many conditions associated with impaired functioning of hepatocytes and does not always lead to the development of jaundice. The reasons for the increase in its concentration may be the intake of alcohol, drugs toxic to the liver, fatty degeneration of hepatocytes.
Indications
- General screening when registering a patient for dispensary registration (including for pregnancy);
- Early diagnosis of hereditary and acquired liver diseases;
- Differential diagnosis of hepatic and obstructive jaundice;
- Monitoring the patient’s condition after acute intoxication;
- Treatment of alcoholic or drug-induced liver damage;
- Diagnosis of bile duct blockage and other bile outflow disorders;
- Diagnosis and treatment of diseases of the abdominal organs.
The interpretation of the analysis results is carried out by: urologist, nephrologist, gynecologist, therapist, family doctor, pediatrician, etc.
Treatment of elevated bilirubin
To normalize the level of bilirubin in the blood, it is necessary to eliminate the underlying disease. Your doctor may prescribe the following treatments:
- infusion therapy, during which saline solutions and glucose are introduced into the patient’s body;
- taking medications, including phenobarbital, if we are talking about the treatment of Gilbert's syndrome, and hepaprotectors - in the case when the cause of the inflammatory process is liver damage;
- phototherapy, which involves irradiating the body with special lamps;
- change in diet.
When it comes to treating hepatitis, it is aimed at eliminating the causative virus.
In what diseases is bilirubin excreted in the urine?
Considering the mechanism of penetration of various forms of pigment into urine, we can say that it is utilized by the kidneys only when excretion through the intestines is difficult or impossible. The reason for this state of affairs may be damage to liver cells, accompanied by a violation of the formation and movement of bile into the bladder, namely:
- parasitic, viral, bacterial, toxic hepatitis;
- autoimmune liver damage;
- hereditary diseases;
- cirrhosis;
- Dubin-Johnson and Rotor syndromes.
Diseases of the biliary system, in which the outflow of bile is disrupted, can provoke increased absorption of direct bilirubin:
- inflammation of the ducts (cholangitis);
- cicatricial changes in the tracts;
- GSD (cholelithiasis);
- tumors and cysts of the head of the pancreas;
- duodenal diverticula;
- hepatic artery aneurysm.
The appearance of bilirubin in the urine of pregnant women can be caused by congestion in the gallbladder, as a result of increased intra-abdominal pressure under the influence of the growing fetus. Such disorders are more often observed in the last trimester and are called cholestatic hepatitis. In children, the pigment can exit through the kidneys against the background of difficult outflow of bile due to congenital anomalies in the development of the bladder and ducts (kinks and torsions).
How does the substance get into the urine?
In complete health, bilirubin should not be detected in urine. Minor amounts are present, but are not detected by standard analysis. Active release of pigment through the kidneys (when its presence is confirmed by laboratory tests) always means an increase in the concentration of the direct fraction in the blood. Then, due to excess, the compound can penetrate the filtration system and leave the body with urine. The bound form is formed in the liver. This means that the pigment has already been neutralized and entered the bloodstream from the bile ducts (hepatic or cystic).
The concentration of free bilirubin can also increase sharply (which is especially noticeable during hemolysis). Even if the value goes off scale, the substance does not pass through the kidneys, since when it binds with albumin, too large molecules are formed that are unable to penetrate the pores of the filtration system. Detection of indirect bilirubin is possible along with elevated protein levels. This happens with renal failure and serious damage to the upper parts of the urinary system (which has its own symptoms, and therefore there is no question of finding the cause).
How to properly prepare for research
Minor bilirubinuria may indicate an incipient disease or appear due to improper preparation for the delivery of biomaterial. To avoid a false positive result, you must:
- before taking the test, do not eat food that changes the color of urine (beets, citrus fruits, carrots) for 1-2 days,
- stop eating foods with diuretic properties (watermelons) one day before,
- Before collecting urine, do not eat, smoke or drink liquids for 10-12 hours, and do not take physical procedures.
If you constantly take medications, then you need to stop taking the following medications for a day:
- diuretics,
- sulfonamides,
- barbiturates,
- oral contraceptives,
- steroids.
If it is not possible to stop taking the medications, then you need to inform the laboratory assistant. A note on the medication taken on the referral form will prevent false interpretation of the results.
A woman should not donate biomaterial during menstruation. Blood entering the urine and partial breakdown of red blood cells with subsequent release of bilirubin will lead to a false positive result.

To avoid incorrect testing data, urine should be collected 1-2 days after the end of your period.
Reasons for increased bilirubin
Bilirubinuria does not always indicate pathological processes. A moderate increase in bile pigment can be triggered by external factors or natural causes.
Physiological factors
Detection of traces of bilirubin in a newborn in the first week of life is considered normal. This is due to the breakdown of red blood cells that have passed from the mother’s blood to the baby before birth. Gradually, the baby’s hematopoietic system begins to work, and the release of pigment in the urine stops. Physiological jaundice is safe for health.
In adults and in children who have emerged from the neonatal period, physiological bilirubinuria does not develop. Detection of bilirubin in urine indicates a problem.
Diseases
In adults, an increase in bile pigment in the urine is often associated with liver pathologies. The reason may be:
- viral hepatitis,
- cirrhosis,
- liver failure,
- fatty hepatosis,
- liver tumors,
- infectious inflammations causing damage to hepatocytes (mononucleosis, brucellosis, leptospirosis),
- chronic intoxication with drugs or alcohol,
- obstruction of the bile ducts due to spasm or stone blockage.
Diagnostics and tests
To determine what is causing the increase in bilirubin, you need to undergo examination by a specialist. After a visual examination (checking the color of the skin, whites of the eyes, plaque on the tongue) and palpation of the abdominal cavity, the doctor prescribes laboratory diagnostics:
- BAC for the content of direct or indirect bilirubin;
- Aspartate aminotransferase and alanine aminotransferase assay;
- Ultrasound examination of the liver.
Blood sampling may be prescribed for a detailed clinical analysis.
Correct therapy can be prescribed only with an accurate diagnosis. In some cases, the help of an infectious disease specialist and gastroenterologist is required.
Other manifestations of bilirubinuria
Slightly increased bilirubin in the urine may not cause signs of deterioration in health. Only the color of urine changes - due to increased secretion of the bilirubin component.
Severe bilirubinuria, when the urine has a rich dark color, is accompanied by characteristic signs:
- yellowing of the sclera and mucous membranes,
- yellowness of the skin,
- dry and itchy skin,
- nausea,
- bitter taste on the tongue
- belching air,
- discomfort under the ribs on the right,
- increased fatigue,
- lightening of stool (up to complete discoloration),
- skin rashes,
- hepatic colic.

The appearance of these signs indicates that bilirubin, due to pathological abnormalities, cannot be excreted through the intestines and enters the urine in large quantities. The resulting condition requires medical examination.
In what cases is a urine test for bilirubin prescribed?
A general urine test can detect the bilirubin component. The test result is the reason for conducting specific studies, determining the amount of indirect and direct bilirubin in the urine and blood.
In addition to identifying elevated bilirubin levels, the reason for research is suspicion of the following diseases and conditions:
- hemolytic anemia,
- atrophic processes in the liver,
- poisoning with poisons that cause hemolysis (disintegration) of red blood cells,
- hepatitis,
- neoplasms in the pancreas,
- abnormalities in the functioning of the spleen (red blood cells are utilized in this organ),
- cholelithiasis,
- liver injuries,
- bile stagnation,
- obstruction of the bile ducts,
- metastasis to the liver or spleen,
- metabolic disorder (acquired or congenital),
- obstructive jaundice.
What to do
To distinguish liver diseases from lesions of the biliary tract, you need to take a closer look at the results of a urine test. The presence of bilirubin immediately indicates a malfunction in the hepatobiliary system; the urobilinogen pigment can be used to determine the exact location of the problem. If its level also exceeds the norm, liver cells are damaged. If the substance is within the reference values, changes in the biliary tract should be suspected.
Table - Norms of urobilinogen in urine
| Population category | Physiological indicator, µmol/l | Sign of diseases |
| Adults | 0‒35 | more than 40 |
| Children | 5‒10 | more than 10 |
To accurately determine the location of the bilirubin “leak,” doctors use data from a biochemical blood test. Hepatic pathologies are indicated by high values for direct and indirect fractions and aminotransaminases with normal levels of alkaline phosphatase. In diseases of the biliary tract, the increase in the level of direct bilirubin is so great that it accounts for more than 50% of the total amount of pigment, the level of alkaline phosphatase increases, and the values of ALT and AST remain normal.
Norm of bilirubin in urine in men, women and children
First, you should familiarize yourself with how bilirubin is indicated in a urine test. On some forms the Russian names of the components of urine are written, and sometimes the Latin abbreviation is used: bilirubin will be designated as BIL.
If the permissible norm in an adult’s blood is up to 17 mmol/l, then in the urine these indicators will be much lower.
The norm of bilirubin pigment µmol/l is:
- urobilinogen – 0-35,
- direct bilirubin – 0-8.5.
The indicator does not increase in women during pregnancy.
In children, there should be no direct bilirubin in the urine, and the amount of urobilinogen in daily urine should not exceed 5-10 mg/l.
Negative urine bilirubin indicates that the liver is healthy and the kidneys are fully filtering urine. But at the same time, the amount of urobilinogen should not exceed normal values.
Self-determination of bilirubin in urine
You can purchase test strips from the pharmacy chain and do a urine test yourself. Complex tests are sold that determine almost all urine parameters, and simple testers that detect only bilirubin and urobilinogen.
Test strips are sold in tubes with a test scale painted on the surface of the jar. It’s easy to do your own research:
- open the package,
- collect fresh urine (biomaterial cannot be stored for more than 2 hours),
- take out the tester without touching the place where the indicator is applied,
- dip the tip with the applied reagents into the liquid for 3-5 seconds,
- tap the strip on the edge of the jar to remove excess urine,
- place on a horizontal surface.
You will have to wait for the result from 30 seconds to 3 minutes (the time depends on the nature of the reagent and is indicated in the annotation). After the chemical reaction is completed and the indicator changes color, you need to evaluate the result using the scale drawn on the tester container.
Standards for general urine analysis
The protocol for a general study of urine reflects all its qualitative and some quantitative characteristics. The analysis evaluates the color, consistency of the liquid, and the presence of inclusions. Detailed information about the composition is obtained by carrying out biochemical reactions, studying physical properties and examining samples under a microscope. What the values should be for a healthy person can be seen below.
For more details about all the indicators of OAM and the reasons for deviations, read the article “General urine analysis - norm and interpretation, table explaining all positions.”
Table - Standards for general urine analysis
| Index | Norm |
| Color | Straw to dark yellow |
| Smell | Characteristic, unsharp |
| Transparency | Absolute |
| Acidity | 5,0‒7,0 |
| Protein, g/l | 0,0‒0,03 |
| Glucose, mmol/l | 0,0‒1,0 |
| Ketone bodies, mmol/l | 0,0‒0,5 |
| Bilirubin, µmol/l | 0,0‒8,5 |
| Urobilinogen, µmol/l | 0,0‒35 |
| Hemoglobin | Absent |
| Bacteria | None |
| Red blood cells | 0‒2 in field of view |
| Leukocytes | 0‒5 in field of view |
| Epithelium | 0‒5 in field of view |
| Cylinders | 1–2 hyaline in the field of view, others absent |
| Crystals | are discovered |
| Yeast mushrooms | None |
| Parasites | None |
The quantitative content of bilirubin is reflected only by laboratories that have modern electronic equipment for studying urine. The analysis form may also indicate “absent,” which means detection of less than 8.5 µmol/L of the substance. Children, including newborns, should not have pigment in their urine. If the analysis protocol shows its presence or 9.0 µmol/l bilirubin, you need to look for the reasons, since such values mean pathology.
The pigment is detected by performing the following tests:
- Rosina - 2 ml of urine is placed on a glass slide, a layer of alcohol solution of iodine (1%) is applied, the formation of a green ring means a high concentration of bilirubin;
- Fouche - urine is mixed with a 15% barium chloride solution, the mixture is passed through a filter with Fouche's reagent, the appearance of green crystals means the presence of pigment.
Indications for analysis
A general urine test is prescribed as a diagnostic and preventive examination. Thanks to it, you can quickly assess the functioning of vital systems and characterize the functions of the urinary tract. A urine test for bilirubin is necessary if you suspect:
- atrophic processes in the liver;
- hepatitis;
- neoplasms;
- lesions of the spleen;
- pancreatic diseases;
- metabolic disorders;
- gallstone disease.
Be sure to study urine if there are signs of a hemolytic process, intoxication, or after abdominal injuries. The analysis is regularly prescribed to patients with cancer pathologies for the early detection of metastases in the liver and kidneys.
False Positives
Because tests for the presence of bilirubin are not very accurate, incorrect information may be obtained. In order for the analysis result to correspond to the real state of affairs, it is necessary to prepare for it and correctly collect the biomaterial. Preparatory activities include:
- eliminating stress and excessive physical activity;
- avoiding alcohol and foods that color urine (carrots, beets, citrus fruits, watermelons) 2 days before the test;
- refusal of diuretics on the eve of biomaterial collection.
If a person regularly or as a course of treatment takes drugs from the group of barbiturates, sulfonamides, oral contraceptives, or steroids, this must be reported to the medical staff who collects the biomaterial (so that the appropriate note is made), or to the doctor who will study the test results.
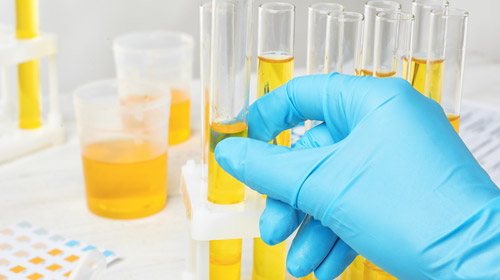
To properly collect urine for an adult, you need to purchase a sterile container from the pharmacy. For small children, polyethylene urinals are used, from which urine is poured into a cup. It is not advisable to reuse food cans for testing. The procedure for collecting biomaterial is as follows:
- The morning portion of urine excreted shortly after waking up is subject to collection;
- before bowel movement, the patient should not eat or drink anything other than water;
- Before urinating, hygiene procedures should be carried out (wash with warm water, without using soap);
- collect only the middle portion of urine (the initial and last ones are not needed);
- The container is tightly closed with the supplied lid;
- The biomaterial is taken for analysis within 2 hours.
It is necessary to ensure that the container with urine is stored at room temperature or in the refrigerator door, and not exposed to direct sunlight, high or low temperatures. Due to these factors, the properties of the material may change and the analysis result may be inaccurate.