The test for syphilis is negative - the result that most patients undergoing testing for infection with this dangerous infectious pathology hope for.
Many patients, having seen the expected result in the column, stop worrying about their health and noticing alarming signs and symptoms.
This action is wrong.
After all, there are cases when the indicators turn out to be far from the truth.
What does it mean if the test for syphilis is negative, do patients ask their doctors, and when is testing for Treponema pallidum generally prescribed?
How to prevent infection if you had unprotected sexual intercourse, and how to behave if the results are positive?
Detailed description of the study
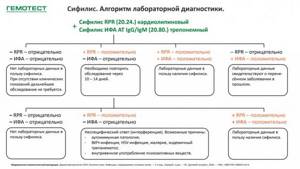
Syphilis is an infectious disease caused by Treponema pallidum. Transmission of infection occurs primarily through sexual contact without the use of barrier contraception. However, it is possible to become infected with treponema pallidum through contact and household contact if personal hygiene rules are not observed, as well as transmission of the pathogen from mother to child during childbirth or breastfeeding. Syphilis can affect any organs and systems. In the absence of timely treatment, the disease becomes chronic. Initially, a hard chancre is formed at the site of contact with the source of infection - a painless ulcer with a small amount of transparent content on the surface. Often the body reacts to the introduction of the pathogen by inflammation of the lymph nodes located near the site of the lesion. Within a few weeks, a scar forms in place of the chancre. However, the disease does not recede, and after some time the infected person notices the appearance of a specific rash on the body - the appearance of small bright pink spots (rosacea rash). This stage is called secondary syphilis. The disease is prone to periodic exacerbations with changes in the nature of the rash. Tertiary syphilis is the result of untimely diagnosis and treatment of this disease. Along with the formation of nodes and tubercles on the skin, which are called gummas, prone to ulceration and scarring, damage to internal organs is observed. Diagnosis and treatment of syphilis is carried out by a dermatologist. To confirm the diagnosis, a modern test for determining rapid plasma reagins, or RPR test (Rapid Plasma Reagins), is used. These proteins are antibodies to the lipid components of cells destroyed by the pathogen.
Deciphering blood for syphilis
Interpretation of the ELISA blood test for syphilis
ELISA is one of the most popular methods for diagnosing syphilis.
This study is inexpensive and effective.
It can be used as a confirmatory method in the case of a positive RPR.
ELISA is one of the treponemal tests.
During the study, antibodies to the pale spirochete are determined.
Immunoglobulins of two classes are detected: IgG and IgM.
Positive test results may not be available earlier than 20 days after infection.
Usually a quantitative analysis is performed to determine the antibody titer.
Possible results:
- positively;
- negative;
- doubtful.
A positive test does not always indicate that the patient has syphilis.
Possible reasons for false positive results:
- pregnancy;
- autoimmune pathologies;
- cancer;
- liver diseases;
- past history of syphilis.

If a false positive result is suspected or the test result is questionable, other tests for syphilis are performed.
These can be either treponemal (TPGA) or nontreponemal (RPR) tests.

Decoding RPGA for syphilis
When performing RPGA, qualitative or semi-quantitative determination of antibodies is usually used.
In qualitative research there can be two types of results:
- positive;
- negative.
Results may not be positive until 2 months after infection.
In most cases, they remain positive throughout life after the disease is cured.
Semi-quantitative research is more informative.

Decoding a blood test for syphilis RPGA using a semi-quantitative method includes an indication of the antibody titer.
There are three possible results:
- An antibody titer above 1:640 indicates infection with syphilis;
- an antibody titer of less than 1:640 indicates a previous illness;
- the absence of antibodies indicates that the person is healthy.
Diagnostic tactics for suspected syphilis may differ significantly in different clinical situations.
Contact our clinic if you have symptoms suggestive of this disease.
We can take any tests for syphilis: screening or confirmatory.
An experienced doctor will interpret the research results.
If the result is positive, you will be prescribed treatment that will cure syphilis in a short time.
If you suspect syphilis, contact the author of this article, a venereologist in Moscow with 15 years of experience.
Indications for the study
The reason for issuing a referral for appropriate analysis may be situations that include:
- ordinary examination for registration of a health record (mainly applies to civil servants, teachers, cooks, doctors and sellers);
- having refugee or homeless status;
- preparation for surgery;
- urgent hospitalization;
- HIV (human immunodeficiency virus);
- establishing the fact that the patient lives with a person suffering from syphilis;
- mandatory screening at an early stage of gestation;
- drug addiction;
- checking a potential donor;
- diagnosis at the end of the main course of treatment for a sexually transmitted disease;
- clarification of the condition of a newborn when the causative agent of syphilis is identified in his mother.
It is also necessary to donate blood for bladder cancer if characteristic symptoms of a dangerous infection are detected, the most obvious are:
- elevated body temperature (37-38.5°C), persisting for a long period of time;
- periostitis of the jaw or gumboil (inflammation of the gum area, accompanied by swelling, as well as painful sensations when pressed);
- a combination of general weakness with cough and runny nose;
- regular pain in muscles and joints;
- erythematous tonsillitis (formation of purple spots on the mucous membrane of the throat);
- local baldness;
- large purplish-purple condylomas (growths);
- dense chancre (hard ulcers with a dense depression and smooth edges);
- conjunctivitis;
- causeless loss of appetite and insomnia;
- dark convex formations on the feet and palms, sometimes resembling blue-red calluses;
- roseola (a type of eczema characterized by the appearance of pale pink, painless spots on the surface of the skin);
- ecthyma (deep wounds with purulent discharge);
- multiple pustules with white heads.
An equally important sign of syphilis is the formation of papules of 2 types: pinkish, smooth elevations of the epidermis with a shiny surface and bluish growths with dry scales near the edges. Terminal symptoms of the disease - gumma - are extremely rare. They are violet-cherry granulomas located in almost all human organs and tissues.
Gummas actively destroy segments of the body, promoting the growth of necrotic foci, as well as scarring. If a person wishes to self-test for syphilis without having obvious symptoms, doctors will be required to write a referral for a laboratory blood test.

Another symptom of infection is the “necklace of Venus” or leucoderma (the appearance of non-pigmented light spots localized in the chest, neck and collarbones)
What does the microprecipitation reaction show?
At the stage of primary syphilis, the body produces antibodies. During analysis, a cholesterolized extract from bovine heart muscle tissue is added to the biomaterial. Its structure is similar to the antigen of the pale spirochete, the causative agent of the infection.
If the blood contains antibodies, a reaction occurs - a precipitate appears in the form of white flakes.
Microprecipitation is a screening test for syphilis. Based on the results of the analysis, the doctor will know whether the patient has an infection or not. Testing RMP for syphilis helps:
- identify the disease at an early stage;
- carry out prompt diagnosis of a large number of patients;
- monitor the effectiveness of treatment;
- adjust the dosage of medications.

Total antibodies to Treponema pallidum: explanation
A positive reaction to antibodies to Treponema pallidum indicates different clinical stages of syphilis (primary, secondary, latent). Also, a positive test result for total antibodies to Treponema pallidum may persist for some time after a course of treatment for syphilis (“serological scar”).
The test result is negative in the absence of infection or early primary syphilis.
The test for total antibodies to Treponema pallidum may have an equivocal result. Then a repeat analysis for total antibodies is carried out a couple of weeks later.
Methods of conducting research
To perform RMP analysis, the biomaterial can be blood taken from a vein, finger, or cerebrospinal fluid. Before this, it is not recommended to drink alcoholic beverages, fatty or fried foods the day before. Blood should be donated on an empty stomach. The microprecipitation reaction is determined in several ways:
Article on the topic: Umbilical hernia in adults - causes and treatment methods
| Type of dough | Execution feature |
| With macroscopy | Carry out without equipment, precipitation under the influence of the reagent is observed with the naked eye |
| With microscopy | Antibodies are detected using a light microscope; no additional substances are required |
| With a quantitative indicator | With serial dilution of the test material, the number of antigen-antibody complexes is determined |
Preparation and delivery
Recommendations: blood test for breast cancer, how to take it? The following preparation is required:
- Blood donation is carried out on an empty stomach;
- A day before the analysis, a ban is imposed on the consumption of fried, smoked, spicy, salty and alcohol-containing foods;
- It is necessary not to undergo physical overload the day before donating blood;
- The patient is obliged to inform the doctor about the presence of diseases, deterioration in health and about taking medications
Where is blood taken for RMP analysis? To conduct research, blood is taken from a vein.

Venous blood is taken for examination
Why get tested for HPV
Cervical cancer is a disease with a proven viral etiology. Its causative agent is the human papillomavirus (HPV), an infection transmitted primarily through sexual contact. However, the more specialists accumulate knowledge about the nature of this disease, the more myths and misconceptions accumulate among the population. Today we’ll try to figure out what to believe and what not – and at the same time answer the most frequently asked questions about HPV.
Human papillomavirus - what is it?
First of all, it's a virus. Like all other viruses, it penetrates the cell, declares itself the local ruler and sets up a factory from the cell to produce its beloved self. These viral copies penetrate neighboring cells and take control of them in the same way.
Researchers have now identified more than 150 different types of HPV. Some of them cause small, harmless papillomas on the skin, and about 40 varieties prefer the tissue of the genital organs.
HPV is a highly contagious virus, easily jumping from person to person during any form of sexual contact, including petting. Due to its high contagiousness, almost every sexually active woman will be diagnosed with HPV at least once in her life.
What will happen to me if I am diagnosed with HPV?
Since HPV prefers to “settle” in the cells of stratified squamous epithelium, which is constantly renewed and exfoliated, in most cases no disease develops.
But if something goes wrong, HPV manages to integrate into the genome of the host cell and says: “I’m in the house.” From this moment on, the immune system ceases to recognize HPV, and the development of the disease begins. Which one depends on the specific type of HPV.
Some viruses are considered low-oncogenic and cause the development of genital warts (anogenital warts) in the genital area. These growths can appear on the skin and mucous membranes of the genital organs in men and women, around the anus, on the rectal mucosa or on the cervix in women. The most common low-oncogenic types are HPV-6 and HPV-11.
Genital warts can look very ugly, sometimes even scary, but they are easy to remove with the help of medications (not on your own! There may be such a chemical burn that it doesn’t seem like much) or surgical methods (cryotreatment, radio waves, laser or electrosurgery).
Highly oncogenic types of HPV (at least 14 different types) slowly but surely “enslave” all layers of the epithelium and penetrate deeper. This process does not manifest any symptoms at all, develops very slowly, but almost inevitably leads to the development of cancer of the cervix, anus and rectum, vagina, penis, mouth and throat. The most dangerous and “evil” types are HPV-16 and HPV-18.
How is HPV infection treated?
Whether you like it or not, attempts to treat HPV infection with all sorts of magical immunotropic drugs, extracts of potatoes, broccoli and some kind of flies are a waste of money.
You can find hundreds of domestic publications and studies telling how amazingly these medicines “work”. The problem is one thing - no one can claim that the virus is defeated by the pill, and not by the body’s own work. In women under 30 years of age, spontaneous clearance of HPV occurs in most cases.
If the virus has entered the integrative phase (into the “house”) and the development of an HPV-associated disease has begun, treatment can only be surgical. If these are genital warts, they must be excised; if this is a precancerous lesion of the cervix (CIN - cervical epithelial neoplasia) - the entire area of the lesion (the doctor sees this place through a colposcope) must be removed.
What can I do to prevent the disease?
The principles of protection are the same as for other infections transmitted primarily through sexual contact. However, even constant and correct use of condoms does not exclude infection (HPV is highly contagious), although it significantly reduces the risk.
The onset of the disease caused by HPV is possible within 8–10 years from the onset of sexual activity, but in order to identify the initial signs of the disease, it is necessary not only to go to the gynecologist, but to undergo cervical screening: a cytological smear from the cervix from the age of 21 (not less than once every 3 years) and analysis for HPV of high carcinogenic risk from the age of 30 (at least every 5 years)1.
Debate has been going on for many years about at what age it is advisable to start HPV testing. In our country, they decided to add an HPV test to cytological screening from the age of 30, and in some countries, including the USA2, from the age of 25. But experts are unanimous on one thing: in young patients, HPV is detected in 90% of cases and leaves the body as quickly and easily as it is colonized. Therefore, there is no need to start testing too early - there will be a lot of unnecessary movements, tears and pointless attempts at treatment.
Does correct diagnosis guarantee protection against cancer?
It is important to understand: screening is good, but not ideal. Of course, the opportunity to catch cervical cancer in its pre-stages is a magical chance given to humanity by Georgios Papanicolaou, but there are many different “buts”.
The analysis must be taken well, transported carefully, colored correctly, viewed correctly - and at each of these stages, errors can, unfortunately, occur. In any case, the task of screening is to “catch” an already started disease at the stage of early, still precancerous, changes in order to cure it as quickly as possible.
But there is a second strategy - vaccine prevention, the task of which is to prevent infection at all. And we’ll talk about the possibilities of preventing HPV-associated diseases through vaccination next time.
Oksana Bogdashevskaya
Photo istockphoto.com
1 Benign and precancerous diseases of the cervix from the perspective of cancer prevention. Clinical recommendations (treatment protocol). Letter from the Ministry of Health of the Russian Federation dated November 2, 2017.
2 Society of Gynecologic Oncology (SGO) and the American Society for Colposcopy and Cervical Pathology (ASCCP): Interim clinical guidance for primary hrHPV testing 2015
What is RMP?
RMP means a blood microreaction to the so-called cardiolipin antigen (bovine heart muscle extract), which is close in nature to the causative agent of syphilis. When a special antigen is introduced into a sample containing a patient’s biomaterial, a response is checked. If in the body of the person being examined, the immune system has formed antibodies (protective proteins) to the virus itself, then they will react to a similar reagent.
The pathogenic microorganism that causes syphilis in humans is Treponema pallidum. This single-celled bacterium is a spirochete (Greek for “curled hair”). Outwardly, it resembles an ultra-thin spirally twisted ribbon without any outgrowths. The microprecipitation reaction in laboratory diagnostic results can be called not only RMP, but also PRP or VDRL. During the procedure, blood is drawn from a vein.

This is what Treponema pallidum, the causative agent of syphilis, looks like
Bibliography
- Ageev F.T., Skvortsov A.A., Mareev V.Yu., Belenkov Yu.N. Heart failure against the background of coronary heart disease: some issues of epidemiology, pathogenesis and treatment. RMJ 2000; 8:15-16.
- Andreev D.A., Batishchev P.N. Some aspects of the practical use of brain natriuretic peptide for diagnostic purposes. Bulletin of the Scientific Center for Agricultural Sciences named after. A.N.Bakuleva RAMS 2004; 3: 146-155.
- Andreev D.A., Mazerkina I.A., Gitel E.N. et al. Changes in brain natriuretic peptide in the treatment of decompensated chronic heart failure. Creative Cardiol 2007; 1-2: 136-142.
- Andreev D.A., Rykova M.S. B-type natriuretic peptides in heart failure. Klin Med 2004; 6:4-8.
- Ballezyuk M.F., Grinenko T.N., Kvetnoy I.M. Heart hormones in the formation of cardiovascular pathology. Klin Med 2005; 11:4-12.
- Bugrimova M.A., Savina N.M., Vanieva O.S., Sidorenko B.A. Brain natriuretic peptide as a marker and prognosis factor in chronic heart failure. Cardiology 2006; 1:51-57.
- A. L. Vertkin, D. B. Saprygin, V. A. Moshina Brain natriuretic peptide in acute coronary syndrome without ST segment elevation. Medical scientific and practical journal “Attending Physician”, No. 6. 2006.
- Golukhova E.Z., Eremeeva M.V., Polyakova E.S., Bockeria L.A. Use of natriuretic peptide precursors in the diagnosis of heart failure of ischemic etiology before and after coronary artery bypass surgery. Creative Cardiol 2004; 3: 156-161.
- Eliseev O.M. Natriuretic peptides. Evolution of knowledge. Ter Arch 2003; 9:40-45.
- Adams KF, Mathur VS, Gheorghiade M. et. al.B type natriuretic peptide from bench to bedside. Am Heart J 2003; 145:34
- Ala-Kopsala M., Magga J., Peuhkurinen K. et al. Molecular heterogeneity has a major impact on the measurement of circulating N-terminal fragments of A- and B-type natriuretic peptides. Clin Chem 2004; 50: 1576-1588.
- Anand I., Fisher L., Chiang Y. et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the valsartan heart fealure trial (Val-HeFT). Circulation 2003; 107: 1276-1281.
- Clerico A., Emdin M. Diagnostic Accuracy and Prognostic Relevance of the Measurement of Cardiac Natriuretic Peptides: A Review. Clin Chem 2004; 50: 33-50.
- Darbar L., Davidson N., Gilleepie N. et al. Diagnostic value of B-type natriuretic peptide concentration in patients with acute myocardial infarction. Am J Cardiol 1996; 78: 284-287.
- Davis M., Richards A., Nicholls M. et al. Introduction of metoprolol increases plasma B-type cardiac natriuretic peptides in mild, stable heart failure. Circulation 2006; 113:977-985.
- Fleisher D., Espiner E., Richards G. et al. Rapid assay of plasma brain natriuretic peptide in the assessment of acute dyspnoea. NZ Med J 1997; 110: 71-74.
- The Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heartand great vessels. 9th ed. Boston, Mass: Little, Brown & Co; 1994:253-6.
- American Heart Association. 2000 Heart and Stroke Statistical Update. Dallas, TX: American Heart Association;1999:18-19.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician