Growth hormone (somatotropic hormone, STH) belongs to the category of pituitary hormones. Analysis for growth hormone is necessary in the diagnosis of many diseases, as well as to confirm the initial diagnosis.
Click to make an appointment, ultrasound or tests
DETAILED INFORMATION ABOUT THE ANALYSIS FOR GROWTH HORMONE HGH
This substance is produced in the anterior lobe of the pituitary gland, the name is explained by the fact that this element is responsible for the growth sites in the bones of adolescents and children.
Growth hormone not only has a direct effect on human growth, but also:
- has an anabolic effect (increases formation, slows down protein breakdown);
- accelerates the breakdown of fat (this makes it possible to increase the ratio of adipose tissue to muscle mass);
- controls carbohydrate metabolism (increases the concentration of glucose in human blood);
- ensures calcium uptake by bone tissue.
PITUITARY Gland – main endocrine gland
One of the first questions I am always asked is what the pituitary gland is.
The pituitary gland is naturally the main endocrine gland, which is located at the base of the brain and therefore surgeons, when operating transnasally, do not affect the brain. They go directly to the pituitary gland.
The pituitary gland itself consists of two parts: the anterior lobe and adenohypophysis, where the main hormones are secreted, and the posterior lobe, which is a reservoir for storing hormones such as isopresin. And the lack of which leads to thirst and frequent urination.
Figure 1. MRI of the pituitary gland is normal.
Here on the slide there is a normal MRI of the pituitary gland, this is a fast image, here the pituitary gland is highlighted in green. We see a thin strip from above - these are the optic nerves, this is the pituitary stalk, and around next to the pituitary gland on one and the other side - these are dark circles - these are the carotid arteries, the internal carotid arteries, the largest arteries that feed the brain.
To whom and for what purpose is the analysis prescribed?

The level of somatotropic hormone reflects the performance of the pituitary gland, and also helps to identify the cause of various types of disorders.
- One of the possible options for assigning this analysis, as you already understood, is to assess the functioning of the pituitary gland.
- Also, the level of the hormone in the blood allows you to confirm or refute the pathology of deficiency or excess of somatotropin. Most often, the pathology occurs in children who urgently need growth hormone. Therefore, this indicator is an important part of the overall diagnostic process.
- Additionally, with the analysis of somatotropin, a study of insulin-like growth factor is prescribed, which more accurately reflects the concentration of growth hormone in the blood.
STH (somatotropic hormone, growth hormone)
HGH or growth hormone are all synonyms for the same name.
Produced in the anterior lobe of the pituitary gland by somatotropic cells.
We know very well that the main effect of this hormone in children is to accelerate growth.
In children and adolescents, it causes acceleration of linear (lengthwise) growth
, mainly due to the growth of long tubular bones of the limbs.
But in adults this hormone also plays an important role.
:
- it is involved in bone metabolism,
- improves calcium absorption by bones,
- promotes fat burning,
- improvement of muscle mass.
This is such a powerful anabolic hormone that athletes love to use to increase muscle mass, and, in general, increase muscle strength.
We know and see perfectly well the manifestations of acromegaly and gigantism in athletes
. When the disease manifests itself in people at a young age, when the growth plates are not yet closed, this ensures high growth and good muscle mass. And the first symptom of acromegaly contributes to the fact that these people achieve high achievements in sports. But, of course, if this disease is not treated, then in the future all this leads to damage to the joints, cardiovascular system and disability of patients.
The vast majority of cases of acromegaly are associated with
a pituitary adenoma
, a benign tumor of the pituitary gland that produces growth hormone. Globally, the prevalence is 40-60 cases per million adults. In Russia there are only 30 cases, which is probably due to the low diagnosis of this disease in our country.

Figure 2. Patients in whom the disease manifested at an early age
In Figure 2 we see young people in whom the disease manifested itself at a young age - these are sons with their fathers. And next to me stands a patient with acromegaly, whose disease also manifested itself at a young age, but only at the age of 50 was he diagnosed, unfortunately, as severely disabled, with damage to the joints and cardiovascular system.
Everyone is well aware of the external manifestations of acromegaly.
:
- nose enlargement,
- swelling,
- large lips,
- enlargement of the tongue, sometimes the tongue does not fit in the patient’s mouth,
- discrepancy of teeth,
- large hands and feet.
And sometimes it is quite difficult to determine when these changes in appearance appeared. The patient sees that changes are occurring, but usually he believes that these are age-related changes. All the people around, relatives, acquaintances, they also perceive these changes as some kind of age-related changes. Therefore, it is quite difficult to say when the disease actually manifests.
We usually ask this question: When did you wear your wedding ring when you stopped putting it on your finger? The patient tells me: “I wore it, but at the age of 36 I took it off and could no longer put it on.” Or when you first got gaps between your teeth.
Figure 3. Patient with acromegaly
Here in Figure 3 is our patient who provided me with her photographs. And despite the fact that in young people the disease still progresses faster, it is quite difficult to say. The girl is 7 years old, 12, 20 and at 26 years old we already see manifestations of acromegaly, we see swelling, a large nose.
Figure 4. Patient after surgery
And now, a month and a half after the tumor was removed in our center, we see an improvement in the condition, a decrease in swelling.
According to the literature, the average time from the onset of the first signs to diagnosis is 8 years
. It has been 8 years since the patient first developed symptoms and when he was diagnosed. Therefore, this is a fairly long period of time when various complications of acromegaly are already developing.
Methods for determining STH
You can directly examine the level of growth hormone in the blood using an enzyme immunoassay. However, this method does not allow one to reliably determine the following: is there a deficiency or excess of the hormone?
For more accurate diagnosis, additional tests (samples) are used.
Test with clonidine or insulin
Both of these substances stimulate the secretion of growth hormone. In accordance with the chosen stimulant substance, blood is taken at certain intervals. Normally, after stimulation, the concentration of somatotropin in the blood will be more than 10 ng/ml. If the level of the hormone does not increase, this indicates its deficiency in the body.
Somatomedin
Somatomedin C , or insulin-like growth factor, as mentioned earlier, is an indicator of the effect of growth hormone on cells. Its concentration does not change throughout the day, which makes it possible to judge the secretion of somatotropin with high accuracy. A low concentration of somatomedin indicates a lack of growth hormone.
The level of insulin-like growth factor in the blood is 150 – 300 ng/ml. This indicator is often used to monitor the treatment of dwarfism and acromegaly.
Symptoms of acromegaly

Figure 5. Symptoms of acromegaly
Here in Figure 5 we see that these are not only the external changes that we talked about.
Changes occur in all internal organs
, the heart enlarges, the liver enlarges, the kidneys enlarge. Patients develop enlarged thyroid glands, diffuse goiter or nodular goiter. Patients develop breathing problems, respiratory dysfunction, and nighttime sleep apnea. The patient develops arthritis and all this leads, unfortunately, to the patient’s disability.
Systemic manifestations of acromegaly

Figure 6. Systemic manifestations of acromegaly
Figure 6 shows systemic manifestations, the most common are lesions of the cardiovascular system, a large heart, and diastolic dysfunction. This is joint damage. We see that any joints can be affected, mainly large joints. This is the risk of various formations, additional tumors, which I will talk about later. And impaired carbohydrate metabolism and the development of diabetes. In addition, this is a decrease in the function of the pituitary gland, the appearance of hypopituitary signs, this is adrenal insufficiency. This is a decrease in thyroid function. This is a violation of menstrual function in women and erectile function in men. And lung damage in the form of respiratory dysfunction and sleep apnea.
Figure 7. Regulation of somatotropic function of the pituitary gland
In Figure 7, I will briefly tell you about the regulation of somatotropic function. The pituitary adenoma secretes somatotropic hormone. It affects the liver, and insulin-like growth factor-1 or somatomilin-C is formed in the liver, this is also a synonym for this factor, which, in principle, determines the main effect, the main effects of acromegaly.
Who to contact for help
The patient is usually sent for examination by a doctor, having some reason for this. Therefore, it is better to contact the specialist who referred you with answers. This could be an endocrinologist, oncologist, therapist or pediatrician.
If you yourself decide to go to a paid clinic to determine the level of somatotropic hormone in the blood, then, if deviations from the norm are detected, you should contact a therapist or pediatrician (if the patient is a child).

Diagnosis of acromegaly
Currently, the diagnosis of acromegaly is based on the determination of insulin-like growth factor-1 and the study of growth hormone, during glucose, 5 points are taken before taking 75 grams of glucose and for 2 hours every half hour. And these two tests are the gold standard for acromegaly all over the world.
And if the patient has diabetes, then we cannot perform this test on them, but this patient can take 5 points, also within 2 hours with an interval of 30 minutes. And its own hyperglycemia, an increase in sugar, is an analogue of this test.
Why don't we use STH level as a marker.
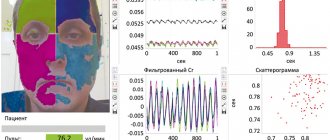
Figure 8 Growth hormone secretion
And in Figure 8, I hope you can see that the green graph is the secretion of growth hormone in a healthy person, and the red graph is in a patient with acromegaly. And we see the circadian rhythm in both a healthy person and a patient with acromegaly. And we can actually draw blood and see high levels of growth hormone in a healthy person and lower levels in a patient with acromegaly. Therefore, we cannot make a diagnosis based solely on the basal level of GH.
Advantages of IRF-1 as a diagnostic marker compared to GH
Insulin-like growth factor, unlike growth hormone, is not subject to such circadian fluctuations.
This is a constant value.
And even a slight increase in growth hormone can be accompanied by high levels of IGF-1.
In addition, this study can be performed at any time, regardless of food intake. That is, we can take blood from a patient after meals, in the morning, during the day, and in the evening. Usually in the morning. And this will not affect the result.
This indicator is the most important and reliable marker for both diagnosis and monitoring of treatment of acromegaly.
Reasons for the “false” decrease in IRF-1
Could there be a false decline? Yes, there may be a false decrease in IGF-1.
- This is uncompensated diabetes mellitus. Very high sugar levels. In these cases, the study must be repeated after compensation of carbohydrate metabolism is achieved.
- In addition, the use of oral estrogens by women, these can be contraceptives, this can be replacement therapy, which includes female sex hormones, estrogens, can lead to a slight decrease in the level of IGF. But usually this occurs in those patients who initially do not have a high level of this IGF.
- And, of course, it is recommended to conduct research in one laboratory, because we have also encountered the fact that it is very difficult to evaluate different results, different laboratories, especially when we prescribe some kind of treatment, we see IRF before treatment in one laboratory and in a completely different one already in another laboratory. It is very difficult to evaluate these results. Therefore, of course, I would like it all to be from the same certified laboratory.
Latest Russian and international recommendations published in 2014.
And this year new Russian recommendations are being prepared. I hope they will be published on the diagnosis and treatment of acromegaly, i.e. it is a document for physicians on which we all rely when diagnosing and treating our patients.
At present, I repeat once again, insulin-like growth factor must be examined in all patients who have been diagnosed with a tumor
, even if they do not have any typical manifestations of acromegaly. And now we are often faced with such a situation. MRI has become generally available and patients themselves who have headaches turn to centers, MRI centers. An MRI is done, a pituitary tumor is found and, naturally, after that they turn to endocrinologists. Such a patient should undergo an IGF-1 study. Naturally, if the patient has typical clinical manifestations of acromegaly. And if there are no external manifestations, but there is a combination of several symptoms. This is either sleep apnea syndrome, or diabetes, or carpal syndrome, i.e. pain and numbness in the fingers. This increased sweating, increased blood pressure, joint pain, a combination of several symptoms is a mandatory indication for the doctor to rule out acromegaly.
Once again, STH should not be routinely examined in all patients.
, we only look at the STG during the test.
What does preparation include?
Preparing for a blood test for growth hormone is very simple; the patient only needs to scrupulously follow the following simple rules. So, before the tests
The following requirements must be met.
- If approximately 3-5 days before the blood test the patient underwent an X-ray or ultrasound examination, scanning, or other medical procedures, it is imperative to inform the attending physician about this.
- Before conducting the study, you need to be more careful about your daily menu. In particular, approximately 5 days before testing for growth hormone,
it is advisable not to eat fried, fatty foods. - It is also highly desirable to avoid all medications that may distort the results of the analysis
. Of course, this is not always possible, but then you need to notify the doctor about it. The exception is when the study is being conducted to test the effectiveness of a treatment. In this case, you need to stop taking the medications prescribed by your doctor on the day of the test. An increase in the concentration of a somatotropic substance in the blood may well be the result of taking drugs such as bromocriptine, glucan, clonidine, estrogen, insulin, adrenocorticotropic hormone, oral contraceptives, and so on. Ideally, any drug that cannot be stopped should be discussed with your doctor. - Three days before the blood test for hormones,
it is strictly forbidden to drink alcohol. It is advisable to give up cigarettes at least on the day of the study (the sooner the better). - 12 hours before the blood
test , you can drink only clean water, since the manipulation must be carried out on an empty stomach. It is also prohibited to consume any other drinks - tea, coffee, mineral water, juice. - Excessive physical activity can also reduce the quality of test results. About three days before donating blood for research, it is better to start abstaining from physical exercise and playing any sports.
If a blood test for growth hormone is repeated, it is advisable to take it in the same laboratory at approximately the same time. Where do hormone tests come from? The answer to this question is from the patient’s vein. The turnaround time for tests depends on the specific laboratory.
Criteria for acromegaly
criteria for acromegaly are currently used worldwide:
:
- increase in growth hormone by more than 1 ng/ml during a glucose test
- increasing IGF-1 levels for a given gender and age.
That is, the minimum level in this sample, any of the points should be more than 1 g/ml.
What hormones are still being studied in patients with acromegaly:
- prolactin,
- thyroid and adrenal hormones,
- sex hormones (estradiol in women and testosterone in men)
Indications for a blood test for growth hormone
The content of the article
Blood test for growth hormone
may be prescribed to the patient in the following situations:
- signs of dwarfism;
- symptoms of accelerated growth rates;
- excessive sweating;
- hair growth disorder;
- osteoporosis;
- muscle weakness;
- reduction in blood glucose levels (for example, after drinking alcohol);
- porphyria.
If a patient comes to an initial consultation with a specialist with ready-made test results, he should definitely check the expiration date of hormonal tests.
ADDITIONAL ANALYSIS AND SERVICES

Treatment of acromegaly
Current treatment goals for acromegaly are:
Of course, we need to normalize hormones.
Of course, we need to control the size of the tumor.
But besides this, we need to eliminate those symptoms of acromegaly that can be eliminated and that are reversible. And, first of all, this concerns cardiovascular changes, this concerns diabetes mellitus, sleep apnea, joint symptoms and colon polyps.
Currently the target values are:
- decrease in the level of growth hormone less than 2.5 ng/ml
- minimum GH level during the glucose test less than 1 ng/ml after adenomectomy
- normalization of IGF-1.
There are three main methods
treatment.
- Surgery
is on the pedestal as the main treatment method for patients with acromegaly. - The second place is occupied by the medicinal method of treatment
. - Third place - radiation treatment methods
, only if the first two are impossible and ineffective.
STH (hormone): norm and deviations
What are the normal values of growth hormone for humans? At different ages, the indicators of such a substance as growth hormone (hormone) are different. The norm for women also differs significantly from the normal values for men:
- Newborns up to one day - 5-53 mcg/l.
- Newborns up to one week - 5-27 mcg/l.
- Children aged from one month to one year - 2-10 mcg/l.
- Middle-aged men - 0-4 mcg/l.
- Middle-aged women - 0-18 mcg/l.
- Men over 60 years of age - 1-9 mcg/l.
- Women over 60 years of age - 1-16 mcg/l.

Surgical treatment of pituitary adenoma with acromegaly.
I will say a few words about surgical treatment.
Currently, endoscopic endonasal operations
And. Operations are performed through the nose. They are most effective for those tumors when the tumor is small in size, the tumor is localized endo-suporsilly and does not grow into the blood sinuses, i.e. it doesn't grow sideways. Because if it grows to the side, it can grow over the carotid arteries, it can grow over the nerves. And in these cases, unfortunately, it is difficult to radically remove, especially if the tumor is dense.
This is a one-time procedure. If everything went well, the tumor was operated on, and the next day the patient already experienced a decrease in hormones. This is the optimal treatment method.
And currently the complication rate is extremely low.
The “success” of surgical treatment depends on:
- SURGEON'S EXPERIENCE (more than 50 operations per year, modern endoscopic installations) Naturally, the success of surgery depends
on the experience of the neurosurgeon. And, indeed, those neurosurgeons who operate on pituitary adenomas, including patients with acromegaly, are generally worth their weight in gold, because they have a lot of experience and not every surgeon, even with modern equipment, can remove such a tumor, because skill is important. I believe with an experienced surgeon, one who performs more than 50 operations per year. Our surgeons perform about 300-500 operations per year. - TUMOR SIZE The larger the tumor, the more difficult it is to remove. But what matters most is the nature of the tumor. That is, the tumor can be invasive, it can grow somewhere, and such a tumor is very difficult to radically remove.
- CHARACTER OF GROWTH (invasion into the cavernous sinus)
If the tumor is small or microadenoma, or a tumor that does not grow beyond the sella turcica. The sella turcica is the bone, so to speak, which is located in the normal pituitary gland. Then the probability of radical removal is extremely high. This is about 80-90% of cases.
If these are large tumors or tumors that are already growing into the cavernous sinuses, then, unfortunately, it is not possible to radically remove such a tumor. Only in 50-60% of cases do we get truly radical removal.
Nevertheless, even in those patients in whom radical removal cannot be performed, removal of most of the tumor leads to an improvement in the patient's condition and improves their sensitivity to therapy. Therefore, it is currently believed that even if we cannot completely remove the tumor, we must reduce it and this will improve the quality of life for our patients.
Here is an example of a successful removal.
The patient is 56 years old. Complaints of headaches, changes in appearance, sweating. The patient has been experiencing acromegaly for 6 years, changes in appearance, enlargement of the hands and feet. For 4 years her blood pressure has been rising. Several years ago, a diffuse goiter was identified. And it was only in 1919 that acromegaly was diagnosed. An increase in IGF-1 to 630 was noted and a glucose test was performed, where we see high levels of hormones, there is no suppression of less than 1 ng/ml. This patient has a small tumor that does not grow anywhere. The patient underwent endonasal adenomectomy. And on the third day after the operation, normalization of growth hormone was noted. And after 3 months, IGF-1 normalization. The patient was discharged on the 3rd day after surgery. Such a patient already needs dynamic observation. But she should no longer receive any additional treatment, because we have achieved remission of acromegaly and radically removed the tumor.
In general, the main method of treating acromegaly is the surgical method, not only in our country, but throughout the world.
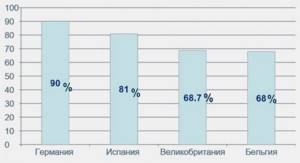
Figure 9. Number of operated patients with acromegaly according to national European registries
Long-Term-Outcome in Patients with Acromegaly: Analysis of 1344 Patients from the German Acromegaly Register. 2012
European countries and the number of patients operated on are presented here. And we see that the main method of treatment, as in Germany, Spain, and other countries, is still the surgical method of treatment.
Treatment
Determination of indications for replacement therapy
The feasibility of replacement therapy for GH deficiency in adults is determined by the expected benefit for each individual patient. Patients with severe GH deficiency, confirmed by stimulation tests and low serum concentrations of IGF-1, are most likely to benefit from treatment. Clinical manifestations indicating the need for treatment are osteopenia, increased cardiovascular risk, as well as reduced quality of life, which must be confirmed by validated questionnaires for this disease [74].
An important category are patients who have achieved target height during replacement therapy and are transferred under the supervision of an adult endocrinologist. In such patients, full maturation of the skeletal and muscular systems may continue for the next 10 years [75–77]. When somatropin was discontinued after achieving target growth, there was a deterioration in lipid metabolism, body composition and quality of life [76, 78, 79]. After achieving final growth, it is necessary to re-diagnose GH deficiency, 1–3 months after a break in treatment with somatropin (Table 4).

Table 4. Re-diagnosis of GH deficiency after reaching final height
The negative clinical manifestations of GH deficiency and the positive effect of somatotropin replacement therapy also extend to patients over 65 years of age [80]. Despite the known fact that GH secretion decreases with age, diagnostic tests make it possible to distinguish between a physiological decrease and a pathological decrease caused by GH deficiency [81]. Thus, the same criteria apply to older patients as to other age categories. However, for such patients it is necessary to choose a lower starting dosage, which will be discussed in more detail below.
Initiation of treatment and selection of dosages
Treatment of GH deficiency in adults is recommended to begin with low doses (0.2−0.4 mg/day subcutaneously), this reduces the likelihood of side effects [82]. Dose titration is recommended at 6–8 week intervals, depending on clinical response and IGF-1 concentrations, which are recommended to be maintained in the upper half of the reference range. In patients under 30 years of age, it is recommended to choose a higher starting dose (0.4–0.5 mg/day), and in elderly (over 60 years of age) a lower dose (0.1–0.2 mg/day) to minimize the risk of developing side effects, since with age there is a physiological decrease in the need for somatotropin. Women receiving oral estrogen replacement therapy require a higher dose of somatropin because oral drugs inhibit the synthesis and secretion of IGF-1 by the liver [83]. When using transdermal forms of estrogens, dose adjustment of somatotropin is usually not required.
After selecting a stable dosage, a blood test for IGF-1 and evaluation for side effects is recommended every 6 months, and a lipid profile and fasting plasma glucose analysis every 12 months or immediately after increasing the dose of somatotropin. A physical examination measuring blood pressure, weight, waist circumference, and BMI is recommended annually and at every visit. If, according to the data of the first X-ray densitometry, a decrease in BMD is detected, a repeat study is carried out once every 2 years. It is also recommended to annually fill out appropriate questionnaires to assess quality of life.
The maximum duration of treatment is currently unknown. However, if there is no effect of treatment within 1 year, it is necessary to decide on the abolition of somatotropin [24].
Side effects
The main side effects of replacement therapy are caused by changes in water-electrolyte metabolism disorders that occur with GH deficiency or fluid retention in case of drug overdose: arthralgia, joint stiffness, myalgia, paresthesia and peripheral edema. Such side effects quickly regress when the dose of somatotropin is reduced. Since previously the initial dose was selected based on body weight, side effects were more common than when the dose was titrated from the minimum.
Very rare side effects include benign intracranial hypertension (BIH) and macular edema. The prevalence of ADHD in the population of children receiving growth hormone therapy is approximately 100 times higher than in the healthy population [84]. In the literature, there is only one description of ADHD as a side effect of replacement therapy for GH deficiency in an adult patient [85]. Two cases of macular edema were described in patients without diabetes mellitus: in an 11-year-old girl who received somatotropin therapy for Shereshevsky–Turner syndrome, and in a 31-year-old adult patient with traumatic injury to the hypothalamic-pituitary region. In both cases, the side effect developed due to an increase in the dose of somatotropin [86].
Impact on replacement therapy for other deficiencies
GH inhibits 11-β-hydroxysteroid dehydrogenase type 1 and promotes greater cortisone synthesis and decreased cortisol synthesis. Careful monitoring of patients with adrenal insufficiency (AI) is necessary when initiating treatment with somatotropin, since the clinical picture of adrenal insufficiency may develop and the risk of decompensation may increase even in mild infectious diseases [87]. In addition, in patients with subclinical hypocortisolism, after initiation of somatropin therapy, the manifestation of clinical manifestations of NN is possible.
When somatropin is prescribed to patients without secondary hypothyroidism, a decrease in the concentration of serum thyroxine (T4) is observed, but the concentration of triiodothyronine (T3) remains stable. Patients on T4 replacement therapy often require increased doses. It has been suggested that GH may increase the peripheral conversion of T4 to T3 and at the same time suppress the release of TSH in the pituitary gland, but the exact mechanism is unknown [88, 89].
Sensitivity to GH is reduced in patients receiving oral estrogen-containing drugs. This phenomenon is explained by the phenomenon of first passage through the liver and inhibition of IGF-1 production. With the use of transdermal forms of estrogens, this effect is practically absent [90, 91].
Testosterone stimulates the secretion of growth hormone and enhances its stimulating effect on the production of IGF-1. Dihydroepiandrosterone (DHEA) potentiates the production of IGF-1 - patients on DHEA therapy achieve IGF-1 targets on lower doses of growth hormone. The mechanism of this effect is unknown. Since DHEA is metabolized to testosterone, it has been suggested that the increase in serum testosterone concentrations accounts for this effect [92].
Cancer risk
According to epidemiological studies, there may be a relationship between high-normal concentrations of GH and IGF-1 in the blood and the prevalence of cancer [93]. In acromegaly, the risk of developing certain cancers is higher than in the general population [94].
Currently, there is no data on an increase in the frequency of relapses of extra- and intracranial tumors in adult patients receiving somatotropin for GH deficiency. However, treatment with somatotropin is contraindicated in the presence of active cancer [24]. In 2021, a study by D. Olsson et al. was published, which included 426 patients with hormonally inactive adenomas: 207 received somatotropin (median treatment duration 12.2 g), 219 did not receive somatotropin treatment (median follow-up 8.2 g .). Among patients receiving replacement therapy, a decrease in overall mortality was noted and no increase in the incidence of mortality from cancer was detected [95].
According to a meta-analysis that analyzed data from seven prospective and two retrospective studies ( n
=11,191). Somatotropin replacement therapy is associated with a reduction in cancer risks in adults with GH deficiency (relative risk 0.69; 95% CI 0.59–0.82). The risk reduction was maintained in additional subgroup analyses, excluding retrospective studies with fewer than 100 observations, studies among patients with craniopharyngiomas, and studies with less than 3 years of follow-up [96].
Thus, according to existing data, the benefits of somatotropin replacement therapy in adults exceed the theoretical risk of neoplasms. Screening for neoplasms in patients receiving growth hormone replacement therapy is no different from the general population. At the same time, it is worth closer monitoring of mature patients, patients with an oncological history and family predisposition, as well as a group with a proven increase in oncological risk - patients after radiation therapy [97].
The quality of life
The quality of life of adult patients with GH deficiency is assessed using the appropriate questionnaires: QoL-AGHDA [98] and PGWB [99].
In 2012, a meta-analysis by A. Hazem et al. was published, which included data from randomized placebo-controlled trials - a total of 54 studies ( n
=3400). Of the selected studies, 16 assessed quality of life, but the authors were unable to conduct a meta-analysis due to data heterogeneity and lack of quantitative data. Eleven studies reported significant improvements in quality of life according to at least one assessment method [100].
Mortality
The study, based on data from the Dutch National Registry for Growth Hormone Treatment, compared 2229 patients receiving growth hormone treatment with a first control group of 109 untreated patients with GH deficiency and a second control group of 356 patients after discontinuation of growth hormone. The standardized mortality rate in the treatment group was 1.27 (1.04–1.56) relative to the general population. After excluding patients with acromegaly and Itsenko-Cushing's disease from the analysis, the indicator was 1.29 (1.05–1.59), after excluding high-risk patients (craniopharyngiomas or other formations of the hypothalamic-pituitary region) - 1.00 (0.79 –1.26). There was also a significant increase in the standardized mortality rate among women in the treatment group - 2.52 (1.57-4.06), and this was observed even after excluding high-risk patients. The authors note that this may be due to the long-term course of uncompensated GH deficiency, which negatively affected cardiovascular risk, but this assumption requires further study [101].
In a study by R. Gaillard et al. among 13,983 patients with GH deficiency receiving somatropin (average follow-up period 4.9 years), an increase in overall mortality was noted by 13% compared with the general population (standardized mortality rate 1.13 (1.04–1.24)), however, mortality rates from cardiovascular diseases and cancer did not differ [102]. According to the results of a meta-analysis by J. Pappachan et al., the standardized mortality rate was 2.40 [95% CI 1.46–3.34] in patients with GH deficiency without treatment and 1.15 [95% CI 1.05–1. 24] in patients receiving somatotropin [103]. K. Stochholm and G. Johansson also demonstrated lower mortality among patients receiving growth hormone compared with patients without treatment: hazard ratio for all-cause mortality 0.34 (95% CI 0.15–0.77) [104].
Metabolic effects of replacement therapy
Since GH is one of the significant regulators of metabolism and energy homeostasis [105], treatment of GH deficiency in adult patients affects body composition, lipid, carbohydrate and bone-mineral metabolism, which is confirmed by meta-analysis data.
Body composition.
In a meta-analysis by A. Hazem et al.
54 RCTs were included ( n
~3400). Somatropin treatment significantly reduced body weight (–2.31 kg, 95% CI –2.66– –1.96) and fat mass (–2.56 kg, 95% CI –2.97– –1.3) and increases lean body mass (1.38 kg, 95% CI 1.10–1.65). However, no significant effect on bone mineral density (BMD) was detected, which may be due to the small number of observations [100].
The meta-analysis by C. Newman et al., which aimed to compare the effectiveness of low and higher doses of somatropin on body composition and lipid metabolism, included the results of 22 RCTs ( n
=1153). Lean body mass significantly increased in treatment groups compared with placebo, while fat mass decreased. Changes in lean body mass and fat mass showed a dose-dependent effect, with treatment at higher doses being more effective [106].
Cardiovascular system and lipid metabolism.
According to a meta-analysis by P. Maison and P. Chanson, which included 16 studies, compensation of GH deficiency promotes an increase in the mass of the left ventricle, the thickness of the interventricular septum and the posterior wall of the left ventricle, an increase in the diameter of the left ventricle in diastole and stroke volume [107]. It is known that the thickness of the intima-media complex of the carotid arteries is a predictor of progression of coronary heart disease [108]. It has been shown that treatment of GH deficiency leads to a decrease in this indicator [109]. Studies have demonstrated a decrease in total serum cholesterol, almost entirely due to a decrease in the concentration of LDL cholesterol. The effect is more pronounced
Postoperative monitoring of pituitary adenoma.
I will say a few words about postoperative monitoring.
- Typically, patients are tested for growth hormone on the first day after surgery until discharge. And a decrease in its level to less than 2 ng/ml is a good predictor of radical removal and long-term remission.
- A glucose test can be performed directly in the clinic, most often 7-10 days after surgery. But this is not done everywhere. For example, this study is not carried out here because patients are discharged quite quickly.
- Next we look at IGF-1. It is recommended to watch it according to all deadlines after three months, because unlike growth hormone, it lives for a long time and it returns to normal slowly, not immediately after the operation. If we see that it decreases, but remains elevated, even within 3 months, we can observe this patient and look at the IFR after another 3 months. In some patients, we see a decrease and normalization after six months. But if after six months it has not returned to normal, then this clearly indicates that acromegaly persists. Or, if we see that after three months it remains very high or increases, then we do not wait these six months, but prescribe treatment.
- It is recommended to do a follow-up MRI no earlier than three months later. Optimally, this is after 6 months. Because there are various postoperative changes, swelling, in addition, surgeons use hemostatic sponges, various materials that gradually dissolve. If you do an MRI earlier, it will simply be difficult to interpret what it is: some postoperative changes or a remnant of the tumor.
Acromegaly should be treated by a multidisciplinary team
: doctors who understand treatment and treat these patients are not only an endocrinologist, a neurosurgeon, but also a whole group of doctors who decide on the patient’s treatment tactics.
Useful tips
- Deep sleep. The most intense production of growth hormone occurs during deep sleep, which is why you need to sleep at least seven to eight hours.
- Rational diet. The last meal should be at least three hours before bedtime. If the stomach is full, the pituitary gland will not be able to actively synthesize growth hormone. It is recommended to have dinner with easily digestible foods. For example, you can choose low-fat cottage cheese, lean meat, egg whites, and so on.
- Healthy menu. The basis of nutrition should be fruits, vegetables, dairy and protein products.
- Blood. It is very important to monitor the level of glucose in the blood; its increase can cause a decrease in the production of somatotropic hormone.
- Physical activity. For children, volleyball, football, tennis, and sprinting sections would be an excellent option. However, you should know: the duration of any strength training should not exceed 45-50 minutes.
- Fasting, emotional stress, stress, smoking. Such factors also reduce the production of growth hormone in the body.
In addition, conditions such as diabetes mellitus, pituitary gland injuries, and increased blood cholesterol levels significantly reduce the synthesis of growth hormone in the body.

Radiation treatment method
The next treatment method is radiation treatment. Using our center as an example, we have a department of radiotherapy and radiosurgery, where patients with various brain tumors, including pituitary adenomas, are treated. We present various installations for both radiation therapy and radiosurgery, and cyber-knife, and gamma-knife, and Novalize, Primus. But still, this method is used in case of non-radical removal and ineffectiveness, intolerance and, as happens in our realities, inaccessibility of drug therapy.
Currently, one of the most modern methods is
radiosurgical treatment
. This method is effective in treating patients, but mainly in patients with non-radical removal, or in those patients whose acromegaly remains active.
Currently, more and more publications are appearing on the effectiveness of this treatment method. It provides good control of tumor growth. That is, after radiation treatment, the tumor does not grow in about 93-100% of cases or decreases. The duration of achieving remission ranges from 1 to 10 years, with an average of 3.5 years. That is, after radiation treatment, the effect is not realized immediately, but we wait at least a year. And only after a year can an initial decrease in hormone levels occur.
But, unfortunately, one of the common complications is
hypopituitarism
, i.e. decreased pituitary function. According to modern studies, this is about 24% on average, but some authors indicate up to 66% of cases. Nevertheless, this percentage still makes us happy, because it is lower than with previously used fractionated radiation therapy, when such complications occurred in about 80% of cases.
Radiation treatment has a delayed effect
.
This treatment is carried out, in general, over several sessions, it is painless for patients, most often it is carried out on an outpatient basis, the patients are discharged. But acromegaly activity remains. Therefore, such patients should receive somatostatin analogues
. And it is recommended to trially discontinue the drugs once a year; if the IGF returns to normal, then we can discontinue the somatostatin analogues. If IGF rises again, then we return to taking somatostatin analogues.
I would like to draw your attention to the fact that, given the risk of developing hypopituitarism, all patients who have undergone radiation treatment must have their pituitary gland function assessed once a year.
. From one year to 10-15 years. If there are already dysfunctions of the thyroid gland or adrenal glands or gonads, then hormone replacement therapy is necessary.
Somatotropic hormone deficiency in the body
Particular attention is paid to somatotropin in childhood. GH deficiency in children is a serious disorder that can cause not only stunting, but also delayed puberty and general physical development, and in certain cases, dwarfism. Various factors can cause such a disorder: pathological pregnancy, heredity, hormonal disorders.
An insufficient level of somatotropin in the body of an adult affects the general state of metabolism. A low level of growth hormone accompanies various endocrine diseases, and a deficiency of somatotropic hormone can provoke treatment with certain medications, including the use of chemotherapy.
And now a few words about what happens if there is an excess of somatotropic hormone in the body.
Drug therapy in the treatment of acromegaly
It is very pleasing that all the modern types of drugs that are used in the world to treat acromegaly are presented in Russia.
These are three groups:
- Analogs (receptor ligands) of somatostatin.
- Type 2 dopamine receptor agonists.
These two groups act directly on tumor cells.
- Growth hormone receptor antagonists. This drug acts peripherally, it does not act on the tumor, but normalizes IGF-1, which is the hormone that causes the clinical picture of acromegaly. Therefore, in these cases, we achieve normalization of IGF-1 and regression of acromegaly symptoms.
According to all modern consensuses, the main drugs for the treatment of acromegaly are
somatostatin analogues
. They are the first line of therapy. They actually subjectively improve the condition of patients. patients note a decrease in headaches, a decrease in weakness, sweating, and a decrease in joint pain. Normalization of hormones is observed in 55% of patients. Tumor size also decreased in approximately half of the patients.
Interfering factors
Increases: Alpha-adrenergic stimulants (Norepinephrine, Clonidine), Beta-adrenergic blockers (Propranolol), Dopaminergic stimulants (Levodopa, Bromocriptine, Apomorphine), Serotonergic stimulants (L-tryptophan), ACTH, Vasopressin, Estrogens, Dopamine, Serotonin, Alphadopa, Insulin, Vitamin PP, Amphetamine, amino acids (Arginine), Diazepam, Indomethacin, Interferon. Reduces: Progesterone, Glucocorticoids, Glucose, Alpha-adrenergic stimulants, Alpha-adrenergic blockers (Phentolamine), Beta-adrenergic agonists (isoproterenol, Dopamine), Serotonin receptor antagonists (Methysegride, Cyproheptadine), Dopamine blockers, Bromocriptine (for Acromegaly), Phenothiazine derivatives , Somatostatin.
Clinical guidelines for the treatment of concomitant diseases
I would like to say a few words about clinical recommendations for the treatment of concomitant diseases.
According to Russian clinical guidelines, we must treat all concomitant, or also called comorbid, conditions.
If the patient has biochemical remission, then we see significant improvements, reduction in swelling, and joint pain. But, unfortunately, those changes in the growth of joint bones have practically no retroactive effect; joint pain can persist, even when biochemical remission is achieved
. Such patients require additional prescriptions: either physical therapy, or anti-inflammatory therapy, analgesics. If there are pronounced lesions in large joints, endoprosthetics of these joints is performed.
All patients who have osteoporosis
, it is necessary to perform X-ray endostometry once every 2 years.
If the patient has decreased pituitary function
, dysfunction of the thyroid gland, adrenal glands, gonads, then, accordingly, replacement therapy should be carried out.
As a rule, if we have achieved remission of acromegaly, then patients experience positive dynamics or complete disappearance of sleep apnea syndrome
, sleep apnea. But if it persists, then Sibab therapy is necessary. Naturally, if a patient smokes, he definitely needs to give up this bad habit.
If patients continue to have carpal tunnel symptoms
, i.e. If this is pain and numbness in the fingers, then such a patient needs physical therapy, in some cases endoscopic operations are performed to cure this syndrome. Where the carpal ligament is cut.
One of the main factors is the normalization, of course, of all risk factors for the development of the cardiovascular system
. It is necessary to normalize blood pressure. Treat diabetes mellitus naturally. The target blood pressure levels are less than 130 over 80, and glycated hemoglobin less than 6.5%, i.e. just like a healthy person.
For the purpose of possible prevention of the development of intestinal cancer
, all patients are recommended to undergo a colonoscopy upon diagnosis of acromegaly.
If there are intestinal polyps
, then removal of these polyps is necessary.
One of the clinical examples.
Male 43 years old. The patient had typical manifestations of acromegaly. The patient was observed by cardiologists for 5 years for hypertension; his blood pressure increased to 150 over 90. For 2 years he had diabetes mellitus and diffuse goiter.
The examination revealed an increase in IGF-1 to 630. And acromegaly was diagnosed. MRI revealed an endolateral pituitary adenoma.
The patient underwent endoscopic endonasal adenomectomy. We see that growth hormone decreased on the second day after surgery. But there remained 5 ng/ml. And after 3 months, the patient showed a decrease, but also maintained a high level of IGF-1. We performed an MRI, which revealed the remainder of the tumor in the cavernous sinus. After the operation, the patient had symptoms of diabetes insipidus: thirst, urine output, up to 5 liters per day. He received the drug desopresin, but later these symptoms regressed. He said it was because of the drug. Given the continued activity of acromegaly, somatostatin analogues were prescribed, and against this background, the patient showed a decrease in IGF-1. But it remained elevated.
A decision was made to perform radiosurgical treatment, since the remainder of the tumor was only in the cavernous sinus, and the pituitary gland did not fall into the irradiation zone. After radiation treatment, despite the lack of normalization and remission of acromegaly, he continued to receive somatostatin analogues. Because he felt much better against this background. And after 2 years, against the background of the discontinuation of somatostatin analogues, normalization of IGF-1 and a decrease in growth hormone during the course of 1 ng/ml were noted. We continue to monitor this patient. Currently he does not have any endocrine disorders in terms of decreased pituitary gland function. But, of course, we continue to observe every year.
If STH is low
There is also a downside when tests reveal a lack of growth hormone in the body. As a result, slow growth is observed, and the general and sexual development of the child may be disrupted. If this is not detected in childhood, then in adulthood a person can have a height of no more than 140 cm. Children experience disturbances in the functioning of the thyroid gland and hormonal imbalances. Adults also experience metabolic disorders, obesity, and memory problems. In addition, somastatin levels increase.
Most often, GH deficiency occurs as a result of diseases of the endocrine system.