PET/CT diagnostics have been used in clinical practice for several decades, and during this period no negative effects on healthy tissues and organs of patients have been identified.
Radionuclide studies, including PET/CT, are carried out in accordance with radiation safety standards. For non-cancer patients, the established standard radiation dose is on average 1 mSv per year, but not more than 5 mSv per year. However, the side effects of PET/CT are not commensurate with the danger of diseases that this diagnostic method can detect. Therefore, no maximum standards have been established for cancer patients, but when prescribing a study, three factors are taken into account:
- validity - the benefit of diagnosis must exceed the possible harm from radiation;
- optimization – all necessary measures must be taken to reduce radiation exposure;
- standardization – compliance with established safety standards and rules.
Exposure over 200 mSv per year is considered potentially dangerous.
Radiation safety standards and requirements for the appointment of radionuclide diagnostics are strictly observed. Examinations are carried out only if there is sufficient justification and if there is evidence.
Radiation from PET/CT: harmful or not
The radiation dose from PET/CT depends on the type of radiopharmaceutical and the scope of the study, for example, when scanning a specific area, the radiation dose is less than when scanning the whole body. With additional contrast, the performance will be slightly higher.
Modern standards reduce harm from PET/CT:
- PET/CT is performed using ultra-short-lived radiopharmaceuticals, so the harm from PET/CT is minimal. Thus, the half-life of 18F-fluorodeoxyglucose is 110 minutes. This means that after 20 hours the drug is completely destroyed and excreted by the urinary system.
- The dose of the drug is calculated individually for each patient according to international standards, taking into account body weight, height and age. This allows you to get an accurate result with minimal radiation.
- Modern PET/CT scanners are equipped with ASIR software and filters to reduce the X-ray dose. The ASiR high-definition image reconstruction method is needed for image processing, removal of noise and defects. As a result, you can get a high-quality image after the examination without additional radiation to the patient.
- Proper patient preparation - drinking plenty of water before and during the examination improves visualization of organs and speeds up the elimination of drugs by the kidneys.
- The examination is carried out in compliance with radiation safety standards according to NRB-99/2009 and OSPORB 99/2010.
Preparation for the production of radiopharmaceuticals at the Nuclear Medicine Center in Ufa
Do they do MRI of the lungs and bronchi?
Diagnosis of respiratory pathologies includes a survey, examination, clinical tests, and hardware tests.
Indications for MRI of the lungs are:
- enlarged lymph nodes in the chest cavity;
- clarification of the stage and nature of the tuberculosis process;
- inflammatory diseases of the bronchi and lungs with insufficient information content of other types of diagnostics;
- suspicion of an oncological process in the chest area;
- voluminous neoplasms of unknown origin;
- chest cavity injuries;
- congenital pathologies of the structure of the lungs and bronchi.
Magnetic resonance imaging is used in planning surgical treatment of pathologies of the respiratory system. The method allows you to determine the size and location of the lesion and clarify the nature of the upcoming operation.
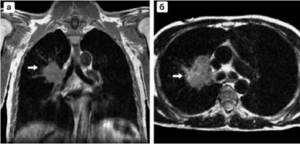
Oncological process on MRI: a - frontal projection, b - axial section (arrow indicates a tumor in the middle part of the lung)
During the rehabilitation period, at least 2-3 procedures are indicated during the first year. Control scans will help monitor the process of restoration of damaged tissues, promptly diagnose complications and adjust postoperative therapy.
MRI of the lungs and bronchi can be done if a person is intolerant to X-ray radiation. The electromagnetic field does not affect the condition of patients suffering from radiation sickness.
Informativeness and safety of positron emission tomography
PET/CT is the optimal examination method, as it combines positron emission tomography, which helps to see changes at the cellular level, and computed tomography to assess the structure of the organ. As a result of the diagnosis, the doctor receives more complete information about the pathological process; tumors from 6 mm in greatest dimension are visible in the images.
Positron emission tomography allows you to determine the stage of the disease and plan treatment, reduce the radiation dose to surrounding healthy tissue during radiotherapy by accurately determining the location of the tumor. It is indispensable in assessing the prevalence of certain malignant neoplasms, such as lymphoma, melanoma and others.
Diseases of the lungs and bronchi
Pathological changes in the airways lead to disruptions in the functioning of the respiratory system. The lungs and bronchi perform the following functions in the human body:
- saturate the blood with oxygen and remove carbon dioxide;
- provide thermoregulation;
- protect against pathogens;
- participate in metabolic processes;
- serve as shock-absorbing protection for the heart.
Pathological changes can affect the bronchi, lung parenchyma and pleural cavity. Clinical symptoms depend on the location and severity of the disease. The most characteristic signs of pathologies of the respiratory system are:
- cough (dry or wet, depending on the presence of sputum);
- shortness of breath (in severe cases, asphyxia is possible);
- presence of blood in sputum;
- pain in the chest cavity (more often observed when inhaling/exhaling).
Features of the manifestation of these symptoms suggest the nature of the disease. Instrumental examination (X-ray, CT, MRI of the lungs and bronchi) allows you to clarify the diagnosis and location of the pathological focus.
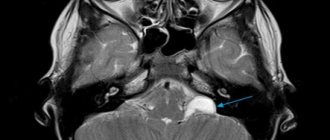
MRI image of the lungs, frontal projection
Diseases of the respiratory system are classified depending on the etiology, location and nature of negative changes. There are the following types of damage to the organs of the thoracic cavity:
- inflammatory processes - acute and chronic bronchitis, pneumonia;
- infectious diseases - tuberculosis;
- granulomatous processes – sarcoidosis;
- malignant tumors – adenocarcinoma, squamous cell carcinoma, etc.;
- parasitic lung infections - ascariasis, pneumocystis, etc.;
- benign neoplasms – papillomas, adenomas;
- congenital pathologies - aplasia of pulmonary tissue, bronchial stenosis, accessory lobe, sequestration, etc.;
- necrotizing processes - abscess and gangrene of the lung, purulent pleurisy;
- allergic diseases - bronchial asthma;
- vascular diseases – pulmonary hypertension, embolism;
- damage to the pleural cavity - pneumo- and hemothorax, pleurisy.
The causes of respiratory diseases are most often chest injuries, infectious, fungal, viral lesions, and the development of neoplasms. The diagnosis largely depends on what the MRI of the lungs and bronchi shows. The final decision is made by the attending physician based on all examination results.
Use in radiotherapy
Radiation therapy involves targeted irradiation of the tumor. The doctor’s goal is to effectively influence the malignant lesion, affecting healthy tissue as little as possible. To do this, you need to accurately determine its boundaries, which is not always easy.
PET/CT helps to distinguish a malignant formation from tissues unaffected by the process and target it.
For example, with lung cancer, atelectasis is observed - collapse of the lung tissue due to the fact that air does not enter the alveoli. The tumor may be small and occupy only part of the atelectasis. But on a computed tomography scan the boundaries between the tumor tissue and the collapsed lung are not visible, so healthy cells are exposed to irradiation. PET/CT helps to distinguish a malignant formation from tissues unaffected by the process and target it. Similarly, positron emission tomography allows one to determine the boundaries of glioblastoma against the background of cerebral edema.
Thanks to PET/CT, the doctor sees the exact contours of the lesion, as a result, the required dose of radiation is delivered to a smaller area, which helps preserve healthy tissue, which is vital when organs such as the brain and lungs are damaged.
Doctors reported what frequent CT scans lead to
Rospotrebnadzor reported that an increase in the number of studies using computed tomography (CT) amid the COVID-19 pandemic could trigger an outbreak of diseases caused by radiation.
According to the department, since the beginning of March, the collective radiation dose from CT scans has exceeded the norm by one and a half times, since tomography, in addition to PCR tests and antibody tests, has become one of the main methods for diagnosing coronavirus.
“People are in a panic because of COVID-19 and are ready to do CT scans every day; I am not always guided by doctors’ testimony,”
— pulmonologist Marina Kazakova told Gazeta.Ru.
At the same time, specialists at the UC Davis Health System Medical Center at the University of California said that CT scans are done unreasonably often. At the same time, a medical examination is accompanied by an excessively high dose of radiation - it is 2-5 times higher than with a conventional x-ray examination.
As Kazakova told Gazeta.Ru, such a dose can lead to cancer - it is especially dangerous for pregnant women. The doctor emphasized that, as a rule, the disastrous consequences of a CT scan are visible only after many years. “At the same time, a really large single dose of radiation can lead to radiation damage to organs, tissues or organ systems,” she added.
Reducing the dose and number of procedures would reduce the risk of developing malignant tumors by 62%. Californian researchers came to these conclusions as a result of an analysis of medical statistics and calculations published in the journal JAMA Pediatrics.
In addition, an increased dose of radiation leads to disruption of the process of cell division in the body. This, in turn, significantly slows down a large number of protective mechanisms designed to protect the human body, an employee of the Moscow Department of Health, radiologist Viktor Gombolevsky told FAN.
At the same time, oncologist Alevtina Kiseleva did not agree with her colleague. “Yes, ionizing radiation in large doses is dangerous for humans. However, there are established parameters that determine the maximum permissible safe doses for the human body when examining certain organs,” the expert explained to Gazeta.Ru.
Thus, according to her, the norm for radiation exposure in Russia during preventive studies using X-rays is considered to be a dose of up to 1 millisievert (mSv) per year. At the same time, Gombolevsky believes that on average Muscovites receive about 3 mSv annually from the environment alone.
Meanwhile, immunologist Maria Polner told Gazeta.Ru that the sanitary and epidemiological rules (SanPiN) do not establish maximum radiation doses for patients.
“Therefore, in this matter we can only speculate. But in theory, frequent unfounded research could do more harm than good."
- she clarified.
At the same time, Alevtina Kiseleva is convinced that CT scanning should not be neglected. “The results of computed tomography allow doctors to make the most accurate, correct diagnosis and prescribe treatment in a timely manner. And this is exactly what we need to diagnose lung damage from a new coronavirus infection,” said the oncologist.
CT helps to identify malignant tumors in a timely manner, immunologist Polner reminded Gazeta.Ru. “I think that timely detection of cancer is more important than the likely consequences that tomography can lead to,” said the doctor.
In addition, according to Kiseleva, modern devices make tomographic examinations as safe as possible. “Thanks to digital X-ray technology, the proportion of radiation exposure is significantly less than 20 years ago. Each patient’s exposure to radiation is documented so that doctors and patients can control the dose of radiation received during X-ray studies,” the Gazeta.Ru interlocutor emphasized.
She added that cancer patients undergo CT examinations more often than others, since doctors need to monitor the dynamics of the underlying disease and detect progression or recurrence of the tumor in a timely manner. At the same time, the patients' condition does not worsen.
“In general, the information obtained during research makes it possible to identify and radically cure many dangerous diseases at the earliest stages, which significantly reduces their mortality,” concluded Kiseleva.
Side effects of positron emission tomography
The state of health after PET/CT is not disturbed or disturbed, however, with some diseases it is difficult for the patient to remain motionless for a long time. The most common side effects of the diagnosis are weakness and dizziness due to dietary restrictions and the duration of the study. The administered medications are non-toxic, prepared under sterile conditions and meet the requirements of state standards. If you follow your doctor's recommendations, PET/CT has no negative consequences.
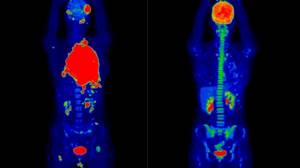
A 19-year-old female patient was diagnosed with diffuse large B-cell lymphoma. The image on the left is the results of a PET/CT study to assess the extent of the malignant process (red areas) before treatment, on the right are the results after two courses of chemotherapy.
Is there any harm from having a CT scan with contrast?

To perform a bolus-enhanced CT scan, a special radiopaque contrast agent is used, which is injected intravenously using a special pump. The contrast contains iodine-based drugs. It is this substance that can cause an allergic reaction in patients, therefore, if the patient is allergic to iodine or seafood, and also has a history of liver or gallbladder disease, serious cardiovascular pathologies or renal failure before the study, you need to inform the radiologist about this or refuse diagnosis with contrast.
In some cases, when the study is vital for the patient, but he has an increased sensitivity to iodine, an antihistamine is administered before the CT scan with contrast to eliminate the risk of developing an allergic reaction.
Even practically healthy people may also experience side effects during the procedure - nausea, slight vomiting, allergic skin reaction, loss of taste and smell. These disorders occur in only 1-5% of patients and usually go away on their own. Cases of more serious violations in the health status of patients are rare.
Contraindications and recommendations
There are several cases in which magnetic resonance scanning is strictly contraindicated. These include the presence in the patient’s body:
- artificial pacemaker;
- metal fragments;
- hearing aid or implants in the cochlea;
- metal implants;
- fixed metal dental bridges and/or crowns;
- surgical clips, for example, in the area of an aneurysm;
- surgical braces;
- lateral column stimulators;
- vena cava filters.
In such cases, other diagnostic methods are used: ultrasound diagnostics, X-ray fluorography, endoscopy, computed tomography. We are talking about certain diseases that can be identified by the above methods in combination: infectious, obliterative, dust bronchitis, tuberculosis and bronchial hyperreactivity, pneumonia and bronchial pathology.
Breastfeeding and the presence of an intrauterine device are not contraindications to MRI. In case of pregnancy, the examination requires the authorization of a gynecologist. Although no obvious adverse effects from MRI on the fetus have been identified, doubts about the influence of strong electromagnetic radiation in the early period of pregnancy have given rise to a generally accepted rule: the conditional limitation is pregnancy in the first trimester, up to the 12th week of gestation.
MRI examination cannot be carried out in patients with severe impairment of vital functions requiring constant hardware and other correction, as well as in people with fear of confined spaces and in patients with inappropriate behavior.
How often should I have a CT scan?
If these complaints develop, you should immediately seek medical help. During the examination, doctors will objectively assess the patient’s condition, including monitoring saturation (oxygen saturation in the blood). Nowadays, many people have a pulse oximeter at home and measure the indicators themselves, but in some cases the patient cannot adequately independently assess the indicators of the sensor.
“I would also like to remind you that the radiation exposure during CT scanning is 150 times higher than radiography. Don’t give in to panic without a doctor’s prescription and rush to do one, much less 4 CT scans. The above signs are “beacons” both for prescribing a primary CT scan and in dynamics. If your condition is stabilized and you are feeling well, you should also not rush to the study yourself,” says Evgenia Parshina.
In addition, performing CT scans without an indication creates additional stress on the healthcare system, when there may not be enough time and appointments for those who really need it. “The presence of lung damage without clinical manifestations, as well as without assessing concomitant diseases, does not mean anything at all, even if the lung damage is more than 45%,” says the immunologist.
Article on the topic
Vaccination, hardening and vitamins. The doctor talks about how to protect yourself from pneumonia
Treatment of pneumonia
To treat pneumonia, you need to know the name of the infection. In patients, the name of the pathogen is unknown at the very beginning of the disease, so empirical antibiotic therapy is used - treatment aimed at the likely pathogen. For all patients with CAP, treatment regimens have been developed aimed at destroying S.pneumoniae and atypical pathogens.
For most patients, combination therapy with beta-lactam antibiotics or macrolides is used. Alternative regimens include fluoroquinolone monotherapy.
Treatment of SARS CoV-2
- The principles of treating pneumonia are general. Prescription of antiviral and antibacterial therapy.
- In severe cases, in a hospital setting, high-flow oxygen therapy, monoclonal antibodies, anticoagulants, and pulmonary ventilation are prescribed.
- Antibiotics do not work against the COVID 19 virus.
Symptoms and signs of pneumonia

Complaints with pneumonia are sudden. Fever, chills, fatigue, chest pain combined with cough (with or without phlegm), shortness of breath, difficulty breathing, increased breathing occur and increase over several hours.
Blood tests will help diagnose the disease: leukocytosis or leukopenia is the result of the body's inflammatory response. Inflammatory markers such as ESR, C-reactive protein and procalcitonin may increase, although the latter is largely specific to bacterial infections.
A mandatory test for diagnosing pneumonia is chest x-ray.
How is an MRI of the lungs performed?
The patient lies face up on the mobile tomograph table. The body and limbs are fixed using bolsters and holding devices. This measure will help avoid involuntary movements during scanning. Changing body position during the examination leads to the appearance of defects in the resulting images.
To protect against the noise of a working device, use special headphones. During the procedure, medical personnel are located in a separate room, which avoids the impact of extraneous electromagnetic pulses on the field induced by the device. Communication with the subject is maintained using an intercom.

MRI session on a closed type machine
The table with the patient is placed in a wide tunnel of the tomograph, inside of which a generator is installed. Sensors read the response of tissues to the induction of a magnetic field, the information is sent to a computer monitor in the form of layer-by-layer images. The thickness of the sections (from 1 mm) is adjusted individually. To get a clear picture, the doctor may ask the patient to hold his breath during the examination.
When using contrast MRI of the lungs and bronchi, the procedure is suspended after obtaining a series of native images. For intravenous administration of the “coloring” solution, a catheter connected to an automatic injector is used. When the contrast fills the vascular bed and intercellular space of the area of interest, scanning is resumed.
As a result of MRI, layer-by-layer images of the respiratory organs are displayed on the computer monitor in three mutually perpendicular projections (sagittal, frontal, axial). If necessary, the doctor reconstructs a 3D image of the area being studied.