- home
- Gynecology
- Female infertility (adhesions, scleropolycystic disease, etc.)
- Laparoscopic tubal surgery
Laparoscopic operations on the fallopian tubes for chronic salpingitis, infertility, ectopic pregnancy, for sterilization.
The first operation performed endoscopically was sterilization. Coagulation of the fallopian tubes with monopolar current was first reported by Palmer R. in 1962, and then by Steptoe PC in 1967. In 1973, Rioux JE and Cloutier D. created a bipolar coagulator to perform coagulation of the fallopian tubes. In the 70-80s, mechanical methods of laparoscopic sterilization using clips and rings, as well as various methods of transcervical occlusion of the fallopian tubes, were proposed. In 1973, Shapiro HI, Adler DLN for the first time removed the fallopian tube using laparoscopic access. A huge contribution to the development of minimally invasive surgery was made by K. Semm, who in 1975 published the first practical guide to operative laparoscopy, which presented the operations of separation of adhesions, terminal salpingostomy, removal of appendages, ovarian resection, etc. In 1977, Bruhat MA, Manhes H et al. reported on conservative interventions for ectopic pregnancy performed endoscopically. In 1981–1982 DeCherney AH described laparoscopic salpingostomy, and since then endoscopic treatment of tubal pregnancy has been widely developed.
Surgeries on the fallopian tubes can be radical and reconstructive plastic. In radical operations, the tube is completely or partially removed due to an ectopic pregnancy or a purulent-inflammatory process. According to V.I. Kulakova, L.V. Adamyan, they make up approximately 14%. Reconstructive interventions (about 86%) are aimed at restoring the patency of the fallopian tubes and are closely related to the study of the problem of infertility.
Laparoscopy for fallopian tube pathology
The fallopian tube (fallopian tube) is a paired tubular organ that essentially connects the uterine cavity with the abdominal cavity.
The main function of the fallopian tube is the delivery of a fertilized egg (zygote) to the site of implantation in the endometrium, which is carried out due to the peristalsis of the fallopian tubes and their lining villi towards the uterine cavity. If there are anatomical changes in the fallopian tubes, the entry of the fertilized egg into the uterus is difficult or impossible. Partial obstruction of the fallopian tube, the presence of obstacles in the form of adhesions lead to the “attachment” of the zygote in it and the development of an ectopic pregnancy, which can be accompanied by life-threatening internal bleeding. According to statistics, from 40 to 80% of female infertility is associated with complete obstruction of the fallopian tubes - the so-called tubo-peritoneal infertility. Therefore, one of the important points in examining a woman who has not been pregnant for more than a year is to conduct a diagnostic laparoscopy to assess the patency of the fallopian tubes. This method also makes it possible to cut adhesions and perform tubal plastic surgery, which leads to restoration of their function. In addition, during laparoscopy, other causes of infertility and gynecological diseases are excluded and, if necessary, eliminated.
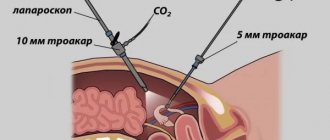
Laparoscopy is a technique that allows for the diagnosis and treatment of diseases of the abdominal cavity and small pelvis with minimally invasive access through 3-4 incisions on the anterior abdominal wall 5-10 mm long, allowing the installation of special ports in the abdominal cavity. Through them, a laparoscope and instruments are inserted, making it possible to carry out not only a detailed examination of the abdominal and pelvic organs, but also a variety of surgical interventions.
A laparoscope is an optical system consisting of a wide-angle lens, an eyepiece and image transfer sections, which allow not only to transmit an image to the screen, but also to study small objects in detail due to the ability to enlarge the “picture”.
Laparoscopy is divided into two main types - diagnostic and therapeutic. It should be noted that quite often a diagnostic operation is transformed into a therapeutic one if pathological changes were discovered during the examination (for example, benign neoplasms or foci of endometriosis).
The tissue removed during this type of surgery is removed through the same small holes. Since very small incisions are made during laparoscopy, in the postoperative period the pain syndrome is much less pronounced than during an intervention accompanied by a large incision on the anterior abdominal wall.
Patients get up and walk within a few hours after the intervention, and the need for painkillers is reduced. In addition, after laparoscopy, the likelihood of adhesions is lower than after transection.
Indications for the diagnosis and treatment of fallopian tube diseases laparoscopically:
1. Infertility - laparoscopy in combination with chromalpingoscopy - injection of Indigo carmine solution into the uterine cavity and assessment of its entry into the abdominal cavity, allows you to diagnose tubo-peritoneal infertility, detect an obstacle and eliminate it. This method, along with the study of a man’s spermogram, the woman’s hormonal status, and assessment of the presence of ovulation, is one of the main methods for examining an infertile couple. It should be noted that a number of patients are inclined to non-operative methods of studying the patency of the fallopian tubes, such as hysterosalpingography and echosalpingoscopy. However, these methods, in some cases, show false results, so obstruction of the fallopian tubes according to the data is an indication for laparoscopy.
2. An adhesive process after an inflammatory disease of the pelvic organs (adnexitis, salpingoophoritis, peritonitis, etc.), leading to the formation of hydrosalpinx, in which the fallopian tube is closed by adhesions at the ends and fluid accumulates in it.
3. Acute inflammatory process leading to the formation of pyosalpinx (accumulation of pus in the fallopian tube) or tubo-ovarian abscess (purulent melting of ovarian and fallopian tube tissue).
4. Ectopic (tubal) pregnancy - in which the fertilized egg implants in the fallopian tube, growing into its wall, often leading to its rupture and life-threatening internal bleeding.
5. Sterilization - by “ligating” the fallopian tubes. This procedure is performed at the request of a woman over 35 years of age, if she has two or more children, upon the written request of the patient.
How to choose the best method?
Many patients are lost in the abundance of diagnostic methods and often do not know what is best to choose for a given study. It is important to understand that you should always consult your doctor. For some, hysterosalpingoscopy is better suited, while others need to additionally remove the cyst from the ovary. In this case, laparoscopy becomes the method of choice. It turns out that the selection of a diagnostic method in most cases is quite individual.
The main criteria that doctors use to evaluate a particular procedure remain:
- Potential reliability of diagnostic information. In this case, laparoscopy often “wins”, since the doctor will be able to see with his own eyes what is happening inside.
- Safety for the patient.
- The need to use additional medications (anesthesia).
- Duration of the procedure.
- The severity of the patient's condition.
By assessing all these criteria, the most appropriate diagnostic method can be selected.
Contraindications to laparoscopy
Despite a number of advantages and possibilities of laparoscopy, there are absolute and relative contraindications to its implementation. These include:
- state of shock;
- severe infectious diseases;
- bleeding disorders;
- severe diseases of the cardiovascular, respiratory systems, liver, kidneys and other organs in the stage of decompensation;
- large hernia of the anterior abdominal wall;
- infection of the anterior abdominal wall;
- tense ascites;
- pregnancy (second trimester);
- diaphragmatic hernia;
- obesity 3-4 degrees.
Types of laparoscopic operations for tubal pathology.
- diagnostic laparoscopy with chromosalpingoscopy – allows you to assess the patency of the fallopian tubes, identify and remove obstacles;
- salpingoneostomy, fimbryoplasty, fimbryolysis - various types of restoration of patency of the fallopian tube;
- adhesiolysis – separation of adhesions that prevent pregnancy;
- salpingotomy (tubotomy) - dissection of the fallopian tube in order to remove the fertilized egg from it in case of short-term ectopic pregnancy;
- salpingectomy (tubectomy) - removal of the fallopian tube, performed in the presence of hydrosalpinx (an enlarged fallopian tube filled with liquid, the ends of which are sealed on both sides), ectopic pregnancy or pyosalpinx (an enlarged fallopian tube filled with pus);
- resection of part of the fallopian tube - performed for some types of ectopic pregnancy, as well as during sterilization.
Menstruation and fallopian tube obstruction
After a check, many patients ask their doctor a question: why is the cycle not disrupted when the fallopian tubes are completely or partially blocked? The timely arrival of menstruation and a stable cycle are a positive aspect of the disease. The fact is that the ovaries can work normally even if the fallopian tubes do not function. If the eggs are formed and mature in a timely manner, then there is a chance to conceive a child using IVF. The in vitro fertilization procedure helps a woman become a mother without the participation of a surrogate mother.
Features of the recovery period

Elements of accelerated rehabilitation have been introduced into the work of the gynecological oncology department of UKB 4. One of the aspects of “fact track” surgery is the early activation of the patient, which in such an operation is carried out 5-6 hours after completion of the operation. The patient is allowed to sit down, stand up (the first time under the supervision of medical personnel) and walk if she feels well.
In order to reduce the intensity and relieve pain, intramuscular injections of non-steroidal anti-inflammatory drugs are used, which also contribute to accelerated rehabilitation. Since laparoscopic operations, in comparison with surgical interventions performed by transection, are accompanied by less severe pain, in most cases, the use of narcotic analgesics is not required.
These measures can reduce the risk of postoperative thromboembolic and inflammatory complications, as well as the risk of adhesions.
In addition, all patients are prescribed elastic compression (wearing compression stockings or elastic bandages) to prevent thrombosis of the veins of the lower extremities. Depending on the degree of risk of thromboembolic complications in the postoperative period, low molecular weight heparins or antiplatelet agents may be prescribed, which reduce blood clotting.
As part of rehabilitation therapy, antibacterial drugs are used, as well as agents that normalize intestinal motility and eliminate nausea (if it occurs).
An important point is to follow the correct diet: on the day of the operation, you are not allowed to eat (you can drink still water); for the next 2-3 days, a gentle diet is prescribed until intestinal function is restored.
The following products are not allowed during this period:
- -raw vegetables and fruits;
- -sweets;
- -bakery products;
- -juices, sweet drinks, coffee, carbonated drinks;
- -sweet sour milk products.
If surgical treatment is not associated with an ectopic pregnancy and is not accompanied by intervention on the ovaries (for example, removal of a cyst), menstruation occurs on time (according to the calendar).
However, 1-2 days after chromosalpingoscopy there may be a slight discharge associated with the release of the contrast agent.
The patient spends several days in the hospital (4-6 days), after which she is discharged home (if there are no complications).
It is recommended to limit strenuous physical activity for 21 days after laparoscopy. The duration of sexual rest is determined by the attending physician and depends on the type and extent of the surgical intervention.
In addition, sitz baths, steam baths, saunas, swimming pools, and swimming in the sea are not recommended for about 2 weeks, but the period may vary depending on the extent of the operation and the healing of the sutures.
Sutures are removed 5-7 days after laparoscopy (the day of surgery is not taken into account in the calculation). After this, you can shower completely, including soaking post-operative scars.
At first, the scars are pink in color, then gradually fade and become almost invisible.
Compliance with all doctor’s instructions during the recovery period after laparoscopy helps reduce the likelihood of complications and successful rehabilitation.
Possible complications after laparoscopy

Surgical interventions performed endoscopically are much easier to tolerate by patients and are less likely to lead to complications compared to conventional operations. Despite this, there is a risk of negative consequences. Any surgical intervention can lead to injury to blood vessels or abdominal organs. This leads to bleeding and inflammatory processes of a purulent nature. Other possible complications include:
- damage to the serous covering of the intestine or bladder;
- accumulation of air in the pleural cavity;
- the occurrence of hematomas.
The possibility of complications associated with anesthesia cannot be excluded. Preparatory measures, including a complete thorough examination of the patient and identification of absolute and relative contraindications, can significantly reduce (and in some cases completely avoid) the occurrence of negative consequences.
Before discharge from the inpatient department, the doctor will set a date for a follow-up examination and/or suture removal. If, after returning home, bleeding from the wound, a strong increase in body temperature, vomiting, accumulation of pus in the area of postoperative wounds and dizziness (up to loss of consciousness) are noticed, it is important to immediately contact a specialist.
Doctor's comment
Are you tired of unsuccessfully trying to get pregnant? Did you know that with a diagnosis of infertility, many women today successfully become mothers? In our clinic alone, more than 600 patients who underwent treatment for infertility gave birth to babies. One of the main reasons for unsuccessful attempts to conceive or miscarriage is tubal factor. Of course, to clarify the extent of damage to the fallopian tubes, it is necessary to undergo an examination: hysterosalpingography or laparoscopy, with the help of which you can obtain information about the condition of the uterine cavity and its outer surface, the lumen of the tubes, as well as the pelvic cavity. A comprehensive examination can be performed in our clinic; for this we have the most modern equipment. Make an appointment and together we will discuss all the possibilities for the upcoming treatment, after which we will select the most optimal method based on the examination results.
Head of the surgical service at SwissClinic Konstantin Viktorovich Puchkov