Hysterosalpingography, or x-ray for tubal patency, is performed to study the internal structure of the uterus. This procedure is often prescribed to women who cannot get pregnant; it allows you to get a complete picture of the condition of the fallopian tubes.
In particular, such an examination is recommended in case of problems during pregnancy. Thus, it is possible to identify the causes of pathologies and begin their effective treatment. When it is necessary to check the fallopian tubes, an x-ray is most often performed, because such an examination gives a complete picture of the condition of the main reproductive organs.
Why is the research being conducted?
The fallopian tubes are an element of the female reproductive system that connects the ovaries and the uterus. The main functions of the paired organ are the transport of eggs and sperm, as well as the creation of optimal conditions for the process of conception. It is in the fallopian tubes that the egg is fertilized, after which it moves towards the uterus and is fixed there for further development. If there are problems with the patency of the tubes, the development of a normal pregnancy is impossible.
Hysterosalpingography (HSG) is a painless and informative diagnostic method that allows:
- determine the degree of patency of the fallopian tubes;
- identify anatomical abnormalities of the uterine body;
- detect neoplasms inside the uterine cavity and fallopian tubes.
Today, HSG is the leading diagnostic technique in gynecological practice. Thanks to the results of the study, the obstetrician-gynecologist can not only make an accurate diagnosis, but also determine the tactics for further treatment.
Assessing the degree of patency of the fallopian tubes, the patient may be prescribed conservative, surgical treatment methods, or assisted reproductive technologies may be recommended.
Who is the procedure indicated for?
Indications for the procedure are:
- absence of pregnancy in a woman during a year of active intimate life without the use of contraceptives;
- repeated spontaneous miscarriages;
- a history of ectopic pregnancy;
- preparation for intrauterine insemination - a procedure in which sperm are introduced into the cervical canal or uterus of a woman. This technology is used when a woman is not infertile, but cannot become pregnant naturally. HSG is performed before intrauterine insemination to assess the patency of the fallopian tubes;
- period after surgical interventions on the fallopian tubes. For example, after surgery to eliminate an ectopic pregnancy. HSG allows us to identify the presence or absence of postoperative complications;
- the presence of pathologies of the uterus and fallopian tubes. HSG is performed to monitor the course of diseases;
- suspicion of genital tuberculosis - a disease that occurs when the genital organs are damaged by tuberculosis bacteria with the development of an infectious process;
- suspicion of isthmic-cervical insufficiency. The pathology is characterized by a decrease in the obturator function of the cervix and isthmus, which leads to the inability to keep the fetus inside the uterus;
- suspicion of uterine pathology - benign tumors, endometriosis, hyperplasia (thickening) of the endometrium.
Reviews
Since the procedure is performed frequently, many women have undergone it and have impressions of the study. Here are the reviews patients give:
Maria, 27 years old: “I had MSG last year because I couldn’t get pregnant for two years. Doctors diagnosed adhesions from previous inflammation. After the adhesions were removed, I was allowed to get pregnant, since a repeat study showed the norm.”
Evgeniya, 35 years old: “I had a metrosalpingography done due to a tubal anomaly. Fortunately, the pathology turned out to be operable and in a couple of months I hope to get pregnant.”
Olga, 47 years old: “Due to early menopause, I experienced hormonal changes, pain, and prolonged periods. Doctors suspected a tumor. After MSG, characteristic contours of the uterus were discovered, which confirmed submucosal uterine fibroid. Now they will monitor the growth of the tumor.”
When is the method contraindicated?
The procedure is not carried out:
- during pregnancy. X-rays and contrast agents used during the study have a negative effect on the fetus. In addition, during the procedure, the embryo can be washed out of the uterine cavity or fallopian tubes with a contrast agent;
- with individual intolerance to contrast agents;
- in acute inflammatory processes, exacerbation of chronic pathologies;
- with uterine bleeding;
- with thrombophlebitis - an inflammatory process in the internal venous wall with the formation of a blood clot;
- for renal and heart failure.
Are HSG and ultrasound the same thing?
HSG and ultrasound are two different procedures. An ultrasound examination involves an overview of the patient’s internal organs and detection of possible pathology by changes in their structure and density. The picture is displayed on the monitor. To perform an ultrasound, there is no need to perform any additional procedures. It is enough to simply lubricate the surface being viewed with a special gel.
HSG involves injecting a contrast fluid into the uterus. After its distribution, the doctor performs a series of images using an X-ray machine (but it is possible to examine the internal organs using an ultrasound machine). The introduction of a contrast agent makes the study more informative. In addition, the doctor can diagnose tubal obstruction, which cannot be done during a regular ultrasound examination.
Since two devices can be used to perform HSG: X-ray and ultrasound, there is a difference in the diagnostic process. If the pictures are taken using X-ray equipment, the procedure is called “x-ray hysterosalpingography”. When an ultrasound machine is used to perform the examination, the technique is called “echohysterosalpingography”. Because of the similarity in name, many people believe that these procedures are identical; in fact, their essence and diagnostic significance differ.
Preparation rules
Preparation for the study is as follows:
- A month before the test, you should limit sexual contact or use contraceptives during intimacy. This will prevent pregnancy, in which the method is contraindicated. Even if you cannot get pregnant for many years in a row, you need to protect yourself before the test, because on purpose, a long-awaited pregnancy can occur exactly at the moment when you planned the diagnosis.
- A week before HSG, you should stop using vaginal suppositories.
- Two days before the procedure, foods that can cause flatulence are excluded from the menu: carbonated drinks, dairy products, sweet fruits and berries, some vegetables (cabbage, asparagus, legumes), flour products, sweeteners.
- Before the procedure, careful hygiene of the genital organs is carried out.
Also, preparation for the study includes conducting diagnostic tests:
- blood test for HIV, hepatitis, syphilis;
- gynecological smear for flora.
Cons of GHA
The disadvantages of the procedure are the following:
- A woman receives a dose of radiation, albeit a small one.
- The likelihood of an allergic reaction to the administered contrast agent. Particular caution should be exercised by women with a history of bronchial asthma, as well as allergic patients.
- There is a risk of mechanical damage to the epithelial layer of the uterus, which leads to the appearance of bloody discharge.
How is the procedure done?
The method is safe and does not require hospitalization. The procedure is performed in the first days after the end of menstruation. During this period, the internal mucous membrane of the uterine body is thin, the cervix is pliable, which facilitates diagnostic procedures and improves visibility. Menstrual bleeding must stop completely, otherwise blood clots may blur the picture.
If a study with a contrast agent is performed on a patient for the first time, then an hour before the drug is administered, a test is performed to exclude an allergic reaction.
During the procedure, the woman lies in a supine position on the couch. The doctor inserts gynecological speculum into the woman’s vagina and treats the genitals with antiseptics. Further, the course of the procedure depends on the type of HSG. The study can be carried out using X-ray or ultrasound.
- During X-ray HSG, a contrast agent is injected in portions through a catheter into the area of the fallopian tubes. The doctor takes several x-rays of the fallopian tubes in succession. The X-ray machine is located above the woman's genitals.
- During ultrasound HSG, the fallopian tubes are filled with saline. The ultrasound sensor is inserted vaginally.
The average duration of the procedure is 40 minutes. Ultrasound examination takes longer, but is considered more reliable. Both methods are painless and therefore do not require anesthesia. During the procedure, a woman may only feel discomfort in the lower abdomen.
What is hysterosalpingography
The procedure is often prescribed specifically to diagnose the causes of infertility. There are two types of hysterosalpingography, depending on the method of conducting the study:
- echohysterosalpingoscopy;
- X-ray hysterosalpingography.
Each of the techniques is a method of obtaining an image of the fallopian tubes and/or uterus, their external and internal state. In the first case, the patient is examined by an ultrasound diagnostician using a special scanning machine with an attachment. Before this, a saline solution is injected into the woman's uterus. This method is more suitable for studying the functional characteristics of the uterus. The classic type of examination is x-ray with contrast. It, unlike an ultrasound examination, visualizes the patency of the fallopian tubes.
What are the possible complications after the procedure?
After HSG, the following are possible:
- scanty blood discharge from the vagina, which disappears after a few days;
- mild nausea, dizziness;
- mild pain in the lower abdomen, which in intensity resembles the pain syndrome that occurs during menstruation;
- weakness.
These side effects are completely normal and should not be a cause for concern. In rare situations, high fever, heavy bleeding from the vagina, and severe pain may occur. In case of such complications, you should urgently seek medical help.
Interpretation of results
Analysis of images obtained during the study allows us to identify various pathological conditions. For example, if the fallopian tubes are blocked, the contrast agent will not flow into the abdominal cavity. With partial patency of the fallopian tubes, there will be insignificant effusion into the abdominal cavity.
The method also allows you to assess the condition of the uterus and identify pathologies of the organ. Normally, the organ is completely stained with a contrast agent. With polyps and fibroids, curvature of the contour of the uterus, an increase in its size, and uneven filling of the organ cavity with a contrast agent are observed.
Uterine hypoplasia can also be diagnosed, in which the organ decreases in size. This condition makes it difficult to conceive and carry a pregnancy to term.
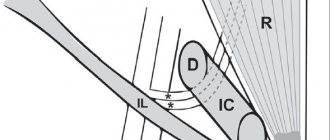
Normal structure and functioning of the fallopian tubes
The fallopian tubes are thin tubes about 8-10 cm long. The wall of the fallopian tube consists of 3 layers - mucous, muscular, serous. The beginning of the fallopian tube originates from the wall of the uterus in the area of the angle and opens with the fimbrial section towards the ovary. The lumen of the fallopian tube expands evenly from the uterus to the ovary, representing a funnel. It is the fimbrial region that plays an important role in capturing the egg and guiding it through the fallopian tube into the uterine cavity. Only with the preservation of the fimbrial part of the fallopian tube, as well as the cilia of the fallopian tube mucosa, is it possible to transport the egg into the uterine cavity.
The egg is not endowed with the ability to move independently through the fallopian tube; only contraction of the fallopian tube and the synchronous movement of the cilia propel the egg into the uterine cavity. If the fimbriae are damaged by an inflammatory and/or adhesive process, then the epithelium may completely or partially lack the ability to capture the egg and move it along the tube. Damage to the ciliated epithelium greatly interferes with fertilization, significantly reducing its chances. Sometimes the fallopian tube is mechanically passable, and when performing tuboscopy, complete destruction of the ciliated epithelium of the fallopian tube is revealed. In such cases, we can talk about the occurrence of an ectopic pregnancy with an externally preserved and patent fallopian tube. In the case when the patency of the fallopian tubes is difficult or the cilia are not able to fully function, there is a possibility of an ectopic (ectopic) pregnancy.

Causes of fallopian tube obstruction
The reasons that lead to obstruction of the fallopian tubes include:
- endometriosis of the ovaries, fallopian tubes, ligaments of the uterus;
- adhesions in the pelvis;
- tubal infection;
- tubal ligation (sterilization).
Complete obstruction occurs when all or part of the pipe is obstructed. The reason for this diagnosis is often pelvic inflammation, which occurs due to a specific or nonspecific infection or external genital endometriosis. With endometriosis, the tissue lining the inner surface of the uterus grows in size outside its cavity. Endometriosis causes obstruction of the tubes and the formation of adhesions in them. With a high degree of development of endometriosis, the likelihood of the spread of adhesions also increases. Symptoms of endometriosis may not be severe in all women. If there is no heavy menstrual flow or the menstrual cycle is accompanied by cramps, the disease is difficult to diagnose. The presence of endometriosis can be reliably determined by laparoscopy.
Fallopian tube infections
Infection of the pelvic organs can occur due to the development of appendicitis or colitis, the presence of an infection in the intestines, or the presence of genitourinary transmitted diseases. Frequent douching can cause an infection in the pelvis, most of which is a nonspecific infection. A woman may not know that she has suffered a serious infection that has led to obstruction of the fallopian tubes. Only when trying to get pregnant does she learn about her illness during the examination process. The most common causes of infections in the pelvis are sexually transmitted diseases.
In past years, gonorrhea was most often detected, currently chlamydia. Repeated infections with chlamydia often lead to infertility due to obstruction of the fallopian tubes. But even a single case may be enough for the patency of the fallopian tubes to be lost.
Modern medicines can relatively easily cure gonorrhea and chlamydia, but the adhesive process in the pelvis cannot be corrected by medication. That is why, when diagnosing infertility, the doctor prescribes a test to detect these infections not only by PCR, but also by determining antibodies in the blood.
Women who do not have infections in the pelvic organs may still experience adhesions in the ovaries and fallopian tubes. Their appearance can be caused by surgery on the ovaries or other abdominal organs, that is, an adhesive process of postoperative origin develops. The likelihood of adhesions increases if the operation was extensive or complicated by infection, accompanied by the placement of drains in the abdominal cavity. For example, a ruptured appendix, massive intra-abdominal bleeding. The sperm may not meet the egg on its way even if the tube is slightly deformed. The likelihood of an ectopic pregnancy also increases.