What infections are hidden?
By latent infection we mean a pathogen that has settled on the mucous surface of an organ (urethra, cervix, intestines) and parasitizes at its expense. He cannot independently produce the proteins necessary to maintain life, so for some time he behaves quietly and does not show symptoms. In 60% of cases, the carrier of the infection finds out that he is sick only when there is a sharp deterioration in health, and the symptoms manifest themselves violently and actively.
Hidden infections include:
- Chlamydia
: incubation period 4 weeks. The route of transmission is sexual. The child becomes infected from the mother during childbirth. - Trichomoniasis
: the No. 1 cause of inflammatory processes in the genitourinary system. - Mycoplasma / ureplasmosis
: sexual transmission and infection is transmitted from mother to child. - Toxoplasmosis: sexual transmission and infection is transmitted from mother to child.
- Candidiasis
: in acute form, it interferes with conception and promotes the penetration of other infections. - HPV
: Causes 99.9% of cervical cancer. - Cytomegalovirus
: often develops during pregnancy due to weakened immunity, causing pathological changes in the structure of the fetus. - Gardnerellosis
(bacterial vaginosis): kills lactic acid beneficial bacteria on the surface of the vagina and creates a breeding ground for the development of pathogenic microflora. - Pyelonephritis: inflammation of the kidneys.
- Bacteriuria: the presence of bacteria in the urine that should not be there indicates diseases of the genitourinary system.
- TORCH infections
(unable to affect an adult, but threatening the life and health of the fetus).
Currently, there are 31 pathogens of latent infection. Each of them is dangerous in its own way.
Intimate - optimal - smear analysis for women
A comprehensive test to evaluate the microflora of the genitourinary tract and detect common infections, including sexually transmitted infections (STIs), genital candidiasis and bacterial vaginosis.
Composition of the study:
09-013 Herpes Simplex Virus 1/2, DNA [real-time PCR] 09-002 Chlamydia trachomatis, DNA [real-time PCR] 09-027 Neisseria gonorrhoeae, DNA [real-time PCR] 09-025 Mycoplasma genitalium, DNA [real-time PCR] 09-026 Mycoplasma hominis, DNA [real-time PCR] 09-031 Ureaplasma parvum, DNA [real-time PCR] 09-032 Ureaplasma urealyticum, DNA [real-time PCR] 09-030 Trichomonas vaginalis , DNA [real-time PCR] 09-001 Candida albicans, DNA [real-time PCR] 09-007 Gardnerella vaginalis, DNA [real-time PCR] 02-003 Microscopic examination of discharge from the genitourinary organs of women (microflora), 3 localizations 09 -184 Human Papillomavirus of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 types), DNA quantitatively, screening to determine the possibility of virus integration into the genome [ real-time PCR]
Synonyms Russian
Comprehensive smear analysis for urinary tract infections in women.
English synonyms
Genitourinary infections;
Sexually transmitted diseases (STD);
Urethral swab test.
What biomaterial can be used for research?
Urogenital scraping.
General information about the study
The microflora of the mucous membrane of the female genitourinary tract (urethra, vagina) is a complex and dynamic environment of microorganisms. To assess the composition of the microflora, timely diagnosis and control of treatment of urinary tract infections, a urethral smear is analyzed. Often there is a combination of infections of the genitourinary system, such as gonorrhea and chlamydia, ureaplasmosis and mycoplasmosis, papillomavirus and herpes infections. For this reason, when examining a woman for infections of the genitourinary system, and even more so when identifying one of these infections, a comprehensive analysis is recommended to exclude or identify all possible infections. The complex analysis includes a microscopic examination of urethral discharge, analysis for all necessary bacterial pathogens (the causative agent of gonorrhea - Neisseria gonorrhoeae, the causative agent of chlamydia - Chlamydia trachomatis, the causative agent of genital mycoplasmosis - Micoplasma genitalium and Micoplasma hominis, the causative agent of genital ureaplasmosis - Ureaplasma urealyticum and Ureaplasma parvum), analysis for all necessary viral pathogens (the causative agent of genital herpes - Herpes Simplex 1/2, the causative agent of human papillomavirus infection and cervical cancer - Human Papillomavirus of high carcinogenic risk), analysis for protozoal infection (Trichomonas vaginalis), analysis for fungal infection (Candida albicans) and testing for bacterial vaginosis (Gardnerella vaginalis).
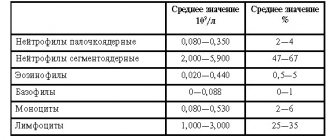
Most of the normal microflora is represented by non-pathogenic bacteria, such as Lactobacilli, Diphteroids, Streptococcus and Peptostreptococcus spp. Some microorganisms (for example, the causative agent of gonorrhea - N. gonorrhoeae or the causative agent of trichomoniasis - T. vaginalis) under no circumstances should be present in the normal microflora of the genitourinary tract. The situation is somewhat more complicated with opportunistic microorganisms, including Gardnerella vaginalis, Candida albicans and Ureaplasma urealyticum. These microorganisms are often detected in small quantities in healthy women of reproductive age who do not show any complaints. However, under certain conditions, opportunistic microflora begins to grow and suppress non-pathogenic microorganisms, which can cause clinically significant bacterial vaginosis, genital candidiasis and ureaplasmosis. Thus, for a full assessment of the microflora of the genitourinary tract, it is necessary to take into account not only the composition, but also the ratio of non-pathogenic, opportunistic and pathogenic microorganisms. This can be done by microscopic examination of the discharge of the genitourinary organs in women.
Many genitourinary tract infections have the same clinical picture, such as vaginal discharge, foul odor and vulvar itching, and it is not possible to identify the etiological agent based on clinical signs. Therefore, laboratory research methods play a leading role in the diagnosis of genitourinary system infections. Identification of the pathogen can be carried out using different methods. One of the most accurate, reliable and fastest diagnostic methods is the polymerase chain reaction (PCR) method. PCR is a molecular diagnostic method that makes it possible to detect fragments of genetic material (DNA) of the infectious agent in biological material (for example, in urethral discharge). The method is highly sensitive and allows the detection of microorganisms even in small quantities. This advantage plays a special role in the diagnosis of sluggish, chronic, “latent” infections, including mycoplasmosis, ureaplasmosis and chlamydia. The method also has high specificity and makes it possible to determine the species of the etiological agent, for example, to accurately differentiate the types of mycoplasmas and ureaplasmas. The high specificity of PCR is especially important in the differential diagnosis of human papillomavirus (HPV) types. Thus, it is known that HPV 6, 11 and 44 are types of low oncogenic risk, are associated with the occurrence of genital warts and do not lead to the development of cervical cancer. On the other hand, HPV 16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 73, 68 and 82 are high-risk HPVs, the presence of which is associated with a high risk of developing cervical cancer. Detection of these types can affect the evaluation and treatment of a woman. To date, PCR is the only method used in clinical practice that allows one to accurately differentiate HPV types. However, the study is not intended for differential diagnosis of high-oncogenic risk HPVs among themselves.
However, the limitations of the PCR method should be noted. Thus, it is not intended to evaluate treatment. This is due to the fact that the study reveals the genetic material of both living and destroyed microorganisms. Therefore, the result of the study will be positive for some time even with successfully selected therapy and after the infection is completely cured.
The detection of pathogens such as N. gonorrhoeae, T. vaginalis, C. trachomatis is always a pathological sign that requires the attention of a doctor. On the other hand, a positive test result for opportunistic microorganisms (C. albicans, Micoplasma spp. and Ureaplasma urealyticum) does not always mean the presence of a clinically significant infection. The result of the analysis should be assessed taking into account additional clinical, laboratory and instrumental data.
What is the research used for?
- For the diagnosis and control of genitourinary tract infections.
When is the study scheduled?
- During a routine examination by a gynecologist;
- in preparation for pregnancy or during it (examination of the first trimester of pregnancy);
- when an STI is detected in a sexual partner;
- if there are complaints of discharge from the urethra or vagina, unpleasant odor, itching in the genital area.
What do the results mean?
Reference values
Microscopic examination of discharge from the genitourinary organs of women (microflora), 3 localizations: https://www.helix.ru/kb/item/02-003#subj12
Candida albicans: https://www.helix.ru/kb/item/09-001#subj12
Chlamydia trachomatis: https://www.helix.ru/kb/item/09-002#subj12
Gardnerella vaginalis: https://www.helix.ru/kb/item/09-007#subj12
Herpes Simplex Virus 1/2: https://www.helix.ru/kb/item/09-013#subj12
Mycoplasma genitalium: https://www.helix.ru/kb/item/09-025#subj12
Mycoplasma hominis: https://www.helix.ru/kb/item/09-026#subj12
Neisseria gonorrhoeae: https://www.helix.ru/kb/item/09-027#subj12
Trichomonas vaginalis: https://www.helix.ru/kb/item/09-030#subj12
Ureaplasma parvum: https://www.helix.ru/kb/item/09-031#subj12
Ureaplasma urealyticum: https://www.helix.ru/kb/item/09-032#subj12
09-184 Human Papillomavirus of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 types), DNA quantitatively, screening to determine the possibility of virus integration into the genome [real-time PCR]: https://www.helix.ru/kb/item/09-184#subj12
Positive result:
| Pathogens | |
| Neisseria gonorrhoeae | Gonorrhea |
| Chlamydia trachomatis | Chlamydia |
| Trichomonas vaginalis | Trichomoniasis |
| Human Papilomavirus of high oncogenic risk | Transient papilloma viral infection Cervical intraepithelial neoplasia Cervical cancer |
| Herpes Simplex Virus 1/2 | Genital herpes |
| Opportunistic flora | |
| Candida albicans | Genital candidiasis Healthy carriage |
| Gardnerella vaginalis | Bacterial vaginosis Healthy carriage |
| Ureaplasma urealyticum and Ureaplasma parvum | Ureaplasmosis Healthy carriage |
| Micoplasma genitalium and Micoplasma hominis | Mycoplasmosis Healthy carriage |
Negative result:
- absence of infection;
- lack of healthy carriers.
What can influence the result?
- The microflora of the genitourinary tract can change depending on the level of estrogen (taking estrogen-containing contraceptives, pregnancy), the phase of the menstrual cycle, sexual activity, and age.
Important Notes
- The detection of opportunistic microorganisms (mycoplasmas, ureaplasmas, yeasts, gardnerella) does not always indicate the presence of a clinically significant infection.
Also recommended
[07-049] Treponema pallidum, antibodies, hypersensitive
[07-032] HIV 1.2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
[40-080] Viral hepatitis. Primary diagnosis
[40-119] Intimate - maximum - smear analysis in women
Who orders the study?
Gynecologist, dermatovenerologist, general practitioner.
Literature
- Larsen B, Monif GR. Understanding the bacterial flora of the female genital tract. Clin Infect Dis. 2001 Feb 15;32(4):e69-77. Epub 2001 Feb 9.
- Holmes KK Sexually Transmitted Diseases / KK Holmes, PF Sparling, WE Stamm; 4th ed. McGraw-Hill, 2008.
- Curtis H. What is normal vaginal flora? Genitourin Med. 1997 Jun; 73(3):230.
What do tests for hidden TORCH infections show?
When a TORCH infection is detected in a woman expecting a baby, she is offered an abortion, because there is a high probability of miscarriage or the birth of a child with serious developmental defects. That is why tests for TORCH infections are taken at the pregnancy planning stage, 2-3 months before conception. In case of a positive result, the expectant mother will take care of her health and eliminate problems, she will have enough time to recover and get pregnant while being healthy. TORCH tests are a mandatory procedure when registering at a antenatal clinic.
TORCH diagnostics is the determination of immunoglobulins (antibodies) that can resist a number of infections.
- IgM antibodies are produced first when foreign microorganisms penetrate, and reach a peak concentration at the end of the 3rd month of infection. They talk about an acute form of the disease. After the 4th month they are not detected. To determine how long a woman has been infected, her IgG antibodies are determined.
- IgG antibodies are produced in response to re-infection or exacerbation of the chronic phase. These immunoglobulins protect the fetus from disease. Their presence indicates a long presence of infection in the body.
A woman takes 8 tests to determine the quantity and quality of IgM and IgG antibodies. Moreover, Ig is the international designation for a foreign body (infection).
Results of tests for the presence of antibodies for hidden infections
| IgG | IgM | What does it mean |
| No | No | Either the body is not infected, or the infection occurred primarily, and antibodies have not been produced. Need monitoring of antibody levels |
| No | discovered | Initial stage of the disease |
| discovered | discovered | Acute form of the disease, monitoring of the type of antibodies is needed |
| discovered | No | The infection has developed immunity, there is no threat to the baby’s health |
For a more accurate prognosis, before the 10th week of pregnancy, a woman is monitored for the level and type of antibodies. The further treatment program depends on its results.
| № | Test for the type of infection | Norm, IU/ml | Infection, IU/ml |
| 1 | IgG to herpes virus type 1 | Less than 16 | More than 22 |
| 2 | IgM to herpes virus type 1 | Less than 0.8 | More than 1.1 |
| 3 | IgG to herpes virus type 2 | Less than 16 | More than 22 |
| 4 | IgM to herpes virus type 2 | Less than 0.8 | More than 1.1 |
| 5 | IgG to cytomegalovirus | Less than 10 | Over 30 |
| 6 | IgM to cytomegalovirus | Less than 0.8 | More than 1.1 |
| 7 | IgG to Toxoplasma | Less than 8 | More than 11 |
| 8 | IgM to Toxoplasma | Less than 0.8 | More than 1.1 |
| 9 | IgG to rubella | Less than 15 | Over 30 |
| 10 | IgM to rubella | Less than 0.8 | More than 1.1 |
| 11 | IgG to parvovirus B19 | Less than 4 | More than 5.5 |
| 12 | IgM to parvovirus B19 | Less than 0.8 | More than 1.1 |
Also, when interpreting the analyses, indicators such as avidity and seropositivity are taken into account.
- Avidity is the severity of the immune response, i.e. how many antibodies are rushed to fight the infection upon initial entry into the body.
- Seropositivity is the presence of antibodies to the infection that has entered the body.
How to prepare for PCR diagnosis of latent infections?
Preparation for PCR diagnostics of latent infections is classic for most tests. To correctly analyze PCR for diagnosing latent infections, you must adhere to the following rules:
- 2-4 hours before the test, refrain from urinating.
- Avoid any sexual contact for 24 hours
- Urine and blood are donated on an empty stomach (morning urine portion)
- The test should be taken before taking medications or diagnostic treatment procedures.
The final analysis is deciphered by your attending physician. The final results will be ready within 1-2 days, in extreme cases - on the day of the tests.
Sign up for PCR diagnostics of hidden infections
Make an appointment
Other tests for detecting hidden infections
There are various methods for identifying hidden infections, which include:
- Laboratory bacterioscopy (smear)
. A smear is taken from the urethra in men and from the vagina in women. The bacteria are placed in a nutrient medium, and the colonies are grown and examined under a microscope. - Enzyme immunoassay ELISA
. The body's responses are studied according to the antigen-antibody principle. - Immunofluorescence reaction (RIF)
. The smear material is stained with special reagents that emit light differently under a fluorescent microscope. - Polymerase chain reaction PCR
. Detects DNA and RNA from a microorganism, allowing you to accurately determine the nature of the infection and the extent of its spread.
Based on the test results, the doctor gives advice and recommendations to the patient. The sooner treatment begins, the sooner recovery will occur.
The material provides general recommendations for taking smears from the urogenital tract for microscopic examination. We ask you to carefully follow these recommendations to improve the accuracy of the study.
Preparation of a smear is the application of discharge obtained from the surfaces of the mucous membranes onto a glass slide. Microscopic examination includes not only the identification of epithelium, microorganisms and other morphological particles, but also an assessment of their number and ratio. The quality of the smear depends on the physiological state of the patient at the time of taking the smear. Clinical material can be the most informative if it is obtained under the following conditions:
- smears were taken in the presence of clinical signs of the disease;
- the patient has not used topical treatment for at least the last 48–72 hours;
- in women, when examining materials from the urogenital tract, it is advisable to take samples approximately in the middle of the menstrual cycle (if the disease does not have obvious manifestations) or on days when there is no bleeding (if the process is exacerbated);
- in men, when studying materials, taking samples from the urethra must be carried out under the condition of urinary retention for at least 3–4 hours;
- the patient has not showered for 24 hours.
Before taking a sample, it is important to understand what material is to be taken and what is expected to be detected. Typically, several clinical specimens (not only for microscopy, but also for other laboratory tests) must be taken during a patient's examination. It is important to remember that:
- Material from the urethra for microscopic examination is taken before all other urethral samples or immediately after taking secretions or samples for culture testing for gonococci.
- The material for preparing a native vaginal smear is taken before all other vaginal tests. The area of the vagina from which the sample should be taken depends on the clinical situation. If there is copious discharge and a trichomonas or candida infection is suspected, a sample is taken from the posterior fornix, where the concentration of the suspected infectious agent is greatest. If the amount of discharge is normal, a sample should be taken from the side of the vagina. This clinical material will provide the most reliable information about the condition of the vagina at the moment.
- A sample from the cervix for microscopic examination is taken before all other cervical samples or immediately after a smear is taken for gonococcal culture.
- Slides must be dry, clean, and not scratched (it is best to use new slides for each new patient).
- The smear is applied in a thin layer to only one side of the slide.
- If the amount of material is small, or you want to place several samples of material on one glass from different locations in one patient, the material should be applied closer to the center of the glass in pre-designated areas.
- The saline solution should be warm (optimally 37°C). This temperature makes it easier to recognize motile Trichomonas.
Clinical material can be obtained using a plastic bacteriological loop or a cotton/Dacron swab. In all cases, preference should be given to Dacron tampons. When using a bacteriological loop, the material is applied to a glass slide in a thin layer using streaking movements. A cotton/Dacron swab is rolled over the glass to transfer the material. All swabs prepared for submission to the laboratory should be air-dried, labeled and, if necessary, recorded.
Taking material for microscopy of native preparations
For microscopy of wet native preparations, vaginal discharge from women is used. In men, direct microscopy of wet smears is performed in the presence of heavy discharge from the urethra with the study of free discharge or flushing.
A vaginal sample for preparing a wet (native) smear is taken in the speculum with a bacteriological loop with a volume of 10 μl from a certain anatomical site (posterior or lateral fornix). Material from the urethra is taken with a bacteriological loop with a volume of 1 μl. The material is taken from the preputial sac with a cotton/Dacron swab.
A drop of warm saline solution (optimally 37°C) is placed on a glass slide. Vaginal or urethral secretions are mixed with a drop of saline, covered with a coverslip, and immediately viewed using a light microscope. If the doctor does not know the method of direct microscopy, the secretions are placed in a tube with warm saline and immediately sent to the laboratory for microscopic examination.
Taking material for microscopy of stained preparations from men
A sample from the urethra for Gram or methylene blue staining is obtained using a 1 µl bacteriological loop. In men, if there is discharge from the urethra, the surface of the glans and the area of the external urethral opening should be cleaned with a gauze swab, the foreskin retracted to prevent contamination. If there are no loose openings, you should ask the patient to lightly massage the urethra with sliding movements from the base of the penis to its head. In this case, a Volkmann spoon or a cotton/Dacron swab can be used to collect material. After inserting the plastic loop into the urethra 1-2 cm, it is necessary to move the plane of the “eye” of the loop towards the opening, lightly pressing on the walls of the urethra. It is not recommended to rotate the loop during the sample collection procedure - this is painful for the patient. After obtaining the clinical material, the loop is placed on the surface of the glass and moved along it several times with light pressure. The loop should leave a thin strip of clinical material on the glass.
A sample is taken from the preputial sac using a cotton/Dacron swab.
Taking material for microscopy of stained preparations from women
A sample from the urethra for Gram or methylene blue staining is obtained using a 1 µl bacteriological loop. If there is a large amount of discharge, the external opening should be cleaned with a gauze swab. If there is no free discharge, a light urethral massage may be performed by a doctor. After inserting the plastic loop into the urethra 1-2 cm, it is necessary to move the plane of the “eye” of the loop towards the opening, lightly pressing on the back and side walls of the urethra. It is not recommended to rotate the loop during the sample collection procedure - this is painful for the patient. After obtaining the clinical material, the loop is placed on the surface of the glass and moved along it several times with light pressure. The loop should leave a thin strip of clinical material on the glass.
A sample from the cervical canal for the preparation of colored preparations is taken in the speculum with a cotton/Dacron swab, a special brush or a Volkmann spoon. It is necessary to thoroughly clean the external opening of the cervical canal using a large gauze swab from vaginal secretions to prevent possible contamination. After inserting the tampon into the cervical canal 1-2 cm, it is rotated several times. The clinical material should be transferred from the swab to the glass in as thin a layer as possible.
For microscopic examination of stained vaginal smears, the material is taken in speculums from the posterior or lateral fornix with a 10 μl bacteriological loop or a Volkmann spoon and distributed in a thin layer on a glass slide.
Taking material from the cervix for oncocytology
The material is taken from two sections: from the external pharynx (ectocervix) and the cervical canal (endocervix) without preliminary treatment of the cervix with a tampon with saline solution . Use an Eyre-type spatula or any other, preferably a special cytobrush. Using rotational movements and light pressure, scrape off the entire surface of the cervix and cervical canal at the same time. A spatula or brush is passed along the glass - two strips are obtained: material from the cervix and the cervical canal. If there is pathology of the cervix, a scraping is taken directly from the affected area. For leukoplakia, erosion, or suspected cancer, at least 2-3 smears must be prepared. In these cases, it is more convenient to take a smear under the control of a colposcope.
Remember, you cannot spread the material in a thick layer - only thin strokes are visible through the microscope. Areas with strong “smearing” are excluded from the study, since it is impossible to qualitatively determine what type of cells are in the resulting mess. On the other hand, do not apply the smear with force, in this case the cells are destroyed and nothing but cell debris is found in the preparation.
Literature: 1. A. M. Savicheva, E. V. Sokolovsky, M. Domeika. The procedure for conducting microscopic examination of smears from the urogenital tract. Methodological recommendations for attending physicians. - St. Petersburg: Publishing House N-L, 2007. - 60 p. (Ex libris Journal of Obstetrics and Women's Diseases series), ISBN 978-5-94869-040-7. 2. “Bulletin of the Laboratory of DNA Diagnostics”, No. 3 (12)/2011, pp. 5-7.
How to take a smear (scraping) from the urethra for infection
If fate has brought you to an appointment with a urologist or venereologist, then you will probably have to do a smear test for sexually transmitted infections or STIs. Many men are frightened by this procedure, so we have set a goal to help you understand this event and not be afraid of this basic research.
Before a smear (scraping) from the urethra, it is advisable not to urinate for about 2 hours. This is necessary in cases where there is no heavy discharge, and in order to obtain a sufficient amount of material, mucus must accumulate in the urethra. Mucus or discharge is needed mainly for the oldest type of diagnosis - microscopy of a smear from the urethra. PCR analysis requires cells obtained by scraping them from the surface of the mucous membrane, so urologists do not always strictly require that one refrain from urinating before collecting the material, and, if the discharge is heavy, they even send the patient to the toilet before the smear.
Since the material is taken from the anterior urethra, the urologist-venereologist may ask you to squeeze out the liquid inside the urethra. The resulting drop is placed on a glass slide directly or taken with a urogenital probe and then applied to the glass. It's absolutely painless!!!
But this is only the first part of the diagnosis - staining and examining a smear from the urethra under a microscope. Fast, not painful, not expensive.
If there is no discharge or the doctor needs to do a PCR test for hidden infections to establish a diagnosis, then you will have to be patient. Because a thin probe is inserted into the urethra to a depth of 1 to 3 cm and scrapes off mucus and urethral cells. Next, the material from the probe is placed on a glass slide and into an Ependorf tube with a nutrient medium for the detection of STIs using the DNA diagnostic method.
One of the types of analysis of a smear (scraping) from the genital tract is bacteriological culture from the urethra. For it, either free secretions or material from the urethra itself are taken. The analysis is taken with a special sterile cotton swab, which is then completely placed in a transport carbon medium, and then onto nutrient media, where the growth of microorganisms present in the urethra occurs. The collection of material is almost painless.
In rare cases, especially in the presence of heavy discharge, severe inflammation of the genital tract and a low individual sensitivity threshold in a man, when it is not possible to take a scraping due to severe pain, we resort to a non-contact method of testing for STIs. That is, the doctor does not insert a probe into the canal, but, after massaging the urethra, 1 portion of urine is taken, which is centrifuged and sent for PCR analysis, microscopy and culture to the laboratory.
After actively collecting material for smear (scraping) analysis, a man may be bothered by some pain when urinating for 1-2 days. In some cases, a drop of blood may appear.
But these unpleasant phenomena quickly pass and should not be an obstacle to your visit to the urologist to take a smear (scraping) from the urethra. Because the consequences of undetected sexually transmitted diseases are much more serious and painful!
Causes of hidden infections in men and women
The content of the article
The main way to get an STI is through unprotected sex, although some diseases (for example, human papillomavirus) can be transmitted by using a condom.
It is important to understand that infection does not occur through seminal fluid, but through contact with mucous membranes. This means that even if sexual intercourse was interrupted and ejaculation did not occur in the woman’s vagina, the exchange of microflora still took place. The composition of the flora is individual for each person and is not always harmless.
The infected partner may not even know that he or she has an STD. Not only does the disease not produce symptoms for a long time, it is also difficult to detect using conventional tests such as a smear for flora or bacterial culture. A person can also simply be a carrier: his immunity does not allow the pathogenic microorganism to multiply, but does not kill it. When it comes into contact with the mucous membranes of a partner with weakened local immunity, the bacteria or virus instantly forms colonies.