Quite often in gynecological practice there are cases when the patient has several problems with the reproductive system. For example, endometriosis and cystic neoplasms, uterine fibroids and ongoing adhesions.
The presence of several diseases at once negatively affects a woman’s reproductive function and leads to secondary infertility. If, after a detailed examination and comprehensive examination, the doctor prescribes surgical treatment, then in some cases laparoscopy and hysteroscopy are indicated simultaneously.
In this article we will describe in detail the essence of these methods, their differences and advantages, as well as when laparoscopy and hysteroscopy are necessary simultaneously for infertility.
What is laparoscopy?
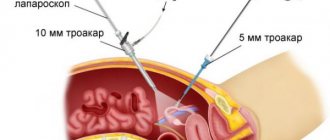
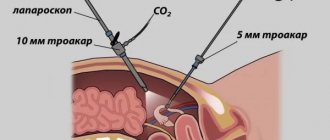
Before talking about the indications for simultaneous laparoscopy and hysteroscopy, we will define these methods. Laparoscopy is a modern type of surgical intervention that is performed in a closed manner. This means that to access the patient's internal organs, the surgeon does not have to make a large incision in the abdomen, as with a laparotomy.
The laparoscopic operation occurs through 3-4 punctures in the abdominal area, through which instruments and a microscopic camera are inserted. It transmits an image magnified 40 times onto the screen in the operating room, which allows you to clearly and clearly view the patient’s internal organs.
Laparoscopy can be diagnostic and therapeutic. In the first case, it allows you to most accurately establish a diagnosis when other research methods have proven unreliable or ineffective. Therapeutic laparoscopy is performed to cure diseases of the reproductive system. Depending on the situation, diagnostic laparoscopy may turn into therapeutic laparoscopy if the diagnosis is confirmed and the surgeon deems it appropriate.
What methods exist for checking the patency of the fallopian tubes?
- Echosalpingography (sonohysterosalpingography)
- Hysterosalpingography (also known as metrosalpingography)
- Laparoscopy (including transvaginal laparoscopy)
Echosalpingography
Echosalpingography is one of the simplest research methods, performed using ultrasound. A thin rubber catheter is inserted into the uterine cavity, and a saline solution is injected through it using a syringe. Using an ultrasound, the doctor sees the fluid in the uterine cavity, and how it passes through the fallopian tubes - how quickly it fills them and pours into the abdominal cavity. The procedure usually takes no more than 10–15 minutes, is practically painless, but can sometimes be accompanied by slight aching pain in the lower abdomen.
Discomfort often occurs in the presence of an adhesive process; in this case, a solution under pressure can separate thin adhesions. Sometimes this even helps to improve the patency of the tubes, and it is not uncommon for a woman to have a long-awaited pregnancy after this study. But you still shouldn’t rely on echosalpingography as a method of therapy in the presence of obstruction of the fallopian tubes; more often than not, “blowing the tubes” in this way turns out to be at least simply ineffective, and is often associated with the risk of developing an ectopic pregnancy.
X-ray examination of fallopian tube patency
X-ray examination of the patency of the fallopian tubes (hysterosalpingography or metrosalpingography) consists of introducing a water-soluble radiopaque substance into the uterine cavity, followed by an x-ray that evaluates its distribution in the pelvic cavity. There are many types of solutions, all of them containing iodine, so this procedure is possible only in the absence of an allergic reaction to iodine preparations.
The technique of hysterosalpingography is as follows: the procedure is performed without anesthesia in a specially equipped room. A metal catheter is inserted into the woman’s cervical canal, through which 2 ml of a contrast agent is poured into the uterine cavity, after which an X-ray is taken. Then an additional few ml of contrast is injected and a repeat image is taken.
On average, the entire procedure takes about 30 minutes. The image shows the uterine cavity and fallopian tubes along their entire length, filled with contrast. Based on the shape of the fallopian tubes, their filling, and the location of the contrast in the pelvic cavity, it is possible to determine the presence of an adhesive process, and if there is obstruction, in which part of the fallopian tube it occurred. The advantages of such a study are its significantly greater accuracy, compared to ultrasound salpingography, and the fact that you still have pictures of your pipes in your hands, which can be viewed by any specialist even in a few years. The disadvantages include the fact that it is associated with more pronounced discomfort due to the technical features of the procedure.
Laparoscopy
Laparoscopy is the most accurate method for examining the patency of the fallopian tubes, the most valuable factor of which is that it is possible to immediately eliminate almost all defects that are identified, from adhesions to foci of endometriosis. In addition, there is no moment of spasm of the smooth muscles of the tubes in response to a painful stimulus, which can simulate tubal obstruction during echosalpingography or HSG, since laparoscopy is performed under anesthesia and the muscles are completely relaxed. But this is already a full-fledged surgical intervention, so it will be discussed separately.
Differences between laparoscopy and hysteroscopy
When a woman is prescribed laparotomy and hysteroscopy simultaneously for infertility, she should understand that these are two fundamentally different methods with different types of access to the organs of the reproductive system. What they have in common is that these are minimally invasive and gentle procedures. On the Internet on various medical sites and forums there are reviews about laparoscopy and hysteroscopy at the same time, which are not true. We strongly advise you not to listen to online advisors, but to contact your doctor, who will provide the most up-to-date and reliable information.
The main differences between laparoscopy and hysteroscopy:
- Laparoscopy requires longer anesthesia than hysteroscopy;
- The operation using the laparoscopic method is performed through punctures in the abdomen, while hysteroscopy takes place without a single incision;
- Laparotomy provides wider access to internal organs and makes it possible to perform surgical manipulations both inside and outside the uterus.
According to patient reviews, laparoscopy and hysteroscopy at the same time is an excellent opportunity not only to save time, but also to cope with several problems at once. In addition, two operations at a time prevents repeated anesthesia, which is not always easily tolerated by the body.
Laparoscopy and hysteroscopy simultaneously may be indicated in cases where the patient has several diseases of the internal genital organs. It could be:
- Endometriosis and endometrioid ovarian cyst;
- Uterine fibroids accompanied by obstruction of the fallopian tubes;
- Endometriosis and myomatous nodes;
- Paraovarian cyst and extensive adhesions.
To find out more information about the procedure of laparoscopy and hysteroscopy simultaneously for infertility, we advise you to consult our specialists. You can make an appointment on the website or by phone.
Laparoscopy and IVF surgery
Laparoscopy is a minimally invasive surgical procedure that allows the doctor to visually assess the condition of the organs being studied and, if necessary, perform surgery.
At the moment, laparoscopy is the “gold standard” for the diagnosis and treatment of a large number of gynecological diseases.
Make an appointment

Features of the procedure
Laparoscopy is a procedure that is performed using special microsurgical instruments and an optical system. It involves the penetration of a laparoscope into the abdominal cavity through incisions of minimal length.
There are diagnostic and surgical options for this intervention. The first, if necessary, can move into the second.
During laparoscopy, the following diseases can be treated:
- Endometriosis.
- Adhesive process.
- Cystic lesion of the ovaries.
- Myomatous nodes.
Laparoscopy is currently a very popular method in the diagnosis and treatment of gynecological diseases. The high safety and effectiveness of the procedure determine its popularity among doctors. Laparoscopy is characterized by low trauma, low risk of complications, and rapid rehabilitation of the patient after surgery.
IVF and laparoscopy surgery
Laparoscopy before IVF in some situations can be a factor that significantly increases the chance of a successful conception. There are a number of situations when this operation is justified. These are:
- Adhesive processes in the pelvic area.
- Endometriosis of various localizations.
- Formation of neoplasms in the pelvis.
- Inflammation of the fallopian tubes.
- Cystic lesion of the ovaries.
These pathologies require laparoscopic surgery. IVF without prior surgical intervention may be unsuccessful, or the pregnancy may be terminated.
A woman should decide whether to undergo laparoscopy before IVF after consultation with a doctor. A reproductive specialist will be able to explain all the features of a specific clinical situation and suggest what to do correctly to increase the chances of a successful procedure.
If the doctor predicts that IVF without laparoscopy is likely to be ineffective, he will prescribe surgery. Only after treatment and completion of a rehabilitation course will a woman be able to enter into the protocol.
Advantages
Laparoscopy is one of the most popular treatment methods in modern gynecology. With the help of this operation, the diagnosis and elimination of many pathologies is carried out. With the development of medicine, this operation is becoming increasingly safer for the patient.
The main advantages of laparoscopy are:
- Low morbidity.
- Speed of the procedure (on average lasts 30 minutes).
- Visual inspection by a doctor. As a result, there is a minimal risk of damage to healthy tissue.
- Fast rehabilitation.
- Good aesthetic effect.
As a diagnostic method, laparoscopy has the greatest information content compared to other techniques.
IVF or laparoscopy?
In some situations, a woman is faced with a choice: laparoscopy or IVF. This is possible if conception naturally is impossible without surgical intervention, but a high chance of pregnancy is predicted after in vitro fertilization. In this case, the woman chooses, weighing all the pros and cons.
Advantages of laparoscopy:
- Natural fertility is restored.
- The price is lower than IVF.
- You don't need your husband's participation.
Disadvantages of laparoscopy:
- The need for surgery (possible: risk of complications, postoperative pain).
- You can become pregnant after surgery not immediately, but after some time.
- Fertility may not be restored, and then IVF will still have to be done.
Disadvantages of IVF:
- Natural fertility is not restored, but pregnancy is only achieved.
- Higher price.
- The participation of the husband is required (he also needs to undergo an examination and also donate sperm for fertilization).
Benefits of IVF:
- You can start the procedure immediately if there are no contraindications.
- Safety (with proper examination and correct selection of ovarian stimulation regimens).
- High efficiency.
IVF after laparoscopy
Almost all patients who decide to undergo this operation immediately ask how long it takes to do IVF after laparoscopy. They want to know how quickly they can get pregnant.
It is impossible to give a definite answer. In each case, everything is individual and depends on quite a large number of factors.
When IVF is possible after laparoscopy is influenced by:
- The severity of the pathology.
- Features of the disease that was eliminated surgically.
- General condition of the patient.
- Woman's age.
- Presence of concomitant pathology.
- Individual characteristics of the body.
In some cases, IVF is allowed to be performed as early as 2 months after surgery. In other situations you have to wait longer. If laparoscopy was performed, only your attending physician will tell you how long it will take to do IVF.