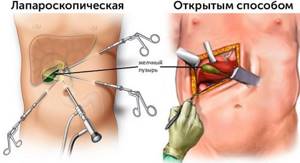
Cholecystectomy is a surgical procedure during which the gallbladder is removed. In modern clinics, it is usually performed laparoscopically - without an incision, through small punctures in the abdominal wall. For a surgeon with appropriate experience, this is a routine operation and does not present any difficulty. Patients tolerate laparoscopic cholecystectomy well, and the risk of complications is low. Discharge from the hospital can occur the very next day after the intervention.
Our expert in this field:
Allahverdyan Alexander Sergeevich
Surgeon-oncologist, professor, MD. Head of the ROH expert group. International expert
Call the doctor Reviews about the doctor
Open cholecystectomy through an incision is accompanied by slightly higher risks, and the recovery period is longer. Currently, this type of operation is used only in certain cases.
Indications for cholecystectomy
The gallbladder is a small sac-like organ located on the undersurface of the liver. Its volume in an adult reaches 50–60 cm³. Anatomically, it distinguishes between the bottom, body and neck, which passes into the cystic bile duct. The latter connects with the common hepatic duct, and together they form the common bile duct. Connecting with the pancreatic duct, it flows into the duodenum.
The gallbladder is needed to store bile. When food enters the duodenum from the stomach, it contracts and secretes 40–60 ml of bile. This is necessary for normal digestion. However, the gallbladder, affected by a pathological process, ceases to perform its job normally and becomes only a source of problems: it causes pain, turns into a reservoir for infection, and disrupts the function of the biliary tract and pancreas. Cholecystectomy helps to completely get rid of all symptoms in 90–95% of cases.
One of the most common indications for cholecystectomy is cholelithiasis. Surgical treatment is used when there are stones in the gallbladder that cause symptoms:
- Attacks of biliary colic - acute, sharp, very severe pain under the right rib. In 2/3 of patients, after the first such attack, a repeat attack occurs within two years. Some subsequently develop serious complications. If episodes of acute pain recur, this is a clear indication for surgery.
- “Minor” symptoms: bitter taste in the mouth, feeling of discomfort, heaviness under the right rib after eating, aching pain. In 6–8% of these patients each year, conditions requiring emergency surgical treatment arise, so the doctor may suggest elective cholecystectomy.
If gallstone disease does not cause symptoms, then surgical treatment may be recommended for large stones (2.5–3 cm - due to the risk of bedsores), hemolytic anemia, surgery for obesity (the course of gallstone disease may worsen after sudden weight loss), when the patient's life expectancy is more than 20 years (since the risk of complications increases over time).
Other indications for elective cholecystectomy:
- Chronic calculous cholecystitis is the formation of stones in the gallbladder and inflammation of its wall. The disease most often occurs in older women.
- Polyps are abnormal growths on the wall of the gallbladder. The causes of their occurrence are not fully understood; they often do not cause symptoms and are an incidental finding during ultrasound.
- “Porcelain” gallbladder is a condition in which the wall of the organ is covered with a layer of calcium. Its main cause is prolonged inflammation. These patients have an increased risk of developing a malignant tumor.
- An attack of acute cholecystitis. Elective cholecystectomy is recommended to be performed within the next 4–6 weeks, with a maximum of 12 weeks.
- An attack of acute biliary pancreatitis , an inflammation of the pancreas caused by problems with the gallbladder. Usually the causes are gallstones, inflammation, and anatomical features. The patient is prepared for surgery as soon as the manifestations of pancreatitis subside.
- Acalculous cholecystopathy (gallbladder dyskinesia) is a disorder of gallbladder motility, which is accompanied by painful symptoms. This indication is not absolute. In Russia, cholecystectomy is performed only in certain cases when drug therapy is ineffective.
- Gallbladder cancer. For malignant tumors, extended radical cholecystectomy is usually performed. Often the gallbladder is removed for another reason, and after the operation, tumor cells are found in it based on the results of a biopsy.
Urgent removal of the gallbladder - within the next 48-72 hours - is indicated for acute cholecystitis, when medications do not help or complications have developed. This is a dangerous pathology that kills up to 1–6% of patients. Acute cholecystitis can be complicated by such life-threatening conditions as necrosis (death), perforation (formation of a through hole) of the gallbladder wall and the development of peritonitis (inflammation in the abdominal cavity), intraperitoneal abscess (ulcer), sepsis (systemic inflammation - “blood poisoning” ).
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
Contraindications
If we are talking about saving the patient’s life, then cholecystectomy through the incision can almost always be performed. Laparoscopic interventions have more contraindications.
The main absolute contraindications include the patient’s very poor, terminal condition, severe disorders of the internal organs, uncontrolled coagulopathy (deterioration of blood clotting), which threatens dangerous bleeding during surgery.
In some cases, cholecystectomy can only be performed openly:
- cicatricial changes or severe inflammation in the gallbladder;
- adhesions in the abdominal cavity;
- concomitant pathologies that require a full examination of the abdominal cavity;
- difficult visibility during laparoscopy due to anatomical features;
- bleeding during surgery;
- malformations of the biliary system;
- widespread peritonitis.
Technologies are improving, so the indications for laparoscopic cholecystectomy have expanded significantly in recent years. Thus, this type of operation has become possible to perform in elderly people, pregnant women (safest in the second trimester), obese people with cirrhosis of the liver (but not always), acute cholecystitis, and previous operations on the abdominal organs. Make an appointment with a surgeon at the Medica24 international clinic: the doctor will assess your situation and determine the optimal surgical tactics.

Preparing for surgery
To decide on the need for cholecystectomy, it is necessary to conduct an examination of the biliary system. The doctor may prescribe ultrasound, endoultrasonography (ultrasound using a probe located at the end of an endoscope), magnetic resonance cholangiography, endoscopic retrograde cholangiopancreatography (ERCP) and other diagnostic procedures.
Then, during a preliminary consultation, the surgeon explains to the patient what type of intervention is planned to be performed, why it is needed, and what the expected result is. The patient must tell the doctor about his concomitant diseases, allergic reactions, and medications that he constantly takes.
Next, the doctor sets a date for hospitalization and surgery, gives a list of studies and tests that need to be completed as part of the preoperative examination. It usually includes general blood and urine tests, a biochemical blood test, a blood coagulation test, tests for HIV, syphilis and viral hepatitis, determination of blood group and Rh factor, ECG, fluorography, consultation with a therapist and, if necessary, other medical specialists.
The night before surgery, a light dinner before 7 p.m. is recommended. Then you cannot eat or drink anything, because the intervention is performed under general anesthesia. In the evening and in the morning they do a cleansing enema. In the morning you need to take a shower.
In acute cholecystitis, preoperative preparation is carried out in an accelerated manner and is limited to the minimum required set of procedures.
How is cholecystectomy performed?
There are different techniques for performing cholecystectomy, each of which has its own advantages and disadvantages and is optimal in certain cases.
Laparoscopic cholecystectomy
Currently, gallbladder removal is most often performed laparoscopically. Typically, the operation is performed through 3-4 punctures in the abdominal wall; in some cases, more may be required. One of the punctures is made in the navel area, through which a laparoscope is inserted - an instrument with a video camera and a light source. An insufflator is also connected to the laparoscope, through which the abdominal cavity is filled with carbon dioxide. This is necessary to provide the surgeon with a good view and space for manipulation.
Special surgical instruments are inserted through the remaining punctures. They are used to carefully isolate the cystic duct and artery, clamp them with clips and cross them. After the gallbladder is isolated, it is removed through one of the punctures.
When the operation is completed, the instruments are removed and stitches are placed on the punctures.
Operation through one puncture
In recent years, an improved method of laparoscopic removal of the gallbladder - single-port cholecystectomy - has been actively developing. In this case, only one puncture is made in the navel area. A laparoport is installed into it, through which several instruments can be inserted at once. Such interventions are optimal for uncomplicated chronic calculous cholecystitis. Their main advantage is an excellent cosmetic effect and the absence of a noticeable scar.
Open cholecystectomy
In an open cholecystectomy, the surgeon makes a vertical incision in the middle of the abdomen (midline laparotomy) or an oblique incision under the right lower costal arch. The gallbladder is isolated, ligated (or clipped) and divided in the same way as during laparoscopic surgery.
As noted above, in some cases open surgery is the best option, because during it the surgeon can fully examine the gallbladder and neighboring organs, as well as conduct intraoperative studies:
- probing the bile ducts and measuring their width;
- cholangiography;
- choledochotomy (opening of the bile ducts) and endoscopic examination;
- ultrasonography.
Minimally invasive open cholecystectomy
In some cases, it is possible to perform a minimally invasive operation, limiting yourself to a small incision 3–5 cm long in the right hypochondrium. This intervention has many of the advantages of open cholecystectomy, but is accompanied by less tissue trauma and shorter hospitalization and recovery periods.
Extended radical cholecystectomy
This is the most complex operation used for malignant tumors. If only the gallbladder is removed during cancer, then the risk of relapse is high. The minimum scope of the operation involves removing the gallbladder, several centimeters of adjacent liver tissue, and all nearby lymph nodes.
In some cases, the following may be removed: part of the liver, common bile duct, pancreas, additional groups of lymph nodes, duodenum and other organs affected by a malignant tumor.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
Recommendations after cholecystectomy - diet after removal of the gallbladder
It is recommended to take choleretic drugs (decoction of rosehip, immortelle, corn silk) ½ cup 15-20 minutes before meals for a month, enzymatic drugs (festal, mezim-forte, panzinorm) 1 tablet with meals. Specific recommendations are obtained from the attending physician and the operating surgeon.
The advantages of the laparoscopic technique for performing cholecystectomy are obvious and virtually no one doubts it. Currently, more than 90% of operations for cholelithiasis in the world are performed laparoscopically. With this method, there is virtually no postoperative pain, an excellent cosmetic result is observed, and the hospital stay and disability period are several times shorter.
Laparoscopic cholecystectomy is the most common endosurgical operation in Russia.
As for the cost of surgery to remove the gallbladder, prices in Moscow vary greatly. It all depends on the qualifications of the specialist who performs the operation, the method, stage of the disease, and the use of various drugs during surgery.
In the surgery department of the International Medical Center in Khimki, depending on the characteristics of the disease, stage, contraindications and concomitant ailments, specialists will offer one or another method of gallbladder removal that is suitable for you.
When you contact Clinic No. 1 in Khimki, you are guaranteed to receive truly high-quality medical care. Be sure that you trust your health to real professionals who will definitely help in any situation. We will find a reliable, effective, and most importantly, the safest method of solving any of your health problems.
- Available: doctor’s appointment from 1500 rubles
- Convenient: open daily from 8:00 to 21:00
- Quickly: we will carry out all the diagnostics at the first appointment
- Complete: has all the necessary equipment
The surgery clinic in Khimki performs the following operations:
- cholecystectomy (open laparoscopic): surgery to remove the gallbladder
- treatment of ingrown toenails;
- hernia removal;
- treatment of boils and carbuncles;
- removal of fibroids;
- removal of a wen (lipoma);
- removal of atheroma;
- wart removal:
- removal of papillomas;
- treatment and removal of calluses and corns;
- treatment and removal of scars and scars
Prices for services
| Name | Time | Price | |
| Surgeon appointment, treatment and diagnostic, primary, outpatient | 1500 | ||
| Surgeon appointment, therapeutic and diagnostic, repeated, outpatient | 1000 | ||
| Removal of cat. I lipoma. difficulties | 5500 | ||
| Removal of lipoma category II. difficulties | 11000 | ||
| Removal of category III lipoma. difficulties | 19800 | ||
| Removal of lipoma IV category. difficulties | 30800 | ||
| Atheroma removal category 1 | 2420 | ||
| Removal of atheroma category 2 | 4235 | ||
| Removal of atheroma category 3 | 6050 | ||
| Biopsy of cutaneous elements using a radioknife | 660 | ||
| Suture (1 pc.) | 300 | ||
| Excision of skin elements and formations (1 element) - Cat. I. difficulties | 2450 | ||
| Excision of skin elements and formations (1 element) - Category II. difficulties | 4250 | ||
| Excision of skin elements and formations (1 element) - Cat. III. difficulties | 6655 | ||
| Intradermal suture, category 1 | 610 | ||
| Excision of subcutaneous formations with sutures - Cat. I. difficulties | 3630 | ||
| Excision of subcutaneous formations with sutures - Category II. difficulties | 5500 | ||
| Intradermal suture, category 2 | 1210 | ||
| Excision of subcutaneous formations with sutures - Cat. III. difficulties | 7260 | ||
| Applying an aseptic dressing | 385 | ||
| Cosmetic suture application | 1815 | ||
| Applying a medicinal dressing | 605 | ||
| Dressing using high-tech dressings | 550 | ||
| Suturing the eyelids | 1815 | ||
| Stitching | 1320 | ||
| Operations for ingrown toenails, matrixectomy (1 zone) - Cat. I. difficulties | 2420 | ||
| Operations for ingrown toenails, matrixectomy (1 zone) - Category II. difficulties | 4235 | ||
| Operations for ingrown toenails, matrixectomy (1 zone) - Cat. III. difficulties | 5445 | ||
| Open (surgical) lymph node biopsy - Cat. I. difficulties | 6050 | ||
| Open (surgical) lymph node biopsy - Cat. II. difficulties | 9680 | ||
| Open (surgical) lymph node biopsy - Cat. III. difficulties | 14520 | ||
| Washing of cavity drainages, fistulas | 429 | ||
| Primary surgical treatment of the wound, revision - Cat. I. difficulties | 1430 | ||
| Primary surgical treatment of the wound, revision - Cat. II. difficulties | 3025 | ||
| Primary surgical treatment of the wound, revision - Cat. III. difficulties | 6050 | ||
| Dressing of a postoperative wound - Cat. I. difficulties | 715 | ||
| Dressing of a postoperative wound - Cat. II. difficulties | 1210 | ||
| Dressing of a postoperative wound - Cat. III. difficulties | 1815 | ||
| Radiosurgical excision of warts - Cat. I. difficulties | 1045 | ||
| Radiosurgical excision of warts - Cat. II. difficulties | 1815 | ||
| Radiosurgical excision of warts - Cat. III. difficulties | 3025 | ||
| Removal of stitches up to 4 pieces (I category) | 880 | ||
| Removal of foreign bodies from soft tissues - Cat. I. difficulties | 1430 | ||
| Removal of foreign bodies from soft tissues - Cat. II. difficulties | 3025 | ||
| Removal of soft tissue formations - Cat. I. difficulties | 1450 | ||
| Removal of foreign bodies from soft tissues - Cat. III. difficulties | 5445 | ||
| Removal of soft tissue formations - Cat. II. difficulties | 3025 | ||
| Removal of skin elements using radiosurgical method - Cat. I. difficulties | 1210 | ||
| Removal of soft tissue formations - Cat. III. difficulties | 4500 | ||
| Removal of cutaneous elements using radiosurgical method - Category II. difficulties | 3025 | ||
| Removal of cutaneous elements using radiosurgical method - Cat. III. difficulties | 4235 | ||
| Radiosurgical removal of nevus - Cat. I. difficulties | 1210 | ||
| Radiosurgical removal of nevus - category II. difficulties | 2420 | ||
| Radiosurgical removal of nevus - category III. difficulties | 3630 | ||
| Radiosurgical removal of nevus - IV category. difficulties | 7260 | ||
| Removal of recurrent nevus | 2420 | ||
| Nail removal - Cat. I. difficulties | 1815 | ||
| Nail removal - Cat. II. difficulties | 2420 | ||
| Nail removal - Cat. III. difficulties | 3025 | ||
| Surgical treatment of purulent-inflammatory processes - Cat. I. difficulties | 3630 | ||
| Surgical treatment of purulent-inflammatory processes - Cat. II. difficulties | 5445 | ||
| Surgical treatment of purulent-inflammatory processes - Cat. III. difficulties | 7865 | ||
| Surgical treatment of purulent-inflammatory processes - IV category. difficulties | 10285 | ||
| Extended consultation with a surgeon with drawing up a treatment plan | 1650 | ||
| Thyroid puncture | 1700 | ||
| Prostate puncture | 5665 | ||
| Lymph node puncture | 1430 | ||
| Excision of the coccygeal passages category 2 | 24200 | ||
| Excision of coccygeal passages category 3 | 30800 | ||
| Removal of sutures, up to 8 pieces (II category) | 1100 | ||
| Removal of sutures, more than 8 pieces (III category) | 1320 | ||
| Dressing of a wound, bedsore, trophic ulcer, etc. Category I | 715 | ||
| Dressing of wounds, bedsores, trophic ulcers, etc. II category | 1210 | ||
| Dressing of a wound, bedsore, peat ulcer, etc. III category | 1815 | ||
| Excision of bedsores category I | 2200 | ||
| Excision of bedsores category II | 3520 | ||
| Excision of bedsores category III | 4950 | ||
| Excision of bedsores category IV | 7150 | ||
| Anoscopy | 825 | ||
| Proctological dressing category II | 1870 | ||
| Removal of telangiectasias with an area of 1 square. see by radiosurgery method | 3025 | ||
| Surgical separation of synechiae NPO | 3630 | ||
| Surgeon appointment is preventive, outpatient | 550 | ||
| Repeated reception of CMN | 1600 | ||
| Initial reception of CMN | 2000 | ||
| Calling a doctor to your home without the cost of manipulations (Khimki, Starbeevo, Ivakino, Naberezhnye) | 3850 | ||
| Calling a doctor to your home without the cost of manipulations (Skhodnya, Podrezkovo, Novopodrezkovo, Planernaya station, Firsanovka) | 4950 | ||
| Calling a doctor to your home without the cost of manipulations (Kurkino, Novogorsk) | 4400 | ||
| Calling a doctor to your home without the cost of manipulations (Left Bank, Moscow, within the Moscow Ring Road) | 6000 | ||
| Medical consultation | 3300 | ||
| Consultation with the head of the surgical department | 0 | ||
| Extract from outpatient card | 660 | ||
| Consultation (interpretation) with analyzes from third parties | 1300 | ||
| Consultation on treatment adjustments | 550 | ||
| Breast puncture | 2200 | ||
| Salivary gland puncture | 1700 | ||
| Puncture of the pleural cavity (1 cavity) | 3850 | ||
| Excision of fistulas - III category of difficulty | 24200 | ||
| Phlebectomy of the GSV | 33000 | ||
| Phlebectomy of the SVC | 30800 | ||
| Hospital stay (days) | 4400 | ||
| Three meals a day (hospital) | 1650 | ||
| Hernioplasty of hernia of the white line with alloplasty mesh category 1 | 50900 | ||
| Hernioplasty of hernia of the white line with alloplasty mesh category 2 | 57400 | ||
| Hernioplasty of hernia of the white line with alloplasty mesh category 3 | 64050 | ||
| Hernioplasty of postoperative, ventral hernia with category 1 mesh | 61800 | ||
| Hernioplasty of postoperative, ventral hernia with category 3 mesh | 82700 | ||
| Hernia repair of femoral hernia with mesh alloplasty | 50900 | ||
| Hernia repair of femoral hernia with local tissue repair | 35400 | ||
| Hernia repair of inguinal hernia with local tissue repair | 35400 | ||
| Hernia repair of inguinal hernia with plastic surgery according to Liechtenstein category 1 | 45500 | ||
| Hernia repair of inguinal hernia with Liechtenstein category 2 repair | 54800 | ||
| Hernia repair of inguinal hernia with Liechtenstein category 3 repair | 60200 | ||
| Hernia repair of inguinal-scrotal hernia with plastic surgery according to Lichtenstein | 71500 | ||
| Hernia repair of umbilical hernia with local tissue repair (according to Sapezhko, Mayo) | 30100 | ||
| Hernia repair of umbilical hernia with plastic surgery of the anterior abdominal wall with mesh, category 1 | 50358 | ||
| Hernia repair of umbilical hernia with plastic surgery of the anterior abdominal wall with mesh, category 2 | 57700 | ||
| Hernia repair of umbilical hernia with plastic surgery of the anterior abdominal wall with mesh category 3 | 63100 | ||
| Electrocoagulation of hemorrhoidal fimbriae (1 piece) | 7480 | ||
| Hemorrhoidectomy category I | 19800 | ||
| Hemorrhoidectomy category II | 27500 | ||
| Hemorrhoidectomy category III | 36300 | ||
| Opening and drainage of subcutaneous paraproctitis | 13860 | ||
| Excision of anal fissures | 24200 | ||
| Laparocentesis | 10890 | ||
| Electrocoagulation of anal papillomas 1 piece | 1650 | ||
| Inpatient treatment (1 bed day) | 1900 | ||
| Dressing (traumatology) category 1 | 925 | ||
| Dressing, removal of category 1 stitches | 759 | ||
| Anesthesia aid category 1 | 12400 | ||
| Roux-en-Y hepaticojejunostomy with controlled Voelker drainage | 350000 | ||
| Relaparotomy. Suturing the liver defect, sanitation and drainage of the abdominal cavity | 350000 | ||
| Ligation of 1 hemorrhoid with a latex ring | 4400 | ||
| Appointment with a proctologist, therapeutic and diagnostic, primary, outpatient | 1500 | ||
| Appointment with a proctologist, therapeutic and diagnostic, repeated, outpatient | 1000 | ||
| Removal of hemorrhoidal thrombus | 3850 | ||
| Sclerotherapy 1 session | 4235 | ||
| Sclerotherapy of 1 spider vein | 1210 | ||
| Sclerotherapy of 1 spider vein (“Surgitron”) | 715 | ||
| RFA of the GSV trunk, (including local anesthesia) | 33000 | ||
| RFA of two basins of the main saphenous veins on one lower limb (GSV + SSV) | 44000 | ||
| RFA of the main saphenous vein with difficult access/several punctures | 44000 | ||
| Miniphlebectomy category 1 (single perforating veins, single inflow up to 0.7 cm) | 11000 | ||
| Miniphlebectomy category 2 (perforating and dilated veins, 2 or more incompetent tributaries up to 0.7 cm) | 16500 | ||
| Miniphlebectomy category 3 (multiple perforating veins and dilated, incompetent tributaries more than 0.7 cm) | 22000 | ||
| Crossectomy | 11000 | ||
| Stripping | 27500 | ||
| Crossectomy+stripping | 33000 | ||
| Using VCP for RFA | 16500 | ||
| Treatment and diagnostic appointment with a neurosurgeon, primary, outpatient | 2750 | ||
| Treatment and diagnostic appointment with a neurosurgeon, repeated, outpatient | 1650 | ||
| Appointment with a phlebologist, therapeutic and diagnostic, primary, outpatient | 1500 | ||
| Appointment with a phlebologist, therapeutic and diagnostic, repeated, outpatient | 1000 | ||
| Flushing the drainage catheter (liver bile drainage) | 3500 | ||
| Rectoscopy | 2500 | ||
| Expand all prices | |||
Rehabilitation period
4-6 hours after laparoscopic cholecystectomy, the patient is allowed to get out of bed and drink water in small portions. The next day the patient can move freely and is allowed to take liquid food. Many patients are discharged home after one night in hospital, while others are kept for another day.
Usually, after removal of the gallbladder, a drain is left in the abdominal cavity - a tube for the outflow of fluid. It is removed the next day. In the first days, pain may be bothersome; they are relieved with painkillers. In some patients, antispasmodics are used for a week. The doctor may also prescribe medications that improve the properties of bile.
You need to stick to a diet for a month after surgery. Tea and coffee, fatty, fried foods, sweets, and any drinks containing alcohol are prohibited. Then the patient gradually returns to his usual diet under the supervision of a gastroenterologist. Also, for a month you need to limit physical activity: avoid straining the abdominal muscles, do not lift loads heavier than 3-4 kg.
After an open cholecystectomy, the patient spends more time in the hospital, and the rehabilitation period lasts longer.
Why do they trust us and choose the CELT clinic?
- CELT surgeons were among the first in the Soviet Union to begin performing laparoscopic gallbladder removal operations in 1991 in Moscow.
- CELT has accumulated experience in the treatment of complicated and acute forms of cholecystitis, and has developed methods for eliminating various complications and postoperative treatment tactics.
- Over 25 years of work, the permanent surgical team has successfully performed more than 15,000 endoscopic operations.
- Over the past 20 years, there has not been a single case of conversion (transition from laparoscopic to abdominal surgery in complex cases). Global statistics – 3-8%.
- Comfortable stay without pain during surgery and in the postoperative period.
- About 75% come to us for gallbladder removal surgery on the recommendation of their friends or relatives
Possible complications
Cholecystectomy, like any surgical intervention, is accompanied by the risk of certain complications:
- Bile leakage is a condition where bile is released from the drainage tube. Often it is not dangerous and stops on its own as soon as the tissue in the area of the gallbladder bed heals. At the same time, the length of hospitalization increases slightly. But sometimes bile leakage indicates a serious complication - damage to the bile ducts. This requires repeated surgery.
- Bleeding.
- Infectious complications.
- Damage to the liver, intestines.
- Thromboembolism is a condition in which a blood clot forms in the veins, usually of the lower extremities, from which a fragment can then break off. It is able to migrate with the bloodstream into other vessels and cause their blockage. For example, this is how a life-threatening complication develops - pulmonary embolism.
- Reactions to anesthetic drugs.
- Pneumonia is inflammation of the lungs. This complication can be caused by general anesthesia and the entry of stomach contents into the respiratory tract.
- Exacerbation of peptic ulcer of the stomach and duodenum.
In most cases, there are no long-term digestive problems after gallbladder removal. This organ does not play a critical role. In some patients, the stool becomes liquid, but over time it returns to normal.
In 5–40% of cases, the so-called postcholecystectomy syndrome develops. The nature of this condition is not completely clear. There are suggestions that it is a continuation of the disease, due to which the bile ducts had to be removed. It is also possible that this is a consequence of the operation itself. Postcholecystectomy syndrome manifests itself in the form of periodic aching pain in the right hypochondrium, nausea, belching, bloating, loose stools, and decreased appetite. Treatment of this condition is medicinal: painkillers, enzymes, drugs that suppress secretion in the stomach.
In most cases, cholecystectomy is not particularly difficult for a surgeon with appropriate experience. Leading doctors work at the Medica24 international clinic and perform interventions in an operating room equipped with the latest laparoscopic equipment. This allows you to achieve excellent results from surgical treatment, minimize risks for the patient and shorten the recovery period.
The material was prepared by oncologist, thoraco-abdominal surgeon, head of the department of surgery at the international clinic Medica24, Alexander Valerievich Korotaev.
To do or not to have surgery?
Gallstone disease is life-threatening due to its complications, which can develop very quickly - in a matter of hours. These complications can be extremely severe and incurable. There are no reliable drug methods for treating cholelithiasis and preventing its complications.
In most cases, cholelithiasis requires surgery.
It is necessary even if pain has never bothered the patient. The first attack of cholecystitis can lead to serious complications.










