Rhesus conflict
Rh conflict: how to save the life of an unborn child
15% of people have negative Rh blood. This genetic feature is not dangerous. But during pregnancy, a Rh-negative expectant mother needs a monthly examination for Rh-conflict.
Rh conflict, Rh factor, pregnancy
When visiting a doctor to confirm pregnancy, a woman undergoes a series of tests, among which the determination of the Rh factor is mandatory. There will be no cause for concern if it is positive, as well as in the case of negative Rh blood in both future parents.
History of the Discovery of the Rh Factor In 1940, doctors Karl Landsteiner and Alexander Wiener published information about the Rh antigen, also called the Rh factor.
Scientists were able to obtain blood serum that interacted with approximately 85% of various human red blood cells. The substance was obtained by immunizing rabbits with red blood cells from rhesus monkeys (Macacus rhesus) and was called Rh factor.
Incompatibility problem
The Rh factor is checked using a blood test. “Rh−” poses a threat to the mother in labor if her Rh does not coincide with the baby’s Rh. Research has shown that some problems are related to blood type incompatibility between mother and fetus or between parents. As written above, markers (antigens) protect the body from external pests such as bacteria and viruses. When an antigen encounters a foreign object, it creates antibodies against it. The same thing can happen when trying to get pregnant. The body will react by producing antibodies to the appearance of sperm or a fetus, which will prevent conception.
Many migraine medications help manage the symptoms but do not cure the pathology. Triptans are a group of medications that are intended specifically for the treatment of the disease. Read more in the article: “triptans for migraines.”

The problem appears when the Rh of the mother's blood does not match the Rh of the fetus, and the body begins to produce antibodies against proteins on the baby's red blood cells. An Rh-negative mother does not always pose a threat to fetal development:
- if both parents are Rh-negative and the child also receives “Rh−”, then no complications arise;
- if the mother has “Rh−” and the father “Rh+”, and the fetus receives Rh negative, then there is no threat of conflict;
- if the woman in labor has “Rh+” and the child has Rh negative, protein incompatibility will not occur.
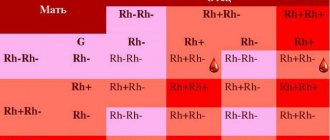
The chance of a child inheriting Rh and the probability of conflict in the table.
Rh factor
| Father | Mother | Child | Probability of conflict |
| + | + | 75% + 25% — | No |
| + | — | 50% + 50% — | 50% |
| — | + | 50% + 50% — | No |
| — | — | — | No |
Blood composition monitoring
If only the woman in a couple is a carrier of a negative Rh factor, it is important for her to have regular blood tests for Rh antibodies. Until the 32nd week of pregnancy, this must be done monthly, from the 32nd to 35th – once every 2 weeks. And from the 35th to the 40th week - weekly. Such monitoring will demonstrate how the blood composition of the expectant mother changes. And if the number of antibodies in it begins to increase, it is necessary to take emergency measures to save the life of the unborn child.
In addition to the Rh factor, another conflict may develop if the blood of the expectant mother and child are incompatible by blood group. Group incompatibility develops if the mother has the first blood group - 0 (I), and the child has the second A (II) or the third B (III).
What are the consequences for mother and child?
For a pregnant woman, the development of a serological conflict does not threaten her in any way and does not affect her health in any way, which cannot be said about a child. A serological conflict can cause severe hemolytic disease (erythroblastosis fetalis), brain damage, hypoxia, and damage the central nervous system, liver and kidneys. For this reason, such a pregnancy requires careful medical monitoring.
Does blood group compatibility affect conception and gender of a child?
When planning a child, parents need to know their own blood type and Rh factor. This is important information that can affect both the course of pregnancy and the health of the unborn child.
Is blood group and Rh factor compatibility so important? The blood type itself (if you do not take into account the Rh factor) does not in any way affect the process of conception, the course of pregnancy or the gender of the child. In the practice of any reproductive specialist, there is more than one case where parents with different blood groups became parents of a healthy child.
Ideally, the Rh factor of both parents should match, otherwise there is a high risk of developing a serological conflict, when the mother’s body rejects the fetus as a foreign body.
Risk of Rh conflict for the unborn child
The appearance of antibodies in the blood of a pregnant woman is a signal that positively charged fetal blood cells have entered it. Thus, the mother’s body begins to get rid of the “foreign body” - her own child. Rh antibodies destroy the baby's red blood cells. Protecting themselves and replenishing them, the baby’s liver and spleen begin to intensively produce red blood cells and, as a result of active work, grow in size. The amount of bilirubin in the blood of the unborn baby increases, causing oxygen starvation. After detecting antibodies to the Rh factor in the blood of the expectant mother, doctors should monitor the development of the fetus using ultrasound and pay special attention to the size of its liver and spleen.
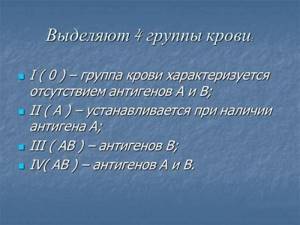
AB0 system
This system for the typology of blood groups began to be used in 1900, when the presence in the blood (on red blood cells) of antigens, which were called agglutinogens, as well as antibodies to them, which began to be called agglutinins, was discovered. Agglutinogens are A and B, and agglutinins are designated alpha and beta. Possible combinations of such proteins create 4 groups:
- 0 (first) – contains alpha agglutinin and beta agglutinin.
- A (second) - contains beta agglutinin and A agglutinogen.
- B (third) - contains alpha agglutinin and B agglutinogen.
- AB (fourth) – contains A agglutinogen and B agglutinogen.
- Which blood type suits everyone: transfusion compatibility, Rh factor
Changing the Rh factor: pros and cons
Opinion “against” The Rh factor refers to the innate properties of human blood, is inherited and does not change throughout life.
Opinion “for” In 12% of cases, there is a risk of a change in the Rh factor from negative to positive and vice versa. But the blood type remains the same.
Proponents of the version of changing the Rh factor argue it with a unique case when a 9-year-old girl, after a liver transplant, changed from group I blood with a negative Rh factor to group I blood with a positive Rh factor. Tests revealed that blood stem cells from the donor’s healthy liver penetrated the girl’s bone marrow and affected the functioning of the immune system. Doctors believe that the patient’s youth and a low number of leukocytes are possible reasons for this change in the body.
If mom and dad's blood types are different
With a different group of parents, there will be even more options for passing on genes.
| Mom's blood type | Father's blood type | Child's blood type |
| First (00) | Second (AA) | Second (A0) |
| First (00) | Second (A0) | First (00) or second (A0) |
| First (00) | Third (BB) | Third (B0) |
| First (00) | Third (B0) | First (00) or third (B0) |
| First (00) | Fourth (AB) | Second (A0) or third (B0) |
| Second (AA) | First (00) | Second (A0) |
| Second (AA) | Third (BB) | Fourth (AB) |
| Second (AA) | Third (B0) | Second (A0) or fourth (AB) |
| Second (AA) | Fourth (AB) | Second (AA) or fourth (AB) |
| Second (A0) | First (00) | First (00) or second (A0) |
| Second (A0) | Third (BB) | Third (B0) or fourth (AB) |
| Second (A0) | Third (B0) | First (00), second (A0), third (B0) or fourth (AB) |
| Second (A0) | Fourth (AB) | Second (AA or A0), third (B0) or fourth (AB) |
| Third (BB) | First (00) | Third (B0) |
| Third (BB) | Second (AA) | Fourth (AB) |
| Third (BB) | Second (A0) | Third (B0) or fourth (AB) |
| Third (BB) | Fourth (AB) | Third (BB) or fourth (AB) |
| Third (B0) | First (00) | First (00) or third (B0) |
| Third (B0) | Second (AA) | Second (A0) or fourth (AB) |
| Third (B0) | Second (A0) | First (00), second (A0), third (B0) or fourth (AB) |
| Third (B0) | Fourth (AB) | Second (A0), third (BB or B0) or fourth (AB) |
| Fourth (AB) | First (00) | Second (A0) or third (B0) |
| Fourth (AB) | Second (AA) | Second (AA) or fourth (AB) |
| Fourth (AB) | Second (A0) | Second (AA or A0), third (B0) or fourth (AB) |
| Fourth (AB) | Third (BB) | Third (BB) or fourth (AB) |
| Fourth (AB) | Third (B0) | Second (A0), third (BB or B0) or fourth (AB) |
Treatment and prevention of Rh conflict
If antibodies to the Rh factor are detected in the blood of a pregnant woman, an injection of anti-Rhesus immunoglobulin is recommended. When it enters the bloodstream, this drug binds antibodies and removes them. To prevent the occurrence of Rh conflict, it is recommended to receive the first vaccination with anti-Rhesus immunoglobulin at the 28th week of pregnancy. The second, also the final, is done within 72 hours after birth. However, if the monthly blood test does not show the appearance of Rh antibodies, you can postpone vaccination until after delivery. In the case of the birth of a child with positive Rh, the expectant mother is required to receive an injection of immunoglobulin. On the negative side, there is no need for it.
Detection of the fetal RHD gene in the mother's blood. Fetal Rh factor
A genetic marker used to determine the Rh factor of the fetus from fetal DNA. The analysis is performed only from the 10th week of pregnancy if the pregnant woman has a negative Rh factor.
Synonyms Russian
Detection of the presence/absence of the 7th and 10th exons of the RHD gene; genotyping of the RHD gene using fetal DNA.
English synonyms
Fetal RHD genotyping test.
Research method
Real-time polymerase chain reaction.
What biomaterial can be used for research?
Venous blood of a pregnant woman with serological negative Rh factor from the 10th week of pregnancy.
How to properly prepare for research?
No special preparation is required.
General information about the study
From the point of view of immunology, pregnancy throughout its entire duration is considered as a process of changing staged immune conflicts. Basically, these conflicts are normal physiological processes and not only do not have a pathological effect on the body of the mother and fetus, but also help the normal course of pregnancy. With their help, such stages of pregnancy as fetal implantation, the formation of the hormonal background of pregnancy and, of course, the birth itself are realized. In addition, there are a number of pathological conflicts that can significantly complicate the course of a normal pregnancy, sometimes leading to death. One of them is Rh conflict between mother and fetus.
The Rh (Rh) system is one of the most polymorphic and immunogenic systems known in humans; it is represented by a group of protein molecules located on the surface membrane of red blood cells. The most studied proteins (antigens) of this group are antigens D, C, c, E and e, which are encoded by the RHD and RHCE genes located on chromosome 1. The presence of the RHD gene in the genome leads to the appearance of antigen D on erythrocytes, which corresponds to Rh positive phenotype (Rh+). The Rh negative phenotype (Rh-) is formed as a result of the absence of both homologous alleles of the RHD gene.
The most important factor in the occurrence of Rh conflict during pregnancy is the formation of an Rh-positive fetus in an Rh-negative mother. Although the bloodstream of the fetus and mother are separated by the placenta, cell fragments and DNA from the fetus (fetal DNA) can pass through it. The permeability of the placenta can increase due to a number of pathological processes: gestosis, diseases of the uterus, taking medications, somatic pathology, etc. When fetal D antigens enter the mother's blood, they produce Rh antibodies (RhAb). They are harmless to the mother, but, passing back through the placenta, they initiate the development of hemolytic disease of the fetus and newborn by binding to fetal red blood cells and their subsequent destruction. Such conditions are a risk factor for perinatal mortality, highlighting the need for early diagnostic and preventive therapeutic strategies to preserve fetal viability.
Currently, there are two main methods for determining the Rh factor. The first method, serological, involves the detection of antigen D on the surface of red blood cells using specific antibodies. It is suitable for wide routine examination. Significant limitations of this method include: 1) the need to have live red blood cells for testing, which makes it impossible to use it in the prenatal diagnosis of fetal Rh factor; 2) the presence of a mutation within the RHD gene or a change in its expression level. In these cases, serological testing may give a false negative result (Rh- if the RHD gene is present), since diagnostic antibodies will not be able to bind to damaged or missing D antigen molecules.
An alternative to serological testing of the Rh factor is genotyping for the presence or absence of the RHD gene. In the case of prenatal diagnosis, fetal DNA isolated from the mother's blood is used as research material. Genotyping is carried out on several fragments (7th and 10th exons) of the gene. A necessary condition that increases the specificity of this method is its use at 10 or more weeks of pregnancy in serologically Rh-negative women. The main method of genotyping in this case is the polymerase chain reaction, which detects the presence or absence of the RHD gene in the material.
Taking into account the fact that the concentration of fetal DNA in the mother’s blood is extremely low, and also taking into account the possibility of the presence of a serological false-negative Rh factor in the mother and the presence of mutations in the RHD gene, genotyping of the fetal Rh factor is carried out by examining a number of indicators: 1) presence/absence of at least two fragments (7th and 10th exons) of the RHD gene; 2) taking into account the signal from the mother’s genomic DNA.
What is the research used for?
- To predict the development of Rh conflict between a Rh-positive fetus and a Rh-negative mother.
- To resolve the issue of a strategy for the prevention of hemolytic disease of the fetus and newborn.
When is the study scheduled?
From the 10th week of pregnancy.
What do the results mean?
During the research process, four types of conclusions are formed.
1. The absence of both fragments of the RHD gene in the test material against the background of a sufficient amount of genomic DNA signal. In this case, a negative Rh factor is detected in the fetus in a Rh-negative mother. This condition does not require therapeutic correction.
2. The presence of both fragments of the RHD gene in the test material against the background of a high amount of genomic DNA signal. In this case, a positive Rh factor is detected in the fetus in a Rh-negative mother. This condition can cause Rh conflict (especially with repeated pregnancies) and requires therapeutic correction. It should be noted that the mother must be serologically confirmed to be Rh negative.
3. The presence of both fragments of the RHD gene in the test material against the background of an equal amount of genomic DNA signal. In this case, it is possible that the mother has a genetically positive Rh factor, but it is not possible to identify the fetal Rh factor.
4. The presence of a weak signal of both fragments of the RHD gene in the test material against the background of a weak signal of genomic DNA. In this case, a questionable result is stated. The presence of a weak genomic DNA signal, regardless of the signal from both fragments of the RHD gene, or the presence of one of the two fragments of the RHD gene in the test material against the background of a high amount of genomic DNA signal indicates an unreliable result. In all these cases, a repeat study is required.
What can influence the result?
- Obtaining a reliable result may be affected by the presence of a serological false-negative result in the mother (Rh- in the presence of the RHD gene) due to the presence of mutations within the RHD gene or a change in its expression level.
- The duration of the study is less than 8-10 weeks of pregnancy.
- A small amount of fetal DNA, for example with pathology of the placenta.
Important Notes
This study should be performed during every pregnancy in an Rh-negative mother.
Who orders the study?
Obstetrician-gynecologist, therapist, hematologist, acute care physician.
Literature
- Addai-Mensah O, Afriyie EY, Sakyi SA, Obirikorang C, Annani-Akollor ME, Owiredu EW, Amponsah FA, Duneeh RV, Asamoah Adu E. Fetal Rhesus D Genotyping and Sex Determination from Maternal Plasma of Rhesus D-Negative Antenatal Population: The Usefulness of Conventional Polymerase Chain Reaction in Resource-limited Settings. Obstet Gynecol Int. 2021 Oct 16;2020:4913793. doi: 10.1155/2020/4913793.
- Rather RA, Dhawan V, Saha SC. Non-invasive prenatal rhesus D genotyping using cell-free fetal DNA. Indian J Med Res. 2019 Jul;150(1):62-66. doi: 10.4103/ijmr.IJMR_1787_17.
- Arentz-Hansen H, Brurberg KG, Kvamme MK, Stoinska-Schneider A, Hofmann B, Ormstad SS, Fure B. Determination of Fetal Rhesus D Status from Maternal Plasma of Rhesus Negative Women. Oslo, Norway: Knowledge Center for the Health Services at The Norwegian Institute of Public Health (NIPH); 2014 Dec. Report from Norwegian Knowledge Center for the Health Services (NOKC) No. 25-2014.
Rh negative is not a hindrance to having a baby
Most pregnant women with negative Rh blood become mothers of healthy children. Rhesus conflict is observed in only 0.8% of expectant mothers. But even in this case, subject to regular testing for antibodies and monitoring the condition of the fetus, the risks can be minimized.
For women with negative Rh blood, an injection of immunoglobulin must be given within 72 hours both after childbirth and after cases of placental abruption, amniocetosis, spontaneous miscarriage, abortion, ectopic pregnancy and blood transfusion.
Expert: Irina Isaeva, obstetrician-gynecologist Author: Elena Nersesyan-Brytkova
The material uses photographs belonging to shutterstock.com