A hemostasiogram, or hemostasis test, is a blood test whose purpose is to identify disturbances in the functioning of the circulatory system, in particular in the process of blood clotting. The human body is designed in such a way that hemostasis maintains blood, as a substance, in a liquid state. But in case of damage to the vessels through which blood is transported, the same system triggers a mechanism to stop bleeding, which is called blood clotting.
Impaired hemostasis can lead to serious problems; this diagnosis in Yeysk is available for medical examination both with and without a doctor’s prescription.
Indications for hemostasis analysis
A bleeding disorder is primarily a serious contraindication for any surgery, so a hemostasis test is required before surgery. This diagnosis is also necessary for pregnant women, since during childbirth, a blood clotting disorder can pose a threat to the woman’s life. In addition, the doctor can prescribe this diagnosis in Yeysk for the following indications:
- Moderate to severe liver diseases: the liver is a hematopoietic organ.
- Diseases of the endocrine system: the blood clotting process is affected by the level of hormones.
- Pathologies of the cardiovascular and urinary systems.
- Autoimmune diseases.
A doctor may prescribe this type of laboratory diagnostics in cases where the patient has frequent nosebleeds, bleeding gums, bruises and hematomas even from a minor mechanical impact (minor bruise, pressure). For varicose veins, this test is also prescribed, as it allows us to identify the likelihood of a blood clot.
Physiology
Extravascular tissue, the vessel wall, plasma coagulation factors, platelets and other blood cells take part in the process of Hemostasis. An important role in G. belongs to physiologically active substances (adrenaline, norepinephrine, serotonin, etc.), local changes in ionic ratios, blood pH, and zeta potential (the potential difference between the dispersed phase and the dispersed medium, platelets and the vascular wall).
Different tissues surrounding an injured vessel have different thromboplastic activity; biol, the significance of these differences for local G. is not yet clear. As a result of the interaction of tissue and plasma factors of the blood coagulation system, active tissue thromboplastin is formed at the site of damage to the vessel wall, which is included in a chain of subsequent reactions, the final product of which is fibrin. However, tissue thromboplastin (less active than blood thromboplastin) is probably of less importance in G. when large vessels are injured. The tissues surrounding the vessel also provide mechanical resistance to the release of blood from the damaged vessel, thus influencing the amount of blood loss.
The role of the vessel wall in blood flow is determined by the presence in it of a number of factors that influence the process of blood coagulation, adhesion and aggregation of platelets; When injured, the vessel wall contracts and blood flow to the wound site decreases. The vessel wall is an efferent regulator of the rate of blood coagulation and fibrinolysis (see). The vascular intima is charged negatively in relation to the adventitia. When the vessels are damaged, the potential is reversed and the intima becomes positively charged, the zeta potential changes, which is important for the interaction of platelets with the wound surface.
Plasma blood coagulation factors in the body of a healthy person are in an inactive state. The International Committee on Blood Coagulation Factors introduced the designation of plasma procoagulants in Roman numerals; their number is thirteen (from I to XIII).
Plasma coagulation factors
Factor I - fibrinogen
Factor II - prothrombin
Factor III - thromboplastin
Factor IV - calcium
Factor V - accelerator (accelerator) of prothrombin conversion (Ac-globulin)
Factor VI - removed from the classification Factor VII - proconvertin Factor VIII - antihemophilic globulin
Factor IX is a plasma component of thromboplastin (Christmas factor)
Factor X - Stewart - Prower Factor
Factor XI - plasma precursor of thromboplastin Factor XII - contact factor (Hageman)
Factor XIII - fibrin stabilizing factor, fibrinase
Activation of the blood coagulation system occurs upon contact with a foreign surface, which is the trigger of the internal hemostasis system (active blood coagulation factors are indicated by adding the letter “a” to the corresponding Roman numeral). G. ends with the formation of a blood clot at the site of damage to the vessel wall.
The participation of platelets in blood clotting is due to their properties such as adhesion and aggregation, the content of their own and adsorbed blood coagulation factors, as well as physiologically active substances.
The role of erythrocytes and leukocytes in blood flow is determined by the content of the majority of blood clotting factors in them. When the vascular wall is damaged, these factors are included in the fibrin formation reaction. During blood clotting, red blood cells are retained in the fibrin network, promoting the formation of a blood clot and an increase in its mass.
The process of Hemostasis has neurohumoral regulation: extreme factors cause an increase in the tone of the sympathetic department. n. pp., increase the flow of adrenaline and norepinephrine into the blood, which accelerates the adhesion and aggregation of platelets and activates the blood coagulation process as a whole. The spread of thrombus formation along the vascular bed is prevented by circulating anticoagulants, fibrinolytic agents and inhibitors of platelet adhesion and aggregation - adenosine and adenosine monophosphate, which are formed during the breakdown of ADP.
Depending on the size of the damaged vessel and the role of individual factors in limiting blood loss, two main mechanisms of blood loss are distinguished: vascular-platelet (or microcirculatory) and coagulation. In the first, the leading role in stopping bleeding is assigned to the vascular wall and platelets (see), in the second - to the blood coagulation system (see Blood coagulation system). In addition, DIC syndrome (disseminated intravascular coagulation) may occur.
Scheme 1. Vascular-platelet mechanism of hemostasis.
Vascular-platelet mechanism
(Scheme 1) occurs when bleeding from small vessels is stopped: arterioles, precapillaries, capillaries and venules. It consists of the following stages: 1) short-term vascular spasm, 2) adhesion of platelets to the wound surface, 3) accumulation and aggregation of platelets at the site of injury, 4) viscous metamorphosis and platelet release reaction, 5) secondary vasospasm, 6) formation of fibrin and fiziol, hemostatic thrombus (see).
Under the influence of injury, the tone of the sympathetic department increases. n. With. and local vasospasm occurs, reducing blood flow. Vasoconstriction is also facilitated by the reflex release of adrenaline into the bloodstream and the release of cholinesterase, which blocks acetylcholine. Platelets adhere to damaged endothelial cells and tissue fibers of the vascular wall on the wound surface: the formation of a hemostatic platelet thrombus begins.
The main structures of the vascular wall with which platelets interact are collagen fibers, microfibrils and basement membrane. The adhesion of platelets to collagen fibers is apparently not associated with the process of blood coagulation, since when the blood is completely incoagulable (for example, as a result of heparinization), it is not disturbed. Thrombin does not cause platelet adhesion, but enhances it, promoting the release of ADP from platelets. In the mechanism of interaction of platelets with the damaged vessel wall in the process of G., electrostatic forces that enhance the adhesion of platelets to the wound surface are probably important. Slowing blood flow and blood movement contribute to the interaction of platelets with the damaged vessel wall.
Following adhesion, platelet aggregation occurs at the site of injury to the vessel wall. ATP is released from damaged endothelial cells, as well as from erythrocytes and platelets, which is converted into ADP under the action of cellular adenosine triphosphatase. Under the influence of the latter, platelet aggregation occurs (reversible); The effect of ADP on platelets is manifested in the presence of calcium ions and a plasma cofactor in the medium - von Willebrand factor, factor XIII (fibrin-stabilizing factor) or factor I (fibrinogen). A number of hypotheses have been proposed to explain the mechanism of platelet aggregation; The most widely recognized hypothesis is that of Gaarder and Laland (A. Gaarder, J. Laland), who believe that the platelet-aggregating activity of ADP is due to three free negative valences: two valences bind one calcium ion, and the third, together with the same valency of the neighboring ADP molecule, attaches another calcium ion; platelet aggregation occurs as a result of the formation of calcium “bridges” between platelet-nucleotide complexes.
Platelets that aggregate at the wound surface undergo viscous metamorphosis under the influence of thrombin. During the process of viscous metamorphosis, blood clotting factors, serotonin, histamine, adrenaline, kinins, nucleotides, and enzymes are released from platelets; platelet aggregation Becomes irreversible. The release of these factors from platelets promotes secondary narrowing of the damaged vessel. In parallel, the reaction of fibrin formation occurs. Fibrin fibers and subsequent retraction of the blood clot compact the hemostatic thrombus, which leads to the final cessation of bleeding.
Scheme 2. Coagulation mechanism of hemostasis.
Coagulation mechanism
(Scheme 2) occurs with injury to large arteries and veins following the limitation of blood loss as a result of vascular spasm, especially of the muscular type. However, in this case, platelets are the first to attach to the site of damage to the vessel wall. At the same time, the blood coagulation system is activated as a result of the complex interaction of plasma and cellular procoagulants, which occurs as a proenzyme-enzyme cascade transformation, and fibrin is formed. Blood cells are drawn into the fibrin network, a blood clot is formed, which reduces or completely prevents blood loss). The final stage is retraction of the blood clot, which lasts several hours. As a result of retraction, the hemostatic thrombus becomes more reliable. In this case, serum rich in thrombin is released from the clot.
Disseminated intravascular coagulation (DIC) is a syndrome that can occur in various pathological conditions (acute hemolysis, infectious processes, intoxication, antigen-antibody reaction, etc.). Both vascular-platelet and coagulation factors take part in its development.
Impaired hemostasis due to defects in individual components of its system - see table.
Hemostasis test for pregnant women
The threat of large blood loss during childbirth is the main criterion that guides the obstetrician-gynecologist when prescribing a hemostasis test for a pregnant woman. However, in addition to this, a hemostasiogram can be prescribed by the doctor monitoring the course of pregnancy in the case when the patient develops gestosis or has uterine hypertonicity, there is a threat of miscarriage, or there is a delay in intrauterine development of the child. A hemostasis test is usually prescribed even if the pregnancy is multiple. When observed by an obstetrician-gynecologist in a medical clinic, a woman undergoes all necessary examinations during pregnancy.
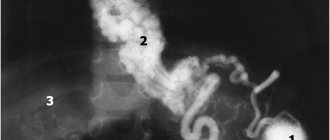
Research methods
G.'s condition is identified by coagulogram indicators (see), as well as on the basis of tests that determine: the state of resistance of the vascular wall, bleeding time (see), both primary and secondary, the volume of blood lost, aspirin tolerance, the strength of early fixation platelet plugs in vessels, the number of platelets, their functional activity (ability for adhesion in vitro and in vivo, ADP-, collagen- and thrombin-aggregation).
The principle of restoring hemostasis is to strengthen the vessel wall, increase the adhesive and aggregation ability of platelets, and restore lost or reduced blood clotting ability.
The main principle of the medicinal method of stopping bleeding is the differentiated use of hemostatic agents, taking into account the mechanism of bleeding development. Therefore, before starting antihemorrhagic therapy, it is necessary to conduct a thorough laboratory study of the functional state of the blood coagulation system in order to identify the main cause of impaired hemostasis.
Conventional and advanced hemostasis analysis
This diagnostics in Yeysk can be carried out at the Sensitive LCC both according to the regular program and in an expanded form. The standard hemostasiogram includes the following indicators:
- thrombin and prothrombin time;
- prothrombin level;
- fibrinogen level;
- platelet count in peripheral blood;
- soluble complexes of monomers and fibrin.
An advanced analysis for hemostasis adds to the above indicators the study of such parameters as:
- antithrombin III,
- lupus anticoagulant and D-dimer,
- von Willebrand factor.
Standard and extended screening of the hemostatic system
The most commonly ordered is the standard test, which includes basic blood clotting assessment tests.
As a rule, a basic hemostasiogram (or coagulogram) includes:
- fibrinogen is a key test of the state of the coagulation system;
- prothrombin - changes in the level of this protein in the blood determine the condition of the liver and gastrointestinal tract;
- platelets - blood cells involved in the regulation of hemostasis;
- prothrombin index (PTI), prothrombin time (PTT), international normalized ratio (INR) - tests that reflect the external pathway of blood coagulation;
- activated partial thromboplastin time (aPTT) - a test that reflects the work of the internal coagulation pathway, the time required for the formation of a blood clot;
- thrombin time is the period required for inactive fibrinogen to convert into fibrin.
However, many conditions require extensive research. In essence, an extended hemostasiogram is the same test, but in addition to the basic parameters indicated above, it includes such important indicators as:
- antithrombin III and protein C are factors of the anticoagulation system; their insufficient level indicates a risk of blood clots;
- D-dimer is an element of the blood clot resorption system; high values may indicate kidney pathology, diabetes mellitus, and gestosis;
- lupus anticoagulant - an indicator that allows you to confirm or refute the fact that a patient has systemic lupus erythematosus or another autoimmune pathology;
- plasma tolerance to heparin is a parameter indicating coagulation function; an elevated level may indicate problems in the liver, heart failure, prethrombosis, etc.;
- soluble fibrin-monomer complexes (SFMC) - products of dissolution of a blood clot during fibrinolysis; an increase in their level may indicate connective tissue pathology, sepsis, thromboembolism;
- plasma recalcification time is an indicator of the formation of a fibrin protein clot; this parameter reflects the coagulation process as a whole;
- activated recalcification time (AVR) is the period required for the formation of fibrin; a shortened time indicates the tendency of the subject’s body to form blood clots, an extended time indicates increased bleeding.
Preparing for hemostasis analysis
The described diagnosis in Yeysk requires some preparation. Blood is given for analysis in a medical clinic on an empty stomach. In addition, it is recommended not to eat food 8-12 hours before blood sampling; during this time you can drink clean, still water. On the eve of donating blood, you should avoid physical activity, stress, alcohol and medications that affect hematopoiesis. This primarily applies to aspirin and similar drugs, which should be stopped taking at least 5 days before the hemostasis test.
Examination of temporary disability in LKK "Sensitive"
Medical certificate for entry into civil service
New rules for a medical certificate for weapons
Why enter into a voluntary health insurance agreement?
Certificates for service at LKK Sensitive
Medical certificate to carry a weapon
Voluntary health insurance agreement
Medical examination in Yeysk