Classification
Leukocytoses are divided according to various criteria. According to their biological significance, physiological and pathological increases in leukocytes in the blood are distinguished. Physiological leukocytosis does not cause any harm and is observed in every healthy person under certain circumstances - during intense muscular work (myogenic), 2-3 hours after eating (alimentary), in the second trimester of pregnancy (gestational). Pathological leukocytosis is caused by diseases. According to the degree of increase in the level of leukocytes, they are distinguished:
- Moderate leukocytosis
. The number of leukocytes is from 9000 to 15000. - High leukocytosis
. The content of leukocytes is from 15,000 to 50,000. - Hyperleukocytosis (leukemoid reaction)
. White blood cell concentration greater than 50,000. Large numbers of immature forms of white blood cells are often present.
In addition to the level of leukocytosis, it is important what type of leukocytes is beyond the normal range. Depending on the type of leukocytes, the following types of leukocytosis are distinguished:
- Neutrophilic (neutrophilia)
. Increase in neutrophils above 75%. The cause is bacterial infections and suppurative processes. - Lymphocytic (lymphocytosis)
. The content of lymphocytes is more than 38% (in children under 7 years of age - above 55%). Common causes are viral infections and lymphoproliferative diseases. - Monocytic (monocytosis)
. Increase in monocytes above 10%. The causes are granulomatous processes, protozoal infections, and septic endocarditis. - Eosinophilic (eosinophilia)
. The content of eosinophils is more than 5%. The main causes are helminthic infestations, allergic reactions, and some lung diseases. - Basophilic (basophilia)
. Increase in basophils above 1%. A very rare condition. The causes are allergies, polycythemia vera, and ulcerative colitis.
Increased leukocytes, signs
It is important to remember that leukocytosis is not a disease or syndrome; it is a consequence rather than a cause. Therefore, it is difficult to identify any clear symptoms. However, an increased white blood cell count usually manifests itself with the following characteristic signs:
- increase in body temperature to subfebrile levels (38 - 38.5 degrees);
- increased sweating, especially at night;
- symptoms of general malaise - weakness, dizziness, asthenia, loss of strength;
- intestinal spasms;
- aching muscle and joint pain of weak to moderate intensity
Thus, you should correctly understand the concept of leukocytosis and not sound the alarm if blood tests show an increase in leukocytes. After all, this may be an absolutely normal reaction of the body to one or another irritant, a sign of normal functioning of the immune system.
Leukocytosis is not a disease. This is simply a sign that the body is adapting to new conditions. However, such test results should not be neglected; the cause of fluctuations in blood cells in the plasma should be clarified by specialized specialists.
Causes of leukocytosis
Infections
The most common cause of leukocytosis is considered to be various infections (bacterial, viral, parasitic). Since the main function of all leukocytes is to maintain anti-infective immunity, the presence of a foreign pathogen in the body is accompanied by a reactive increase in white blood cells in the blood. Moreover, a certain type of microorganism causes various types of leukocytosis.
- Bacterial infections
. During bacterial infections, the content of neutrophils and monocytes in the blood increases, which destroy pathogens through phagocytosis and an “oxygen explosion.” In localized infections (angina, pyelonephritis, bronchitis), leukocytosis is usually insignificant. Severe purulent processes (abscess, phlegmon, osteomyelitis) and generalized infections (sepsis, endocarditis) are characterized by high leukocytosis, and sometimes a leukemoid reaction occurs. A distinctive feature of leukocytosis, the cause of which was a bacterial infection, is a shift in the leukocyte formula to the left, i.e. the appearance in the blood of “young”, immature forms of neutrophils (metamyelocytes, promyelocytes). In acute processes, leukocytosis increases sharply and reaches a maximum on days 1-2 of the disease, then gradually decreases and returns to normal. In chronic bacterial infections, the white blood cell count may be at or slightly above the upper limit of normal. - Viral infections
(flu, measles, mononucleosis). They cause an increase in lymphocytes in the blood, which have the ability to trigger the apoptosis mechanism in viral cells and produce specific antibodies (immunoglobulins) against them. Lymphocytosis is most often moderate and can persist for a long time (weeks, months, years), especially with persistent viral infections (cytomegalovirus, Epstein-Barr virus). - Helminthic infestations.
Infection with helminths (roundworms, pinworms, hookworms) is considered one of the most common causes of eosinophilic leukocytosis. Eosinophils contain in their granules eosinophilic cationic protein, which disrupts metabolic processes in the body of helminths. Eosinophilia occurs approximately on the 5th day of illness, grows rapidly and reaches very high values by 35-40 days, and then begins to slowly (over several weeks) decrease to normal numbers.
Systemic diseases
Leukocytosis is often caused by chronic systemic inflammatory processes. The exact pathogenetic mechanisms of the increase in leukocytes in these pathologies are still unknown. It is assumed that mediators and cytokines produced during rheumatic inflammation stimulate the production of leukocytes in the bone marrow. This mainly concerns the following rheumatic diseases:
- Joint diseases
: rheumatoid arthritis, ankylosing spondylitis. - Diffuse connective tissue diseases
: systemic lupus erythematosus, dermatomyositis, scleroderma. - Systemic vasculitis:
nonspecific aortoarteritis, granulomatosis with polyangiitis, giant cell arteritis.
In arthritis and diffuse connective tissue diseases, leukocytosis is usually moderate. In systemic vasculitis with necrotizing inflammation in the vascular wall, leukocytosis can reach high numbers.
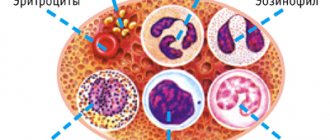
What are leukocytes
Several types of formed elements float in the blood, which support the health of the whole organism. White cells that have a nucleus inside are called leukocytes. Their peculiarity is the ability to penetrate the capillary wall and enter the intercellular space. It is there that they find foreign particles and absorb them, normalizing the vital activity of the cells of the human body.

Leukocytes include several types of cells that differ slightly in origin and appearance. The most popular division is based on morphological characteristics.
| Morphology | View | Normal quantity |
| Granular (having granules in the cytoplasm) | Neutrophils | 70% |
| Eosinophils | 1-5% | |
| Basophils | Up to 1% | |
| Non-granular (no granules) | Lymphocytes | 21-35% |
| Monocytes | 4-8% |
The ratio of these cells is the same in all healthy people and is expressed by the leukocyte formula. By changing the number of any type of cells, doctors draw conclusions about the nature of the pathological process.
You need to know the symptoms of high blood pressure in women in order to provide timely help. Correctly provided first aid for a hypertensive crisis can save a person’s life. Read more in the article: “causes of high blood pressure in women.”
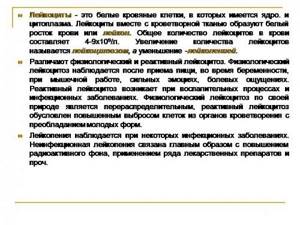
It is leukocytes that maintain human health at the proper level. Most infections that enter the human body are asymptomatic due to a timely immune response.
Allergy
This is the main cause of eosinophilic leukocytosis. Entry of an allergen into the body causes IgE-mediated degranulation of mast cells with the release of mediators of allergic inflammation - leukotrienes, histamine, etc. One of the main functions of eosinophils is to suppress the production of inflammatory mediators, therefore any allergic reaction is accompanied by an increase in the level of eosinophils.
The maximum level of eosinophilia is achieved at the time of exacerbation of the allergic reaction, then it gradually decreases as symptoms regress and returns to normal levels during the remission stage. In most allergic diseases (bronchial asthma, rhinoconjunctivitis), moderate leukocytosis is observed. Only with the development of systemic reactions (Stevens-Jones syndrome, DRESS syndrome) can high leukocytosis occur.
Blood diseases
Malignant myeloproliferative (leukemia, polycythemia) and lymphoproliferative (lymphoma) pathologies are considered the main cause of hyperleukocytosis. It is caused by oncological transformation of bone marrow and lymphatic tissue stem cells with subsequent hyperproduction of leukocytes. With leukemia, neutrophilic, monocytic or eosinophilic leukocytosis is observed, with lymphomas - lymphocytosis.
In acute leukemia, in addition to leukocytosis, signs such as leukemic failure are noted, which implies the presence of only mature leukocytes and blast cells and the absence of intermediate forms (metamyelocytes), basophilic-eosinophilic association (simultaneous sharp increase in basophils and eosinophils). Leukocytosis increases slowly over several years. Reaches high numbers (up to 100,000) and gradually decreases under the influence of chemotherapy.
Other reasons
- Massive tissue breakdown
: myocardial infarction, ischemic stroke, pancreatic necrosis, extensive burns. - Toxic effects on the bone marrow
: poisoning with lead, organic hydrocarbon compounds, ionizing radiation. - Endocrine disorders
: chronic adrenal insufficiency, autoimmune polyglandular syndromes, congenital dysfunction of the adrenal cortex. - Primary immunodeficiencies
: Wiskott-Aldrich syndrome, Jobe syndrome (hyper-IgE syndrome). - Malignant neoplasms
: small cell lung cancer, breast cancer, colon adenocarcinoma. - Lung diseases
: pulmonary eosinophilia (eosinophilic pneumonia), Langerhans cell histiocytosis, allergic bronchopulmonary aspergillosis. - Dermatological diseases
: eczema, Dühring's dermatitis herpetiformis, scabies. - Condition after removal of the spleen (splenectomy)
: as a component of post-splenectomy syndrome.
Diagnostics
Leukocytosis is detected during a clinical blood test. Since there are many reasons for an increase in white blood cell levels, you should first consult a general practitioner. The doctor collects a detailed medical history, conducts a physical examination of the patient, including measuring body temperature, examining the skin and mucous membranes, etc. Based on the data obtained, in order to confirm the disease that caused leukocytosis, the following studies are prescribed:
- Blood tests
. Markers of inflammation are determined in the blood - high ESR and CRP, autoantibodies (rheumatoid factor, ACCP, antibodies to the cytoplasm of neutrophils). The leukocyte formula (percentage of leukocyte forms) must be calculated. A blood smear is examined for the presence of toxic granularity of neutrophils, atypical mononuclear cells, and Botkin-Gumprecht shadows. If a septic condition is suspected, presepsin is measured. - Pathogen detection
. To identify the infectious pathogen as the cause of leukocytosis, bacterial culture of blood, sputum, and urine is performed. The enzyme immunoassay method detects antibodies (class and immunoglobulins) to bacteria, viruses, helminths, and their DNA is detected using the polymerase chain reaction. - Allergy diagnostics
. In order to confirm the allergic nature of the disease, the level of immunoglobulin E (IgE) is measured using the ELISA method. To identify the causative allergen, basophil tests and various allergological tests are performed - skin (scarification, patch, prick tests), provocative (nasal, inhalation, conjunctival). - Radiography
. In case of pneumonia, chest x-rays show infiltrates in the lungs, foci of darkening; x-rays of joints in patients with arthritis show narrowing of the joint space, osteoporosis, and bone erosion. With osteomyelitis, x-rays of bones reveal thickening of the periosteum and sequestration foci (areas of bone necrosis). - Ultrasound
. With pyelonephritis, an ultrasound examination of the kidney reveals an increase in the size of the kidneys, expansion and thickening of the pyelocaliceal system. Infectious mononucleosis is characterized by hepatosplenomegaly. Echocardiography may show vegetations on the valves and effusion into the pericardial cavity. - Histological studies
. If leukemia is suspected, a trephine biopsy or sternal puncture is performed, the material of which reveals hyperplasia of the granulocytic lineage and a large number of blast cells. To diagnose lymphomas, an aspiration biopsy of an enlarged lymph node is performed; the biopsy specimen reveals lymphocytic hypercellularity, collagen proliferation, and Berezovsky-Sternberg giant cells.

The leukocyte formula allows you to determine the percentage of different types of leukocytes
Functions of leukocytes
The importance of leukocytes is explained by their participation in the immune response and protecting the body from any foreign agents. The main functions of white cells are as follows:
- Antibody production.
- Absorption of foreign particles – phagocytosis.
- Destruction and removal of toxins.
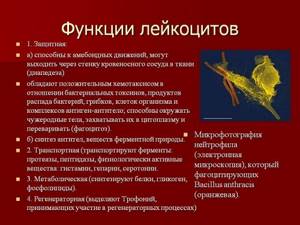
Each type of leukocyte is responsible for certain processes that help in carrying out the main functions:
- Eosinophils
. They are considered the main agents for the destruction of allergens. They participate in the neutralization of many foreign components that have a protein structure. - Basophils
. They accelerate the healing process at the site of inflammation, due to the presence of heparin in its structure. Updated every 12 hours. - Neutrophils
. Participate directly in phagocytosis. Capable of penetrating into the intercellular fluid and into the cell where the microbe lives. One such immune cell can digest up to 20 bacteria. Fighting microbes, the neutrophil dies. Acute inflammation provokes a sharp production of such cells by the body, which is immediately reflected in the leukocyte formula as an increased number. - Monocytes
. Helps neutrophils. They are more active if an acidic environment develops at the site of inflammation. - Lymphocytes
. They distinguish their own cells from foreign cells by their structure and participate in the production of antibodies. They live for several years. They are the most important component of immune defense.

Many doctors require you to do a clinical blood test before prescribing treatment. Viral and bacterial diseases cause different changes in the analysis, which makes it possible to make the correct diagnosis and prescribe the necessary medications.
Gonorrhea is an infectious disease that is transmitted during sexual intercourse. Gonorrhea is always unpleasant and should be treated only after a complete diagnosis. Read more in the article: “treatment of gonorrhea with one tablet.”
Treatment for leukocytosis
There is no symptomatic treatment for leukocytosis. To normalize the level of white blood cells, it is necessary to combat the underlying pathology that caused leukocytosis. With minor leukocytosis during the period of recovery from an infectious disease, no medical intervention is needed. However, even a moderate increase in leukocytes in the blood that persists for a long time requires consultation with a specialist to determine the cause.
Antibacterial, antiviral, and anthelmintic drugs are used to treat diseases accompanied by leukocytosis. If the high level of leukocytes is due to rheumatological pathology, drugs that suppress the inflammatory process (glucocorticosteroids, immunosuppressants) are used. Allergic reactions are effectively treated with antihistamines and corticosteroids.
If the cause of leukocytosis is malignant hematological diseases, a long course of chemotherapy is required, and in some cases, allogeneic bone marrow transplantation. Suppurative processes (phlegmons, abscesses) are subject to surgical intervention, which involves dissection of soft tissue, washing and draining of the lesion. Endocarditis may require valve surgery or replacement.
Leukocytes in the blood are low
If leukocytes are elevated, it means there is an inflammatory process in the body, or a fight against infection, but the body fights on its own and often copes with the task, but what do low leukocytes signal? About a decrease in a person’s immunity, about a deterioration in the body’s ability to resist various diseases.
A reduced level of white blood cells indicates problems in the hematopoietic system, namely in the bone marrow, which produces blood cells. Chemotherapy for cancer, as well as taking interferon-based drugs, can cause a decrease in the number of indicators. but lower results do not always indicate the presence of a serious disease. Sometimes the reason can be simple - poor nutrition and a significant lack of certain vitamins: B vitamins, copper, iron and folic acid.
Severely low white blood cells can be a sign of a disease such as AIDS. This deviation should serve as a reason for conducting a more in-depth analysis of the health status.
Forecast
Leukocytosis in itself cannot be a predictor of consequences or complications. It is impossible to predict the prognosis and risk of death. The outcome directly depends on the cause, i.e. the disease that caused leukocytosis, as well as the degree of its severity. For example, an acute respiratory viral infection almost always proceeds benignly, ends with complete recovery and does not in any way affect life expectancy. Pathologies such as systemic vasculitis and hemoblastosis are characterized by a high mortality rate. Therefore, at any level of increase in leukocytes in the blood, a thorough examination aimed at identifying the cause and timely initiation of treatment is indicated.
Signs of leukocytosis
It is often impossible to determine the presence of leukocytosis based on certain symptoms. In most cases, the pathology occurs unnoticed by the patient. Clinical manifestations are observed when the level is significantly exceeded. This condition can only be provoked by very serious pathologies, the signs of which will not go unnoticed by the patient. The main features include:
- Unreasonable weakness and fatigue
- Decreased ability to work
- Frequent dizziness
- Brief fainting
- Decreased appetite and resulting weight loss
- Increased work of sweat glands
- Labored breathing
Against the background of leukocytosis, the patient's lymph nodes may become enlarged. During diagnostic procedures, an enlargement of the liver or spleen is sometimes detected. Some patients experience deteriorating vision and discomfort in the abdominal area, characterized as tingling.
Due to changes in qualitative and quantitative blood parameters, bruising, increased sensitivity of the mucous membranes, and bleeding gums are noted. A slight excess of the norm of leukocytes is not accompanied by noticeable manifestations, however, the patient may experience symptoms of diseases that led to leukocytosis.