Complexes with this research
Women's check-up No. 1 38 studies for annual preventive examination RUB 19,290 Composition
Male infertility. Extended examination Analysis of male reproductive health 29,030 RUR Composition
Nutritionist recommends Metabolic status assessment RUB 7,570 Composition
IN OTHER COMPLEXES
- Men's check-up No. 1 RUB 18,570
- Advanced anti-aging diagnostics in postmenopause RUB 29,230
- Fitness monitoring 6,780 RUR
- Prevention of fetal malformations RUB 7,130
- Stress complex 4,310 RUR
How does TSH affect pregnancy?
TSH itself has no effect on the course of pregnancy. The functioning of the thyroid gland depends on its content in the blood. The hormone has a stimulating effect. With its deficiency, the formation of thyroxine and triiodothyronine by thyroid cells slows down. Excessive amounts of TSH leads to an increase in their synthesis.
As a result of hormonal imbalance:
- the general condition of the pregnant woman worsens - toxicosis, headaches and heart pain, fatigue, anemia, pressure changes;
- the formation of the placenta and the nutrition of the fetus are disrupted;
- the growth and development of the child is inhibited;
- childbirth occurs with complications.
Detailed description of the study
Thyroid-stimulating hormone (TSH) serves as an important link in the regulation of the thyroid gland. It is produced by a small organ located in the brain called the pituitary gland. According to its structure, it belongs to the endocrine glands. TSH acts on thyroid cells to produce and release the thyroid hormones thyroxine (T4) and triiodothyronine (T3) into the blood.
T4 and T3 help regulate the speed of the body's metabolic processes. They are also important for the normal development of pregnancy. The thyroid gland produces more thyroxine, but it is inactive and is converted into the much more active T3 in the tissues.
TSH, together with thyrotropin-releasing hormone (TRH), coming from the hypothalamus, helps maintain sufficient concentrations of thyroxine and triiodothyronine in the blood.
In case of reduced levels of these hormones in the blood, the pituitary gland increases the production of TSH under the influence of TRH. TSH released into the blood stimulates the production of T4 and T3. With an increased content of these hormones in the body, the reverse mechanism begins to operate. The pituitary gland produces less TSH, which leads to lower levels of thyroxine and triiodothyronine. Normally, such a system allows you to stabilize the content of thyroid hormones in the blood.
If the thyroid gland produces excessive amounts of T4 and T3, a person experiences symptoms caused by an overactive thyroid gland (hyperthyroidism). These include weight loss, sweating, mood swings, anxiety, sleep disturbances and some other manifestations.
The most common cause of this condition is Graves' disease, an autoimmune disease in which the patient's immune system produces autoantibodies that activate the TSH receptor. This leads to the production of excessive amounts of thyroid hormones. In response, the pituitary gland produces less TSH, causing the level of this hormone in the blood to decrease.
An underactive thyroid gland is called hypothyroidism. In this case, symptoms such as weight gain, dry skin, excessive sensitivity to cold, and constant fatigue may be observed.
Hashimoto's thyroiditis is the most common cause of hypothyroidism. This is a chronic autoimmune disease in which the immune response causes inflammation of the gland, as well as the production of antibodies to the cells of the own thyroid gland. With Hashimoto's thyroiditis, hormone production decreases. As a result, the pituitary gland usually increases the release of TSH.
However, solely assessing TSH concentrations does not always predict or reflect thyroid disease. Some people with pituitary disease produce an abnormal form of TSH that does not function properly. They often have hypothyroidism despite TSH levels being normal or slightly elevated.
Changes in the amount of TSH may be associated with disruption of the pituitary gland. In addition, hyperthyroidism or hypothyroidism occurs if damage to another gland, the hypothalamus, is detected.
TSH (Thyroid Stimulating Hormone)
Description
TSH (thyroid-stimulating hormone) is a pituitary hormone that stimulates the formation and secretion of thyroid hormones (T3 (Triiodothyronine), T4 (Thyroxine)). Marker of regulation of thyroid function.
Indications for the purpose of analysis
- Detection of hidden hypothyroidism.
- For dynamic observation and assessment of the effectiveness of treatment for detected hypothyroidism (lifelong 1 - 2 times/year).
- For dynamic observation and assessment of the effectiveness of treatment for detected diffuse toxic goiter (1.5 - 2 years, 1 - 3 times/month).
- Delayed mental and sexual development in children.
- Goiter.
- Cardiac arrhythmias.
- Myopathy.
Norms
0.23 – 3.4 µIU/ml
Level up
- thyrotropinoma;
- basophilic pituitary adenoma (rare);
- syndrome of unregulated TSH secretion;
- thyroid hormone resistance syndrome;
- primary and secondary hypothyroidism;
- juvenile hypothyroidism;
- uncompensated primary adrenal insufficiency;
- subacute thyroiditis and Hashimoto's thyroiditis;
- ectopic secretion in lung tumors;
- pituitary tumor;
- severe somatic and mental illnesses;
- severe gestosis (preeclampsia);
- cholecystectomy;
- contact with lead;
- excessive physical activity;
- hemodialysis;
- treatment with anticonvulsants (valproic acid, phenytoin, benserazide), beta-blockers (atenolol, metoprolol, propranolol), taking drugs such as amiodarone (in euthyroid and hypothyroid patients), calcitonin, neuroleptics (phenothiazine derivatives, aminoglutethimide), clomiphene, antiemetics agents (motilium, metoclopramide), ferrous sulfate, furosemide, iodides, radiocontrast agents, lovastatin, methimazole (Mercazolil), morphine, diphenin (phenytoin), prednisone, rifampicin.
Downgrade
- toxic goiter;
- thyrotoxic adenoma;
- TSH-independent thyrotoxicosis;
- pregnancy hyperthyroidism and postpartum pituitary necrosis;
- T3 toxicosis;
- latent thyrotoxicosis;
- transient thyrotoxicosis with autoimmune thyroiditis;
- thyrotoxicosis due to self-administration of T4;
- pituitary injury;
- psychological stress;
- starvation;
- taking drugs such as anabolic steroids, corticosteroids, cytostatics, beta-adrenergic agonists (dobutamine, dopexamine), dopamine, amiodarone (hyperthyroid patients), thyroxine, triiodothyronine, carbamazepine, somatostatin and octreotide, nifedipine, drugs for the treatment of hyperprolactinemia (metergoline, peribedil, bromocriptine).
Information for specialists
TSH (Thyroid-stimulating hormone) - Produced by basophils of the anterior pituitary gland under the control of thyroid-stimulating hypothalamic releasing factor, as well as somatostatin, biogenic amines and thyroid hormones.
Increases vascularization of the thyroid gland. Increases the supply of iodine from blood plasma to thyroid cells, stimulates the synthesis of thyroglobulin and the release of T3 and T4 from it, and also directly stimulates the synthesis of these hormones. Enhances lipolysis.
There is an inverse logarithmic relationship between the concentrations of free T4 and TSH in the blood.
TSH is characterized by daily fluctuations in secretion: blood TSH reaches its highest values at 2 - 4 am, the highest level in the blood is also determined at 6 - 8 am, the minimum TSH values occur at 17 - 18 pm. The normal rhythm of secretion is disrupted when awake at night. During pregnancy, the concentration of the hormone increases. With age, the concentration of TSH increases slightly, and the amount of hormone emissions at night decreases.
TSH level for pregnancy
For pregnancy to occur, the TSH level is considered optimal, which does not go beyond 1.5-2.5 µIU/ml, while it should normally be from 0.3 to 4.2 units. This narrow range is due to the fact that often the cause of infertility is damage to the thyroid gland.
Therefore, at the stage of planning conception or when entering an IVF (artificial insemination) program, it is recommended to undergo a complete examination of the thyroid gland by an endocrinologist. If there are deviations in hormone levels, drug treatment is carried out - levothyroxine, iodine or drugs that inhibit the synthesis of thyroxine (Mercazolil, Espa-carb) are recommended.

Why is elevated TSH detected during pregnancy?
Elevated TSH during pregnancy is a sign of low thyroid function, diseases of the pituitary gland, and the hypothalamus of the brain. These disorders cause changes in metabolism, heart function, digestive system, and toxicosis. This is dangerous for the mother (swelling, weight gain, constant weakness, convulsions). The consequences for the child include inhibition of growth and development.
Main reasons
Thyroid-stimulating hormone increases for the following reasons:
- autoimmune inflammation (formation of antibodies to one’s own cells) – Hashimoto’s thyroiditis;
- lack of iodine in water and food;
- congenital predisposition to thyroid diseases;
- endemic goiter (characteristic of the area of residence);
- removal of part or all of the gland;
- diseases of the pituitary gland, hypothalamus - tumors with the formation of thyrotropin;
- recovery after a long illness;
- severe course of late toxicosis;
- low adrenal function.
Moreover, the first two reasons occur in more than 85% of cases.
Symptoms of change
Clinical manifestations may be completely absent. Their severity depends on the level of thyroid hormones. It can be low (little thyroxine) if the cause is diseases of the pituitary gland or high if the gland is affected and there is not enough iodine in the diet. The last factor is more common. It leads to hypothyroidism with the following symptoms:
- lethargy, slowness;
- constant drowsiness;
- cold, pale skin;
- poor tolerance to cold, chilliness;
- swelling;
- rapid weight gain;
- constipation;
- elevated blood cholesterol.

Why is it dangerous for mom?
Thyroid dysfunction causes dangerous complications during pregnancy:
- swelling;
- increased blood pressure;
- slow heart rate;
- fainting conditions;
- anemia (lack of hemoglobin and red blood cells), resistant to treatment with iron supplements and vitamins;
- convulsions;
- an increase in the size of the thyroid gland with compression of the tissues of the neck - difficulty swallowing and breathing;
- early and late toxicosis.
Consequences for the child
A lack of thyroid hormones is accompanied by severe consequences for the child. It is especially harmful in the first months of pregnancy. At this time, the fetus is completely dependent on the function of the mother's gland. If there is little thyroxine and triiodothyronine, then the formation of the nervous system and brain suffers.

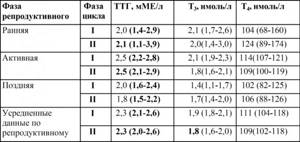
TSH norm during pregnancy: changes by week, trimester
TSH during pregnancy changes normally by week and trimester. With a healthy thyroid gland, it first decreases and then gradually increases from 10 weeks. Monitoring its level in the first trimester is important.
By trimester
In pregnant women, normal TSH levels by trimester have been revised several times. According to the latest recommendations, the range of fluctuations in µIU/ml values is established:
- first trimester – 0.1-2.5;
- second trimester – 0.3-3;
- third trimester – 0.4-3.5.

The upper limit of normal TSH during pregnancy for the 2nd trimester
By week
During pregnancy, changes in TSH by week are allowed, but normally they should correspond to the given intervals by trimester. Therefore, in the laboratory, opposite the obtained indicator, the acceptable values for each period of pregnancy will be given.
1st trimester
The first 3 months of gestation (1st trimester) are characterized by an increase in the hormone produced by the embryonic membrane - chorion. It is called human chorionic gonadotropin and is structurally similar to TSH. Therefore, its molecules stimulate the cells of a woman’s thyroid gland. It increases slightly in size and begins to intensively produce thyroxine.
The pituitary gland, on the contrary, inhibits the production of thyrotropin, since the thyroid gland is already working actively. In multiple pregnancies, TSH is close to zero. The situation changes at 10-11 weeks. Human chorionic gonadotropin is no longer needed, since the placenta begins to work, it falls, and TSH increases. This trend continues until childbirth.
Consequences for mother and fetus
When TSH is below normal, this is accompanied by negative consequences for the fetus and the pregnant woman:
- early toxicosis with uncontrollable vomiting;
- severe pregnancy;
- risk of early miscarriage, premature birth, cessation of fetal development, stillbirth;
- increased blood pressure;
- heart failure - palpitations, shortness of breath, swelling, enlarged liver;
- placental abruption;
- bleeding in the postpartum period.
Excess thyroid hormones inhibit the formation of the placenta. Malnutrition of the fetus often causes abnormalities in its development, some of which are incompatible with life. Children may be born with low body weight, increased excitability, and delays in physical and mental development.
Is it possible to get pregnant with high or low TSH?
With high TSH, conception usually occurs with difficulty, and low levels are less likely to affect the ability to become pregnant. In any case, deviations from the norm in the concentration of this hormone are a sign of thyroid dysfunction. Carrying a child against the background of such changes is accompanied by the risk of miscarriage and severe toxicosis.
Due to an imbalance of maternal hormones, the child may lag not only in growth and physical development, but also dementia. When TSH is low, the formation of the thyroid gland is inhibited. Therefore, gynecologists insist that the hormone be completely normalized before planning conception.
How to properly take a TSH test during pregnancy
A TSH test during pregnancy should be taken after preparation:
- Do not eat food for 8-10 hours, you are allowed to drink clean water;
- eliminate fatty foods 24-48 hours before;
- there should be no physical or emotional stress during the day;
- If any medications and vitamins are prescribed, then no later than 3 days in advance you should discuss with your doctor the need to discontinue them.
It is important to understand that food will not affect the test result, it cannot increase or decrease TSH, but fats change the composition of the plasma, so the data obtained may be inaccurate. It is important to come to the laboratory before 12 noon, since the level of the hormone is subject to daily fluctuations.
Blood is taken from a vein, and the study is carried out using immunological methods. For this, different reagents are used. Therefore, it is better to undergo repeated tests in the same institution as the first examination. If there are signs of acute infection, it is recommended to reschedule the test to other days.

How to normalize hormone levels
In order for the TSH level to be within normal values, it is necessary:
- undergo examination by an endocrinologist - ultrasound of the thyroid gland, blood test for TSH, thyroxine and triiodothyronine, antibodies to thyroid peroxidase, brain tomography (if indicated);
- identify the cause of changes in hormone concentrations and undergo drug treatment;
- change the iodine intake - with low thyroxine and high TSH, it is necessary to consume seafood, fish, iodized salt, and if the hormone ratio is reversed, they should be avoided.

If conservative therapy is insufficiently effective, surgery or radioactive iodine therapy is prescribed; it is important to undergo this treatment before pregnancy.
What does low TSH indicate during pregnancy?
During pregnancy, low TSH is normal, especially in the early stages, but it can also indicate increased thyroid function - thyrotoxicosis. Less common is a decrease due to diseases of the pituitary gland and hypothalamus due to injuries, inflammation, brain tumors, and vascular disorders.
Symptoms of decreased hormone levels
A decrease in the level of thyroid-stimulating hormone of the pituitary gland manifests symptoms only with increased thyroid function. It produces thyroxine in excess quantities. When its level increases, women complain of:
- weak weight gain as pregnancy progresses;
- sweating;
- intolerance to heat and stuffiness;
- increased appetite;
- hand trembling;
- strong and frequent heartbeat, pulsation in the head, neck, stomach;
- nausea, vomiting, diarrhea;
- rise in body temperature without signs of infection.

Pregnant women become very impressionable and tearful, and sleep is disturbed. Possible protrusion of the eyes, lacrimation, pain when looking at a light source, double contours of objects.