Types of diseases
Today, the most widespread lesions of the liver and gallbladder are associated with nutritional and metabolic disorders. Let's look at some of them.
Fatty hepatosis (liver steatosis, fatty liver, fatty liver) is an independent disease or syndrome caused by fatty degeneration of liver cells. There are primary and secondary fatty hepatosis. The causes of primary fatty hepatosis are obesity, type 2 diabetes mellitus, and hyperlipidemia. Secondary fatty hepatosis can develop when taking hepatotoxic drugs, as well as with chronic gastrointestinal diseases - such as pancreatitis, colitis, malabsorption syndrome, etc. and after surgical interventions on the intestines. Fatty hepatosis was identified in the 60s of the last century thanks to the introduction of liver puncture biopsy into clinical practice. It is characterized by pathological intra- and (or) extracellular deposition of fat droplets. The morphological criterion of fatty hepatosis is the content of triglycerides in the liver of more than 10% of dry weight.
Due to the benign course of the disease, there are practically no clinical signs of hepatosis. And fatty hepatosis itself can become the initial stage of a whole cascade of liver damage.
The disease is usually diagnosed accidentally and does not require special pharmacotherapy. If fatty hepatosis is detected, a special diet with limited spicy and fatty foods is usually recommended. The next nosology that fatty hepatosis can lead to is non-alcoholic steatohepatitis.
Non-alcoholic steatohepatitis (NASH) is an independent nosology, which is characterized by increased activity of liver enzymes in the blood and morphological changes in liver biopsies, similar to changes in alcoholic hepatitis. The term “non-alcoholic” means that the development of NASH is not associated with alcohol consumption. The main cause of the development of steatohepatitis is considered to be an increased content of free fatty acids in the liver. Most often, NASH has a benign and asymptomatic course, but in some cases liver cirrhosis, portal hypertension and liver failure can develop.
Similar to fatty hepatosis, primary and secondary NASH . The causes of primary NASH are also obesity, type 2 diabetes mellitus, and hyperlipidemia. Secondary NASH develops against the background of metabolic disorders, taking a number of medications (amiodarone, glucocorticosteroids, synthetic estrogens, tamoxifen, perhexiline maleate, methotrexate, tetracycline, NSAIDs), malabsorption syndrome and other disorders.
In NASH, there is increased activity of cytochrome P4502E1 in the liver, which is accompanied by the formation of reactive oxygen radicals and increased lipid peroxidation reactions.
Most patients with NASH do not have symptoms characteristic of liver disease. Some patients experience vague abdominal discomfort or heaviness, as well as aching pain in the right hypochondrium, and asthenic syndrome is quite pronounced. With small droplet steatosis - the most unfavorable option (many small lipid droplets are detected in hepatocytes, and the nucleus is located in the center of the cell), episodes of hemorrhage, fainting, hypotension, shock (mediated by the influence of tumor necrosis factor released during inflammation) may develop. Jaundice, ascites, and “liver signs” are rarely detected. Body mass index is the only independent factor for assessing the degree of fatty infiltration of the liver.
To date, no strict management regimens for patients with NASH have been developed. When choosing treatment, the presence of concomitant diseases and risk factors is taken into account. Gradual, moderate weight loss is most effective in cases of NASH development against the background of obesity and diabetes mellitus and is accompanied by positive dynamics of clinical and laboratory parameters and a decrease in the histological activity index.
Pharmacotherapy for NASH includes drugs that normalize lipid metabolism and have a direct cytoprotective effect (ursodeoxycholic acid drugs). Patients with NASH are also shown drugs with membrane-stabilizing and antioxidant effects (ademetionine, phospholipids).
Alcoholic liver disease (ALD), along with viral hepatitis, is one of the most pressing problems of modern hepatology.
It is believed that drinking more than 80 g of ethanol per day leads to clinically obvious liver disease in men; for women this dose is 2–4 times less. However, for the risk of developing alcoholic liver disease, drinking 30 g of ethanol per day is sufficient.
Chronic alcohol consumption is more dangerous in terms of the development of ALD: people who drink alcohol intermittently at least two days a week have a lower risk of ALD. Laboratory tests in patients with ALD reveal an increased concentration of serum proinflammatory cytokines: IL1, IL2, IL6, TNF. Morphologically, the following stages of liver damage are distinguished: fatty degeneration (liver steatosis); alcoholic hepatitis (balloon and fatty degeneration of hepatocytes, which was the reason for the introduction of the term alcoholic steatohepatitis); cirrhosis.
Clinically, ALD is manifested by the following symptoms: anorexia, discomfort and dull pain in the right hypochondrium or epigastrium, nausea, jaundice of the skin, itching, weight loss. At the stage of cirrhosis, splenomegaly, ascites, telangiectasia, palmar erythema, remitting or persistent fever reaching febrile levels, severe jaundice, hemorrhagic syndrome, hepatic encephalopathy, and renal failure appear.
Treatment of ALD involves, first of all, complete cessation of alcohol intake. For severe alcoholic hepatitis, glucocorticosteroids are used: prednisolone or methylprednisolone. Essential phospholipids have become widespread in the treatment of chronic forms of ALD. To improve the clinical and biochemical parameters of ALD, ursodeoxycholic acid and S-adenosyl-L-methionine (ademetionine), a natural substance that is formed in the body from methionine using ATP with the participation of the enzyme S-adenosylmethionine synthetase, are prescribed. Recently, the possibility of using chimeric antibodies to TNF-α (infliximab) and TNF-α inhibitors (etanercept) has been discussed (see article “Joint diseases” ).
Cholelithiasis (GSD) is a chronic recurrent disease of the hepatobiliary system, which is associated with impaired metabolism of cholesterol, bilirubin, bile acids and is accompanied by the formation of gallstones in the hepatic bile ducts (intrahepatic cholelithiasis), the common bile duct or the gallbladder.
Currently, cholelithiasis is considered as a hereditary-determined disease caused by increased formation in the body of 3‑hydroxy-3‑methylglutaryl-coenzyme A reductase, an enzyme that regulates the synthesis of cholesterol in the body. As a result, the level of cholesterol in bile increases (bile becomes lithogenic). The production of lithogenic bile by the liver aggravates cholestasis and contributes to the development of the inflammatory process in the gallbladder. Factors contributing to lithogenesis include irregular and irrational nutrition with a reduced content of dietary fiber in the diet, biliary dyskinesia, physical inactivity, obesity, and hemolytic anemia.
Clinical manifestations of cholelithiasis are associated with the development of calculous cholecystitis. The nature of the pain syndrome in cholelithiasis corresponds to that during exacerbation of chronic cholecystitis. Pharmacotherapy of cholelithiasis includes the use of chenodeoxycholic and ursodeoxycholic acid drugs, enterosorbents (lignin, cholestyramine, etc.), antispasmodics (belladonna derivatives, metamizole, aminophylline); hepatoprotective drugs. Indications for lithotripsy are single or multiple stones up to 30 mm in diameter, provided there are no morphological changes in the walls of the gallbladder.
Examples of performed operations:
- Laparoscopic Kasai surgery
- Mini laparotomy access for operations on the biliary tract
- Bypass operations (portosystemic, mesoportal, arterioportal bypasses)
- Endovascular occlusion of the duct of Arantius
- Endovascular embolization of liver hemangiomas
- Liver surgeries (hemihepatectomy, removal of cysts and tumors in the liver, and others)
- Surgeries on the pancreas (traumatic injuries, cysts, tumors, pancreatic malformations, calculous pancreatitis)
The Hepatobiliary Center has accumulated the largest world experience in portosystemic shunting - 791 shunt operations. Elimination of the risk of bleeding after the first operation is 96.5%.
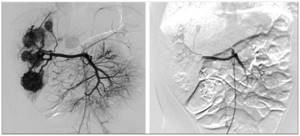
Angiography before surgery (discharge to varicose veins of the esophagus and stomach)
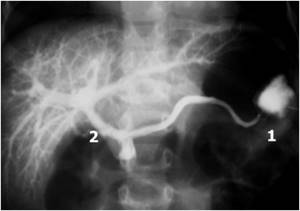
Angiography after surgery (discharge to varicose veins of the esophagus is not detected)
The Center performed 81 mesoportal bypass operations
Complete restoration of portal perfusion was observed in 91.4% of surgical interventions.
For the first time in the Russian Federation, endovascular occlusion of the duct of Arantius was performed
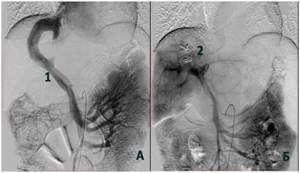
Angiography before and after occlusion of the duct of Arantius
Multiple liver hemangiomas before and after endovascular embolization
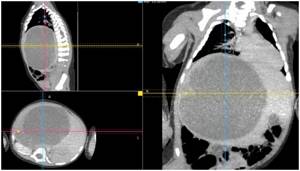
Cystic formation of the right lobe of the liver in an 8-month-old child
Hepatoprotectors
Preparations containing essential phospholipids (EPL)
EPL substance is a highly purified soybean extract containing predominantly phosphatidylcholine (PC) molecules with a high concentration of polyunsaturated fatty acids (PUFAs). The main active ingredient of EPL is 1,2‑dilinoleoyl-phosphatidylcholine, the synthesis of which is impossible for the human body. EPL molecules are integrated directly into the phospholipid structure of damaged liver cells, replacing defects and restoring the barrier function of the lipid bilayer of membranes. In this way, the membrane-stabilizing and hepatoprotective effect of EPL is achieved. Phospholipid PUFAs increase the activity and fluidity of membranes, reduce the density of phospholipid structures, and normalize membrane permeability. Exogenous EPL promotes the activation of phospholipid-dependent enzymes and transport proteins located in the membrane, which, in turn, supports metabolic processes in liver cells and increases its detoxification and excretory potential.
The hepatoprotective effect of EPL is based on inhibition of lipid peroxidation processes, the leading pathogenetic mechanism of liver damage. EPL preparations can be additionally enriched with various vitamins: B1, B2, B6, B12, E and nicotinic acid, since deficiency of these vitamins often develops with liver damage. Phospholipids can also be found in combination with the amino acid methionine. Methionine is necessary for the synthesis of choline, increases the formation of this integral part of EPL and increases the level of endogenous phospholipids, reducing the deposition of neutral fat in the liver.
Methionine is also necessary for the detoxification of xenobiotics (including ethanol). In atherosclerosis, methionine reduces the concentration of cholesterol and increases the concentration of blood phospholipids. Another phospholipid combination consists of phosphatidylcholine and glycyrrhizic acid. Glycyrrhizic acid complements the effects of EPL with an immunostimulating effect by stimulating phagocytosis and increasing the activity of NK cells and inducing γ-interferon. In addition, glycyrrhizic acid has an antiviral effect, blocking the penetration of viruses into cells, and exhibits antioxidant properties.
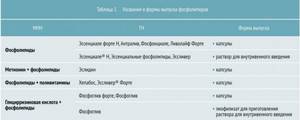
Table 1 presents the INN, TN and release forms of phospholipids present on the domestic market.
Analogues of ademetionine
Among hepatoprotectors used for liver damage, ademetionine is considered one of the most effective. S-adenosyl-L-methionine, which is part of it, is an analogue of intracellular ademetionine, a biological substance present in all organs and tissues. At the same time, the maximum content of ademetionine is in the liver and brain. The latter fact explains the dual effect of the drug - hepatoprotective and neuroprotective. S-adenosyl-L-methionine increases the fluidity of cell membranes and normalizes the functioning of intracellular transport systems, thus stimulating the production and outflow of bile, as well as the flow of bile acids from hepatocytes into the biliary system.
Restoring the outflow of bile from hepatocytes prevents its excessive accumulation in cells and damaging effects on membranes. In addition, the drug stimulates the regeneration and proliferation of hepatocytes, which makes it possible to compensate for liver function even at a late stage of liver pathology, increasing patient survival.
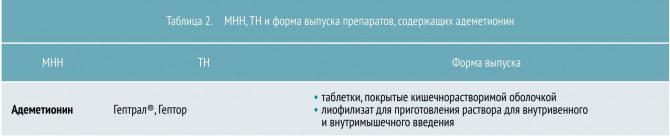
By increasing the synthesis of glutathione, taurine and cysteine - natural factors of antioxidant protection in the body, ademetionine preparations prevent the harmful effects of free radicals, bile acids and other toxic agents on liver cells. Table 2 presents ademetionine preparations registered in the Russian Federation.
Ursodeoxycholic acid preparations
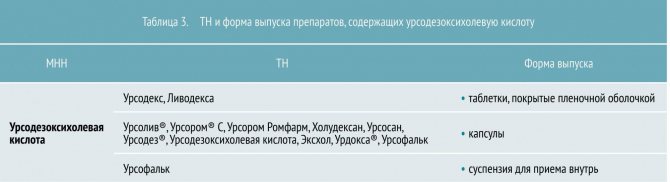
Another effective drug for liver damage is ursodeoxycholic acid, which has a wide spectrum of action. Firstly, by being integrated into the membranes of liver cells, it stabilizes their structure and protects against the damaging effects of bile salts (hepatoprotective effect). Secondly, it stimulates exocytosis and cleanses hepatocytes of toxic bile acids (BAs), the concentrations of which are increased in liver diseases. It is this property that makes ursodeoxycholic acid a special hepatoprotector. In addition, acid reduces the absorption of lipophilic FAs in the intestine, increasing their turnover during enterohepatic circulation. At the same time, choleresis and the removal of toxic fatty acids through the intestines are enhanced. The acid also reduces the lithogenicity of bile, prevents the formation of stones and dissolves already formed stones. Table 3 presents technical specifications and release forms of drugs based on ursodeoxycholic acid.
Herbal preparations based on silymarin
Silymarin is a mixture of isomeric flavonoids from milk thistle with a predominance of silibinin. Bioflavonoids activate the synthesis of proteins and enzymes in hepatocytes, improve metabolism in cells, stabilize the membranes of liver cells, slowing down the entry of toxic metabolic products into them, and improve the body’s immunological reactivity. In addition, silymarin, by reducing elevated levels of transaminases in the blood serum, inhibits dystrophic and potentiates regenerative processes in the liver. Milk thistle preparations prevent the accumulation of lipid hydroperoxides and reduce the degree of damage to liver cells (antioxidant effect).
Currently, several drugs containing milk thistle fruits are presented on the Russian pharmaceutical market, both in pure form and in combinations. Preparations containing, in addition to milk thistle, also extracts of tansy, St. John's wort and birch leaves, have hepatoprotective, membrane-stabilizing, regenerating, antioxidant and choleretic effects. They normalize lipid and pigment metabolism, enhance the detoxification function of the liver, inhibit lipid peroxidation processes in the liver and normalize intestinal motility (INN and TN are presented in Table 4).

Preparations containing flavonoids from other plants
Among representatives of this category, products based on artichoke leaf extract are quite widely used. The main hepatoprotective and choleretic effect of this substance is due to the presence in it of the phenolic compound cynarin in combination with phenolic acids (caffeic, chlorogenic, etc.). In addition to them, the artichoke contains carotene, vitamins C, B1, B2, which is important due to the disruption of normal liver function.
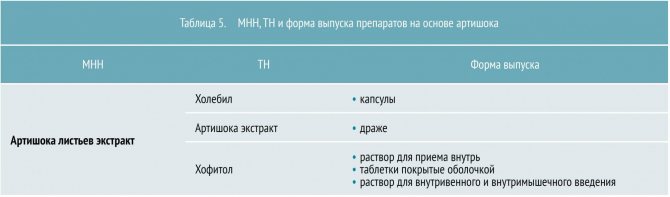
Artichoke extract affects the functional activity of liver cells, stimulates the production of enzymes, thereby affecting lipid and fat metabolism and increasing the antitoxic function of the liver. Artichoke reduces cholesterol levels in the blood during initial hypercholesterolemia, has a choleretic effect due to a moderate choleretic and weak cholekinetic effect. The INN and TN of artichoke-based drugs are presented in Table 5.
Another well-known drug of the subgroup under consideration is a drug containing extracts of spiny caper, western cassia, black nightshade fruits, as well as extracts of Tamarix dioica and Terminalia chebula fruits. The drug protects the liver parenchyma from toxic agents, enhances intracellular metabolism and stimulates regeneration. Only one drug with this INN is registered on the pharmaceutical market of the Russian Federation, under the trade name Liv.52, available in the form of tablets and drops for oral administration.