Azizova Muslimat Akhmedovna, gynecologist
— Please tell us about cervical diseases and the common diagnosis of cervical dysplasia, which frightens women so much
— Yes, indeed, there are many diseases of the cervix, but the main pathology of the cervix, dangerous to a woman’s life, is cervical cancer (CC). Therefore, all diagnostic methods and techniques for examining the cervix were developed for the early and differential diagnosis of this particular disease and its obligate precancer.
Dysplasia or, according to international terminalology, cervical intraepithelial neoplasia (CIN) of three degrees is initiated by a persistent infection caused by high carcinogenic risk human papillomaviruses (HPV HCR), which supports the progression of damage to invasion. CIN I with a high probability of regression to CIN II-III are true precancerous lesions. They precede cervical cancer for several years and even decades.
— What is the difference between dysplasia 1, 2 and 3? And do I understand correctly that dysplasia and Cin are the same thing?
- YES indeed, dysplasia is used in Russian terminology for cytological examination of the cervix and cin (cin) in histologists and international classification.
- CIN I - undifferentiated cells occupy the lower third of the epithelial layer.
- CIN II - immature cells occupy the lower two-thirds of the thickness of the epithelium;
- CIN III - immature abnormal cells occupy more than two-thirds of the thickness of the epithelial layer or its entire thickness, but there is no invasion into the underlying stroma
All three of the following classifications exist today.
Correlation of classifications of precancerous lesions of the cervix
| Papanicolaou system | WHO Descriptive System | CIN | TBS (Bethesda Terminological System) |
| Class 1 (normal) | No malignant cells | No neoplastic changes | Norm |
| Class 2 (epithelial metaplasia, inflammatory type) | Atypia associated with inflammation | Reactive changes in ASC cells: ASC - US; ASC - N | |
| Class 3 (“dyskaryosis”) | Mild dysplasia | CIN I Koilocytosis | LSIL |
| Moderate dysplasia | CIN II | HSIL | |
| Severe dysplasia | CIN III | ||
| Class 4 (cells suspicious for cancer or carcinoma in situ) | Carcinoma in situ | ||
| Class 5 (cancer) | Invasive carcinoma | Carcinoma | Carcinoma |
— How can we identify these cells in ourselves and prevent or “catch” the early stage of the malignant process?
— To determine, you need to take a smear for oncocytology from the cervix along
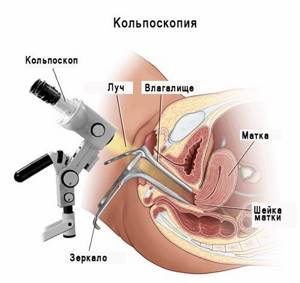
Pap or Betesta, and do a colposcopy once a year
-Do you need special training?
— No, you don’t need any special preparation, but it’s better not to take a smear:
- earlier than 48 hours after sexual intercourse;
- during menstruation;
- during the treatment of genital infections;
- earlier than 48 hours after extended colposcopy with treatment with 3-5% solutions of acetic acid or Lugol, after using lubricants, tampons or spermicides;
- after vaginal examination or douching.
-What is the difference between a cytology test and a biopsy?
A biopsy is the last stage of examination of the cervix after cytology and colposcopy. Cytology is the study of cells and biopsy is the study of cervical tissue.
Detailed description of the study
Liquid oncocytology is a laboratory diagnostic method that is alternative to conventional oncocytology, which is currently common. The difference between liquid cytology and conventional cytology is that the material taken is placed in a liquid medium, from which cyto-preparations are then formed in a special centrifuge. They consist of “washed cells” that are concentrated in one place and form an even layer. This makes the cytologist’s conclusion much more reliable compared to conventional smears, when the material is immediately applied to the glass. Liquid cytology is recognized by many world organizations (FDA, American Cancer Society, etc.), recommended by international consensuses for effective screening of cervical cancer. Numerous studies have shown that liquid-based cytology is more informative than conventional cytology, and, therefore, qualitatively improves diagnosis.
A feature of endometrial cancer is that it is asymptomatic for a long time, and the vast majority of patients have a hormonally dependent variant of the tumor (60–90%), which develops against the background of hyperestrogenism, as well as against the background of a whole complex of complex endocrine and metabolic disorders, in particular pathology ovulatory process, disorders of carbohydrate and lipid metabolism. The first, estrogen-dependent, path of development of endometrial cancer occurs slowly and is characterized by a favorable clinical course and sensitivity to hormonal therapy. The second variant of oncogenesis is associated with mutations in suppressor genes and is characterized by a more aggressive course, as well as a lack of sensitivity to hormonal therapy. This situation requires the selection of patients with a poor prognosis for appropriate more aggressive treatment and monitoring. However, the biological behavior of an endometrial tumor remains quite unpredictable even for patients with the same extent of the tumor process. In this regard, recently, great importance has been attached to immunohistochemical markers for predicting the clinical course of various neoplasms and their outcome.
Indications for performing a biopsy are
- abnormal cytological results of smears;
- pronounced changes during extended colposcopy;
— abnormal colposcopic pictures (ACC);
— discrepancy between the results of the cytological method of examination and extended colposcopy

-Part 2
- If you have any abnormalities in your analysis?
ASC-US (questionable) Women 25 and older
ASC-US is the most common abnormal cytology finding and is associated with the lowest risk of CIN3+, in part because in approximately one-third of cases, ASC-US is not associated with HPV infection. The risk of CIN3+ in women with ASC-US does not exceed 2%, therefore, observation with repeat cytological examination after a year, or HPV testing, which is preferable, is possible.
In the absence of HPV, co-testing after 3 years.
If HPV is detected, colposcopy is performed; if abnormal patterns are detected, a biopsy is performed; if they are absent, co-testing is performed a year later.
For ASCUS with a positive HPV test, it may be appropriate to triage women using immunocytochemical tests with staining for P16 and ProExC.
Moreover, in women with a positive test for HPV types 16 and/or 18, the overall risk of developing CIN III or microinvasion over the next 3 years is about 21%, and for other types - no more than 5%
Analysis of pipel biopsy of the endometrium of the uterus: indications and contraindications
Pipel biopsy replaces the painful procedure of conventional biopsy, which is dangerous with complications, from medical practice. It is performed for the same indications
:
- examination of endometrial tissue in female infertility;
- bleeding - in patients over 40 years of age, during hormonal contraception, therapy, during menopause;
- as an element of a comprehensive examination of the uterus simultaneously with transvaginal ultrasound or hysteroscopy.
- when obtaining a tissue sample from patients with diabetes mellitus, the risk of spreading cancer cells and endometriosis.
The ability to obtain fragments of different tissues significantly increases the value of simultaneous comprehensive examinations.
Pipelle biopsy has a minimal number of contraindications
:
- infectious diseases of the genital organs;
- inflammatory processes in the vagina and cervix;
- pregnancy.
Women 21-24 years old
For ASCUS, repeat cytology annually; immediate colposcopy is not indicated. If ASCUS is repeated or the HPV test is positive, a colposcopy is performed; in accordance with the results of the colposcopy, a biopsy is performed.
Women following surgery for CIN
ASCUS in women observed after treatment for CIN - colposcopy.
Pregnant
Colposcopy can be postponed until the postpartum period (6 weeks after birth).
women with LSIL ( low grade squamous intraepithelial lesion)
LSIL are significantly more often associated with HPV infection than ASC-US (77% of women with LSIL have HPV)
Women with LSIL and positive HPV - colposcopy for:
— Negative HPV — repeat co-testing after 1 year,
- Positive HPV or pathology in smears - colposcopy, biopsy if indicated,
- Negative results of both tests - re-screening after 3 years.
Pregnant
For LSIL - colposcopy. If there is no suspicion of severe damage, re-examination after childbirth.
Types of biopsy
Outdoor. This is the collection of biomaterial for research directly under “eye control”, for example, for visible mucous membranes, skin, etc.
Internal. Such a biopsy involves taking a piece of tissue using a special method, for example, by puncture (using a needle), which is usually carried out under ultrasound guidance.
You can find out details about performing a biopsy at the SM-Clinic in St. Petersburg by calling us or ordering a call back.
| Name of service (price list incomplete) | Price, rub.) | In installments* |
| Collection of material for histological examination | 500 | — |
* You can read more about the conditions here - Treatment on credit or in installments.
Postmenopausal women
HPV testing and colposcopy are indicated for any test results.
ASC-H
The risk of CIN 3+ in ASC-H is higher than in ASC-US or LSIL, but lower than in HSIL. This risk increases with age. Colposcopy is indicated for all patients, regardless of HPV status, including women under 25 years of age.
Women HSIL (high grade squamous lesion)
For HSIL, urgent colposcopy is indicated. However, triage based on repeat smear results or HPV status is not acceptable. And when the ST is completely visible, the detected CIN lesions are immediately excisively excised not only for diagnostic purposes, but also for therapeutic purposes—the “see and treat” approach. In case of incomplete visibility of the ST, LLETZ is indicated for diagnostic purposes. Destruction of lesions is unacceptable!
AGC/AIS
If AGC or AIS is detected, colposcopy with cervical curettage is indicated, regardless of the results of HPV testing. By the way, in women over 35 years of age, taking an aspirate from the uterine cavity is indicated to exclude endometrial pathology.
Dispensary observation.
For all benign (background) diseases of the cervix (1st dispensary group), dynamic observation is indicated once a year with extended colposcopy; cytological examination, monitoring of PCR of discharge from the cervical canal for HPV VCR. And further tactics after surgical treatment of CIN II-III/CIS (intensive observation or, in case of relapse, repeated excision) are determined taking into account the results of the Pap test and HPV test, the type of CT, the woman’s age, and her reproductive plans. In case of relapse of CIN II-/CIS, repeated conizations (2-3) are highly likely to cure the patient and avoid hysterectomy.
These clinical recommendations, according to the order dated November 2, 2017, determine the main directions for the diagnosis and management of patients with benign and precancerous diseases of the cervix, however, a justified deviation from this protocol with an expansion of the scope of the examination is not a mistake.
Share link:
- Telegram
Cytology
It is carried out to evaluate the morphological specifications of the elements of tissue cells of various organs, as well as fluids and various types of body secretions.
The procedure helps doctors understand the essence of dysplastic and malignant transformations of specific cells and, based on the collected information, make a preliminary diagnosis.
The method has its advantages:
- It is available;
- Economical for the patient;
- Does not require complex expensive equipment;
- The duration is 60 minutes;
- Non-invasive or minimally invasive (here it all depends on the method of sampling the material chosen by the doctor).
Agree, the listed advantages explain the wide popularity of the study; it is readily used, for example, as part of the initial examination of various diseases.
The specifics of the material removal became the basis for the following classification of the study:
- Preoperative;
- Intraoperative.
The first has the following types:
- Exfoliative. Here, the object of analysis is the discharge of the genitourinary organs, sputum, sweat, urine, etc. This type has one significant drawback - the safety of the material leaves much to be desired.
- Abrasive. The object of study is scrapings from areas of internal organs. To remove the material, the doctor uses special tools. This approach allows the material to be well preserved, which means the result will be clearer.
- Aspiration. A fine-needle biopsy technique is used. This gives the doctor the widest possible access to any organ. This method has found widespread use in the diagnosis of breast tumors at an early stage of their development.
Cytological analysis alone, with all its undeniable advantages, is not enough to perform a final analysis. Using the method, the doctor can determine the presence of a malignant neoplasm, nothing more. There are modern techniques, thanks to which a preliminary diagnosis is made more accurately and, based on it, the doctor can plan treatment tactics.
A few words must be said about cytological examination in gynecology. Here it manifests itself as a highly informative, absolutely safe method that gives the doctor the necessary picture to begin treatment in the presence of an identified pathology.
Cytology of a cervical smear is a necessary and mandatory measure in terms of diagnosing diseases of a woman’s genital area.
The procedure itself does not cause any inconvenience or anxiety to the patient; it is painless and does not take a long time.










