For timely diagnosis and further treatment, all women aged 21 to 30 years are recommended to undergo colposcopy with cytology at least once a year, and then, in the absence of pathologies, it is prescribed once every 3 years.
So what is colposcopy, is it necessary to carry it out together with a cytological examination, and most importantly, what are the differences between these gynecological methods of examining the cervix? This article is about all this and some important nuances.
What is the difference between colposcopy and cytology?
Colposcopy is a non-invasive method of examining the walls of the vagina and cervix. This type of examination is carried out by a specialist exclusively using gynecological mirrors and a special device - a colposcope, which magnifies the tissue of the cervical canal by 40 times, thereby allowing a more careful study of the color, shape and relief of the mucous membrane.
This method of study is rightfully considered one of the safest and most painless, which is why it is often prescribed to both pregnant women and women after childbirth to identify the following diseases:
- cervical cancer and various degrees of its erosion;
- polyps and growths of atypical cells;
- various inflammatory processes of the vagina and cervix (exocervicitis);
- death of particles and fragments of mucous surfaces.
Important! Statistics show that women aged 35 to 55 are at risk of developing cervical cancer. It follows from this that colposcopy with cytological examination should become a mandatory procedure when examining a patient, especially after 30.
In addition to a standard examination with a colposcope by a gynecologist, various solutions can be used, with the use of which the reaction of the surface of the mucous membrane of the cervical canal can describe in more detail the condition of the tissues of the vagina and cervix.
Often, during a colposcopy, a specialist decides to take a smear of internal tissue for cytological examination.

Thanks to cytology, a more accurate and completely painless study of tissues under a microscope is possible. Laboratory analysis allows a specialist to diagnose atypical cell behavior at an early stage and identify abnormalities.
From the above it follows that the most important difference between calposcopy and cytology is the subject of research. So for colposcopy, the main thing is the relief, shape and color of the walls of the vagina and cervix, which the gynecologist examines, albeit using a microscope, but still only visually. Cytology, in turn, more carefully studies in the laboratory the cellular structure of the mucous membranes of the patient’s genital organs.
Is colposcopy necessary if cytology is normal?
A cytological examination of the cervix is prescribed during an examination by a gynecologist to identify pathological or inflammatory processes. Cytology can give two types of results:
- positive - pathological or atypical cells have been identified, which are either the result of an inflammatory process inside the female genital organs or will cause the development of diseases;
- negative - the tissues are healthy and no abnormalities have been detected.

In cases where the result of a laboratory test for cytology is negative, the gynecologist may nevertheless prescribe an additional examination with a colposcope, since during this examination the gynecologist will determine exactly what abnormalities occur in the development of the vaginal and cervical mucosa.
Good colposcopy and bad cytology
What should happen if, as a result of the research, a good colposcopy and bad cytology are obtained - a specialist will take an additional biopsy of mucosal tissue for examination.
In cases where, after a colposcopic examination, no abnormalities are revealed, but cytology still indicates a change in the morphology of tissue cells, the gynecologist conducts an additional examination of the tissues, types of pathological process in the cells are identified, and further treatment is determined.
Smear examination
The examination of the smears themselves is carried out by specialists from cytological laboratories - laboratory assistants and cytologists. The resulting smear is prepared, stained with special dyes and then examined under a microscope.

A doctor or laboratory technician evaluates the quality of the material taken, the coloring of the smear, the number of cells of different types, their shape and structure. Next, a conclusion is made. The CIS countries are still working at the junction of two classifications of PAP smears.
The old classification of 1960-70 included the concepts:
- Norm;
- Inflammation;
- Dysplasia or CIN of three degrees;
- Suspicion of cancer;
- A certain type of cancer.
Now the CIS countries are trying very hard to switch to the Bethesda classification from 2001, but getting used to it will take more than one year. This is a completely different system, so even the best and most modern doctors find this transition difficult. There are abbreviations for each microscopic smear pattern: NIL, LSIL, HSIL, and so on.
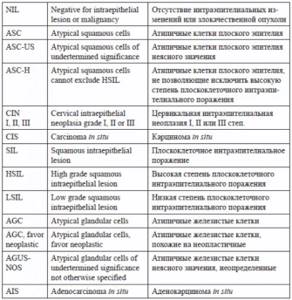
You can see how many possible answers there are for a smear according to this classification. That is why only a gynecologist can evaluate the result, taking into account the specific clinical situation of each individual patient.
We have presented these classification options so that our patients understand that, at the moment, they can get the result of a cytological smear using both options. It is up to the gynecologist to understand their results and make some decisions on the prescription of treatment and examination.
How to properly prepare for colposcopy with cytology
Two such similar and yet different procedures are often an integral part of each other, so the preparation for both methods of examination is the same.
For the most accurate and correct result from a colposcopic examination with cytology, the patient will need to comply with several fairly simple preparation conditions:
- The examination takes place on days 5-7 of the cycle (1-3 days after the end of menstruation);
- sanitary and hygienic procedures are carried out without any means or devices, exclusively using warm water;
- abstinence from sexual relations for several days preceding the study;
- refusal to use pharmaceutical and intravaginal products (tampons, suppositories and tablets can cause changes in tissue relief and have a bad effect on the cytology result).
With proper preparation, the result of colposcopy and cytological examination will most accurately reflect the state of tissues and cells, which will help to diagnose the disease in advance, and therefore prevent morphological changes in the structure of cells.
TREATMENT OF CERVICAL CANCER
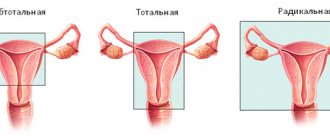
- Stage IA1:
- in patients of reproductive age, high and wide conization of the cervix is performed, followed by curettage of the mucous membrane of the remaining part of the cervical canal and, if indicated, the uterine cavity; — in the presence of concomitant pathology of the uterus and there is no need to preserve reproductive function, it is possible to perform extrafascial hysterectomy type I (the cervix is removed along the edge of the vagina, the pubovesical-cervical fascia is not separated from the cervix and is removed along with it). - Stage IA2:
- a modified extended extrafascial extirpation of the uterus type II is performed (removal of the obturator, middle group of external iliac lymph nodes and lymph nodes in the area of the bifurcation of the common iliac artery, as well as the upper third of the vagina); - if it is necessary to preserve reproductive function, it is extremely rare, but it is possible to perform wide conization of the cervix with extraperitoneal or laparoscopic pelvic lymphadenectomy or extended trachelectomy (removal of the cervix with parametric tissue and the upper third of the vagina, bilateral pelvic lymphadenectomy and anastomosis between the body of the uterus and the vagina) . — if there are contraindications to surgical treatment, radiation therapy. - IB1 and IIA1 - extended extrafascial extirpation of the uterus type III - Wertheim-Meigs operation (with uterine appendages, upper third of the vagina, iliopelvic lymphadenectomy) or radiation/chemoradiotherapy according to a radical scheme. The choice is determined by the patient’s age and the presence of concomitant pathology. In the presence of metastases in the pelvic lymph nodes, lumbar lymphadenectomy is mandatory. Adjuvant treatment is carried out depending on the presence of progression factors.
- IB2 and IIA2 – 3 treatment options:
- Extended extrafascial hysterectomy type III - Wertheim-Meigs operation (with uterine appendages, upper third of the vagina, iliopelvic lymphadenectomy). In the presence of metastases in the pelvic lymph nodes, lumbar lymphadenectomy is mandatory. Adjuvant treatment is carried out depending on the presence of progression factors.
- Chemoradiation therapy according to a radical regimen.
- The first stage is neoadjuvant chemotherapy with drugs containing platinum, the second stage is the Wertheim-Meigs operation. Adjuvant treatment is carried out depending on the presence of progression factors.
- Stage IIB-IVA – chemoradiotherapy is indicated. In the case of metastatic lesions of the pelvic and/or lumbar lymph nodes, the first step may be to perform extraperitoneal limadenectomy. If technically possible, patients with stage IIB are recommended to undergo surgery both as the first stage of combination treatment and after neoadjuvant chemotherapy. In some patients without the tumor spreading to the pelvic wall, an alternative to chemoradiation treatment may be pelvic exenteration (especially in the presence of fistulas). This intervention is possible for primary stage IVA patients and patients with a central relapse involving the bladder and/or rectum that does not extend to the pelvic wall, in the absence of peritoneal dissemination, regional and distant metastases.
- Stage IVB – palliative therapy.
Features of treatment of cervical cancer
At each stage of the disease, the choice of tactics is determined for each patient by a council of 3 doctors: a surgeon-oncologist, a chemotherapist and a radiologist, taking into account individual characteristics such as age, general condition, and the presence of concomitant pathologies.
If radical surgical treatment is possible, surgery is preferred. For patients of reproductive age, I try to carry out the most organ-preserving treatment; if radiation therapy is necessary, I first perform transposition of the ovaries. It is worth noting that this treatment is performed according to very strict indications and to a limited number of people.
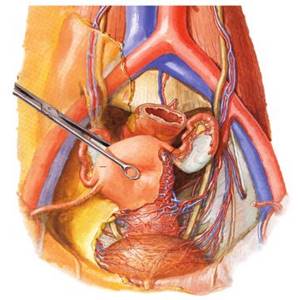
Patients diagnosed with cancer are often depressed, they ask about the prognosis of their disease and are very worried about the upcoming operation. A large volume of surgical intervention, especially if it is performed through a cavity approach (with a wide incision in the anterior abdominal wall) with the installation of drainage tubes, adds physical suffering to the existing psycho-emotional experiences. All this taken together does not speed up the rehabilitation process. Constant work with a large number of such patients has helped me solve problems to improve their quality of life and well-being: I perform surgery using a laparoscopic approach, due to which the patient is activated already on the day of surgery. For maximum and at the same time careful removal of the tissue surrounding the organs, which carries lymphatics nodes and vessels, I use the Thunderbeat device (Olympus, Japan), which combines ultrasonic and bipolar energies, due to which it is possible to achieve a completely dry field. During the operation, I also use other electrosurgical devices, for example, LigaSure (Covidien, Switzerland). The choice of tool depends on the fabric on which the work is currently being done and the tasks at hand. Thanks to laparoscopic access and the use of the most modern equipment, I am able to achieve maximum efficiency, safety and speed of the intervention; there is no need to install drains, as a result, the surgical technique is as gentle as possible, and rehabilitation is accelerated. And of course, all the surrounding medical personnel try to surround patients with care and attention as much as possible, to alleviate their mental suffering, and in cases where patients want to receive professional psychological help, there is always a psychotherapist nearby who will help you get into the right frame of mind. Thanks to an integrated approach - the development of the Fast Track surgery system - rapid recovery surgery - it is possible to reduce the stress reactions of the body and shorten the inpatient stage of treatment.