general characteristics
Phagocytosis is a complex of reactions aimed at recognizing, absorbing and eliminating microscopic particles from the body. Many types of cells are capable of phagocytosis to one degree or another, but the phagocytic activity of neutrophils is of greatest importance for the immune system. In this case, several main stages of the phagocytic process are distinguished: • Adhesion - sticking of cells to microbes. • Absorption of a microbe, forming a phagosome. • Degranulation is the release of special microbicidal factors into the phagosome containing the engulfed microbe. • Oxidative burst – a sharp decrease in pH in the phagolysosome. • Death and degradation of the microbe in the phagolysosome under the influence of microbicidal factors and low pH. Failure in at least one of these stages leads to so-called ineffective phagocytosis. For example, neutrophils can be present in the blood in normal numbers, exhibit full chemotactic and absorption activity, but without killing the absorbed microorganisms. It is possible that in laboratory tests phagocytes demonstrate a high oxidative potential (metabolic reserve), but the process of recognition and absorption of microbes is impaired. The process of cleansing the body of pathogens will not be effective enough even if the concentration of neutrophils in the blood is reduced for some reason. That is why the functional activity of granulocytes should be assessed comprehensively. Our laboratory uses a test system that allows the reaction to be carried out in whole blood, in the presence of serum opsonizing factors, which greatly increases the objectivity of the study. Granulocytes are not subjected to preliminary isolation and washing. In addition, assessing phagocytosis using flow cytometry avoids some of the disadvantages of the traditional smear microscopy method.
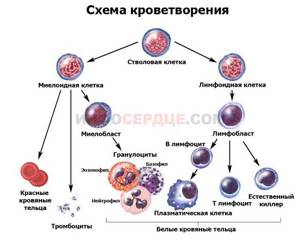
What are leukocytes?
The main granulocytes are neutrophils, otherwise called leukocytes. Their task is to rid the body of the following types of pathogenic microorganisms: viruses, bacteria, parasites. An increase in their number indicates the fight against infections and that the patient should be checked for the listed types of infection.
The infection can also be internal, so without a doctor it will be difficult to find the source of the illness, and in the absence of medical education, you can get confused in terms and definitions. Leukocytes are inhibited and die under the influence of potent drugs. This should be remembered and before taking tests you need to take a break from taking medications.
Also, the number of leukocytes decreases in conditions where a person has blood diseases. The task of white cells is to destroy pathogenic particles by absorption. As a result, the protective bodies die. Before they develop this ability, they undergo a maturation process.
- What do immature granulocytes indicate in a blood test?
White blood cells (neutrophils) are produced in the bone marrow. Some of them are always located in the parietal space of the vessels, the rest constantly wander around the body. Their lifespan is about 7 days in blood fluid. In tissues, the lifespan is reduced and is no more than 2 days.
Patient preparation rules
Standard conditions:
The fasting period is 8 hours (unless otherwise determined by the doctor).
You can drink water. Biomaterial is accepted in accordance with the schedule for taking biomaterial in the ML department of DILA. On the eve of the study, it is necessary to exclude physical activity (sports training) and smoking.
Children under 5 years of age and adults with contraindications for fasting are allowed a light meal of low-fat food at least 2 hours before the BM test. You can add this study to your cart on this page
Types of granulocytes
Granulocytes are divided into neutrophilic, basophilic and eosinophilic depending on how they perceive standard dyes. The size of these cells is 9-12 microns.
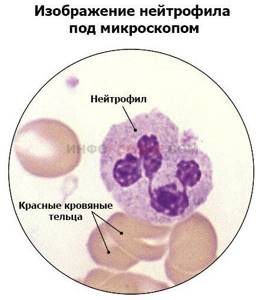
Neutrophils are the most numerous group of granular leukocytes. Their name is due to the fact that according to the Romanovsky method they are stained with both a basic dye and an acidic dye (eosin). Mature neutrophil granulocytes are polymorphonuclear cells because their nucleus consists of four to five segments. In the blood of a healthy person, mainly mature segmented forms and a small number of band granulocytes circulate.
Eosinophils get their name due to the fact that they stain only with an acidic dye (eosin) and do not absorb the basic one. Their core consists of two lobes.

Interpretation:
- High spontaneous activity may indicate a systemic inflammatory process, activation of phagocytes in the peripheral blood.
- Reduced oxidative intensity. Extremely low levels (1/10 or lower of normal) of oxidative intensity after stimulation with E. coli and PMA are a diagnostic marker for myeloperoxidase (MPO) deficiency and chronic granulomatous disease (CGD). For differential diagnosis between MPO deficiency and CGD, an additional examination is necessary - a nitroblue tetrazolium test (NBT test), which will be normal in case of MPO deficiency, and reduced in case of CGD. The intensity of the oxidative burst (stimulation index) depends on the mutation of several enzymes of the NADPH oxidase cascade. If a female patient has two subpopulations of stimulated granulocytes that differ in the intensity of the oxidative burst, this may indicate an X-linked carriage of the deficient chronic granulomatous disease gene CYBB. Minor abnormalities in the dihydrorhodamine test (DHR test) may occur in glucose-6-phosphate dehydrogenase (GP6PD) deficiency and some other phagocytosis defects, but are not specific. If the positive stimulation control (PMA) is positive and the test sample (E. coli stimulation) is negative, then the blood sample most likely contains EDTA or citrate salts as an anticoagulant. It is necessary to retake the BM using the anticoagulant Na-heparin. The DHR test performance can be significantly affected by the use of systemic glucocorticoids, leading to a temporary decrease in its performance. Low phagocytic activity is an indirect indicator of the presence of a phagocytosis defect. It can also be observed when blood transportation is disrupted and a large number of damaged phagocytes accumulate, unable to respond to the stimulus. Low phagocytic activity can occur in sepsis, diabetes and other diseases characterized by general severe intoxication and/or exhaustion.
Sample result (PDF)
Etiology of increased immature granulocytes in the blood
Increased levels of immature granulocytes indicate that pathological processes are developing in the body. The body produces neutrophils in large numbers to protect itself from infection. The reasons for the appearance of immature granulocytes can also be physiological in nature.
So young granulocytes are increased:
- In newborn babies,
- In pregnant women,
- In people in stressful situations,
- After eating,
- In women during menstruation,
- During and for some time after heavy physical activity.
The levels of immature granulocytes are increased, what does this mean?
This means that the patient may have:
- Poisoning or any intoxication (lead),
- Cardiovascular problems (myocardial infarction),
- Burns (thermal, chemical),
- Malignant formations,
- Reactions to vaccination
- Atypical reactions to certain medications
- Blood loss
- Chronic skin pathologies (dermatitis, psoriasis),
- Symptoms of serum sickness,
- Lung infarctions,
- Gangrenous processes,
- Purulent phenomena (abscesses, phlegmons),
- Pneumonia,
- Inflammatory processes (angina, meningitis, cholecystitis, appendicitis, peritonitis, pyelonephritis, osteomyelitis),
- Infectious diseases (hepatitis, typhoid fever, tuberculosis, measles, rubella, influenza).

Granulocytic leukocytes
A sharp shift in the leukocyte formula is determined in myelomonocytic leukemia, as well as in purulent processes. Not only the number of granulocytes changes, but also the “quality” of their cells.
In a child, immature granulocytes in the blood increase when:
- Burns of 3rd and 4th degree of severity,
- Trophic ulcers,
- Leukemia,
- Acidosis,
- Acute infectious infection (otitis media, pneumonia),
- Hemolytic anemia.
What it is?
Granulocytes are blood cells, a subtype of leukocytes with a granular structure. Their nucleus has an irregular shape, and the cells themselves seem to be divided into segments.
Click image for a larger view
They come in two types:
- Mature ones are the basis of “white” blood and are fully functional cells.
- Immature - just released from the bone marrow, are produced in small quantities to replace old forms and in large quantities when there is a shortage of mature cells in the blood or the body's need for leukocytes suddenly increases.
According to their composition, these cells are:
- Neutrophils – 70% of the total composition of granulocytes.
- Eosinophils – 5%.
- Basophils – 1%.
Role in the body
Granulocytes are the body’s “line of defense” against pathologies, infections and foreign deposits.
Depending on their type, they perform different functions, united by a common focus - immune:
| View | Functions |
| Neutrophilic | Produce antimicrobial substances. Absorb and destroy bacteria and infections. Cleanse the body of “foreigners”. |
| Basophilic | Their function is to release biologically active substances from mast cells (degranulation), which leads to increased blood flow and improved vascular permeability. Simply put, their task is to mobilize the remaining granulocytes to the site of inflammation. |
| Eosinophilic | Give the immune system targets to attack. They produce substances against parasites. Absorb excess histamine, releasing it back when necessary. |
When a virus or bacteria enters the body, these blood cells absorb the “foreigner,” usually dying along with it.
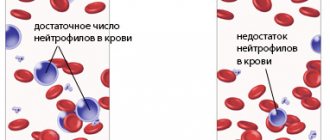
If the infection is too aggressive, then granulocytes die more intensively and there are fewer of them. If a rapid immune response and the participation of a larger number of cells are required, then their relative deficiency occurs. Then, to replenish reserves from the bone marrow, still immature forms are “called upon” to fill the gaps in immune defense.
When immature granulocytes are visible in the analysis in large quantities, this means that the immune system is under the influence of a pathogenic environment - usually this condition is caused by infectious diseases, allergic reactions, inflammatory processes and autoimmune disorders.
Normal blood levels
In a normal healthy state, the relative number of granulocytes in human blood averages:
- Immature - up to 5% of the total number of leukocytes.
- Ripe - 65%.
- When calculating, the level of neutrophils in the blood is taken into account, since they are the most abundant, and a deficiency of this form of granulocytes clearly shows painful processes in the body.
- These numbers are not considered absolute amounts - for many people, the fluctuation in the values of these cells in the analysis falls between 45 and 70 percent.
- The ratio of mature and immature cells in children is slightly different from adult indicators.
- Pregnant women also have a different normal level of granulocytes, due to hormonal changes in the whole body.
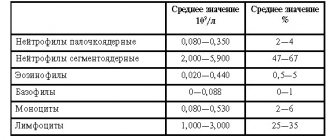
In adult men and women
The number of granulocytes in the analysis can be designated by the letter combination GRA or GRAN.
This indicator is written as a percentage relative to the total number of leukocytes.
The standard for adults has the following designation: 1.2 – 6.8*10 (to the 9th power) per 1 liter (of blood). That is, the norm will be 47-72% of mature granulocytes in the composition.
Immature cells also have their own “threshold” of 1-5% - this is a normal volume if a person is healthy.
There is no difference in quantity between men and women - the leukocyte composition of the blood depends very little on the gender of the person. Only during periods of pregnancy can the percentage of immature cells undergo temporary changes that will be considered part of the normal functioning of the body.
In case of disturbances in the body, the leukocyte formula can undergo either a left shift on the scale or a right shift - up or down:
- A value above 5-6% is considered elevated.
- A value below 1-2% is considered reduced.
In children
Childhood is special, even regarding blood composition. The ratio of norms here is different than in adults.
| Table of quantitative norms of granulocytes in children | ||
| Age | Mature cells (%) | Immature cells (%) – no more |
| Infant under 1 year | From 15 to 30 | 4 |
| Child from 1 to 6 years old | From 25 to 60 | 5 |
| Child from 7 to 12 years old | From 35 to 65 | 5 |
| Teenager from 13 to 15 years old | From 40 to 65 | 6 |
| Teenager 15 years and older | From 45 to 75 | Range 1 to 6 |
These quantitative differences from adult indicators are considered the norm at each specific stage of growing up.
Too low or too high values of granulocytes in a child can be considered a sign of pathology only if, with the transition to a new age group, the abnormal level persists and does not fall within the normal range.
In infants, in the first weeks of life, immature granulocytes are elevated, and are almost never at a low level, unless the child is sick. Such an increase in the norm is considered acceptable, since the newborn experiences the stress of separation from the mother and begins to adapt to the new environment. Over time, there is a decrease to normal age levels.
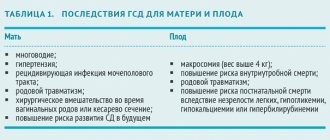
What do pregnant women need to know?
The rate of immature granulocytes in women during pregnancy is usually higher. The production of estrogen affects all body systems and blood composition. Due to such a restructuring, there is a need to increase the number of leukocytes. And along with them, the importance of immature cells also grows.
Typically, this process begins at 30 weeks and is not a sign of pathologies or infections.
Before and during childbirth, the level of granulocytes can also exceed normal values for adults, since the woman’s body is under stress and mobilizes all systems.
How is analysis carried out to determine their level?
The level of granulocytes is detected during clinical collection and testing of blood, which is taken in the standard way - from a finger prick. The procedure must be carried out on an empty stomach and in the morning.
You can take a complete blood count (CBC) in any clinic; the value of granulocytes is prescribed if the doctor asks the laboratory assistant for a “leukocyte formula”.

The procedure is quick and suitable for all age groups - including infants, pregnant women and adolescents. Women, however, are not advised to take the OAC if they are menstruating, as this condition may skew the actual value.
Another group of people whose performance may be distorted are athletes, especially professional ones. Constant loads change the composition of the blood, so the “output” values may be overestimated, although there are no pathologies or infections in the body.
To avoid a “false alarm”, it is necessary to stop training or reduce the intensity of physical activity for 1-2 days before the OAC.
Reasons for increase or decrease
The main reason for the increase in the level of immature granulocytes in the blood is considered to be inflammatory and bacterial processes in the body. The immune system, in order to fight pathogens, requests more neutrophils to eliminate harmful microflora.
The reasons for changes in the number of immature granulocytes in children and adults will be the same.
Factors contributing to increased levels:
- Intoxication of the body (poisoning, insect bites).
- Heavy bleeding.
- Allergy.
- Burn.
- Peritonitis.
- Infections or viruses (flu, scarlet fever, etc.).
- Purulent processes.
- Myocardial infarction.
- Taking certain medications.
- Graft.
- Myeloplastic diseases.
- Otitis.
- Appendicitis.
- Pneumonia.
- Other inflammatory processes.
- Diseases of the blood and hematopoietic system.
Factors contributing to the decrease in level:
- Anemia of various forms and causes.
- Acute leukemia.
- Lead poisoning.
- Autoimmune pathologies.
- Exposure to radiation.
- Thyroid diseases.
- Itsenko-Cushing's disease.
- Taking hormonal drugs.
- The use of chemotherapy drugs in the treatment of cancer.
- Malaria.
- AIDS.
- Hepatitis.
- Alcoholism.
- Diabetes.
- Recent surgeries.
- Polytraumas.
- Aplastic process in the bone marrow.
- Sepsis.