About 7% of all pregnancies are complicated by gestational diabetes mellitus (GDM), which accounts for more than 200 thousand cases worldwide annually [1]. Along with arterial hypertension and premature birth, GDM is one of the most common complications of pregnancy [2].
- Obesity increases the risk of developing gestational diabetes mellitus during pregnancy by at least two times.
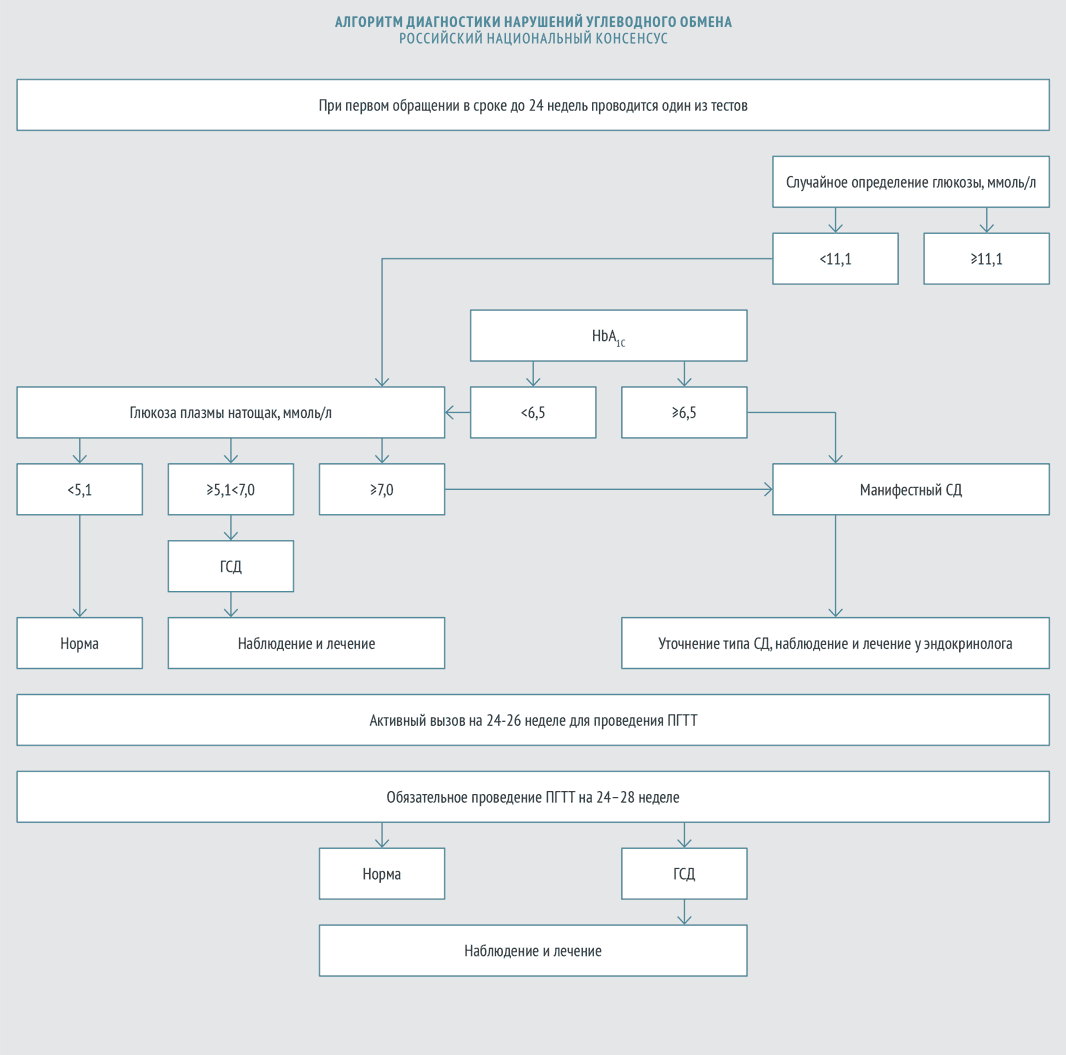
- A glucose tolerance test should be performed on all pregnant women between 24 and 28 weeks of pregnancy.
- If the fasting plasma glucose level exceeds 7 mmol/l, the development of overt diabetes mellitus is indicated.
- Oral hypoglycemic drugs are contraindicated in GDM.
- GDM is not considered an indication for elective cesarean section, much less for early delivery.
Pathophysiology consequences of gestational diabetes mellitus and impact on the fetus
From the earliest stages of pregnancy, the fetus and the developing placenta require large amounts of glucose, which is continuously supplied to the fetus with the help of transporter proteins. In this regard, the utilization of glucose during pregnancy is significantly accelerated, which helps to reduce its level in the blood. Pregnant women tend to develop hypoglycemia between meals and during sleep, since the fetus receives glucose constantly.
What are the dangers of gestational diabetes mellitus during pregnancy for the child and mother:
As pregnancy progresses, tissue sensitivity to insulin steadily decreases, and insulin concentrations increase compensatoryly [3]. In this regard, the basal level of insulin (fasting) increases, as well as the concentration of insulin stimulated using a glucose tolerance test (the first and second phases of the insulin response). As gestational age increases, the elimination of insulin from the bloodstream also increases.
With insufficient insulin production, pregnant women develop gestational diabetes mellitus, which is characterized by increased insulin resistance. In addition, GDM is characterized by an increase in the content of proinsulin in the blood, which indicates a deterioration in the function of pancreatic beta cells.

Description of the analysis for glycated hemoglobin
Glycohemoglobin is present in the blood of any person; the main difference between a healthy person and a sick person is that in a person suffering from diabetes, the amount of this compound greatly exceeds the norm.
Moreover, analysis for glycated hemoglobin allows not only to detect diabetes in the early stages, but also to determine the tendency to develop this disease. Therefore, the test should be carried out even for healthy people at least once a year. This will make it possible to timely detect disturbances in carbohydrate metabolism and apply effective preventive measures, as a result the person will remain healthy and prevent the development of diabetes, which is much more difficult to combat.
It should be taken into account that some congenital pathologies can affect the level of glycosylated hemoglobin. For example, in patients with sickle cell anemia, its amount will be noticeably lower than normal.
The main advantages of the glycohemoglobin test include:
- Can be done at any time, even immediately after eating.
- One of the simplest and fastest tests to diagnose diabetes.
- Serves as a reliable indicator of how the diabetic has controlled sugar levels in the previous 2-3 months.
- The accuracy of the analysis is almost unaffected by extraneous factors (infections, physical activity, alcohol intake).
Thanks to the high reliability of this study, the doctor is able to prescribe appropriate therapy and make the necessary adjustments to treatment regimens in a timely manner. Therefore, patients with an established diagnosis of diabetes mellitus should donate blood for glycosylated hemoglobin every 3-4 months.
Rapid tests to determine this indicator have not yet been developed, so samples are taken only in medical institutions with a referral from the attending physician.
Risk factors for GDM
The risk of developing GDM should be assessed at the first visit of a pregnant woman to an obstetrician-gynecologist regarding pregnancy. There are factors that increase the risk of developing GDM by at least twofold [4], these are:
- overweight and obesity (body mass index (BMI) above 25 kg/m2 and above 30 kg/m2);
- increase in body weight after 18 years by 10 kg;
- the age of the pregnant woman is over 40 years (compared to women aged 25–29 years);
- belonging to the Mongoloid race (compared to the Caucasian race).
In addition, the likelihood of GDM is increased by smoking, a sedentary lifestyle, and a genetic predisposition to type 2 diabetes mellitus (DM). In recent years, information has emerged indicating that short stature may be associated with GDM [5]. Women with impaired glucose tolerance (IGT) are more likely to develop insulin resistance during pregnancy; patients suffering from polycystic ovary syndrome, as well as arterial hypertension [4].
There are also risk factors associated with the course of pregnancy. Thus, the likelihood of developing GDM increases significantly with multiple pregnancies (twice for twins and 4–5 times for triplets), as well as with rapid weight gain during pregnancy. The use of beta-blockers or corticosteroids to prevent the threat of preterm birth increases the risk of GDM by 15–20% or more [4].
Risk factors for GDM associated with obstetric history include:
- GDM in previous pregnancies;
- glucosuria (during current or previous pregnancy);
- history of large fetus and/or hydramnios;
- history of stillbirth.
What should you not do if you have gestational diabetes? With GDM, it is necessary to limit the amount of energy consumed per day. Changes in the diet should be aimed at switching to fractional meals (for example, three main meals and three snacks). Carbohydrates should make up no more than 50% of the diet, with fat and protein 25%.
According to the 2013 American Diabetes Association standards [6], a woman is classified as at high risk of developing GDM if she has at least one of the following criteria: obesity; burdened heredity; history of GDM; glucosuria; history of polycystic ovary syndrome.
A woman is said to be at low risk of developing GDM if she meets all of the following criteria: age under 25 years; normal weight before pregnancy; belonging to an ethnic group with a low likelihood of developing diabetes; absence of first-degree relatives suffering from diabetes; no history of IGT; absence of a burdened obstetric history.
Women who do not fall into the high- and low-risk categories have a moderate risk of developing GDM.
Preparing for the HbA1c test
Many blood tests are recommended to be performed only on an empty stomach.
Glycosylated hemoglobin does not require this condition, since this indicator can be analyzed even after eating. This is because it displays the average glycemic value over 3 months, and not at the time of measurement. The HbA1c result is not affected by:
- snacks;
- taking antibacterial drugs;
- cold;
- mental state of the patient.
Factors contributing to distortion of the result:
- disorders of the thyroid gland that require the use of special hormonal drugs;
- presence of anemia;
- taking vitamins E or C.
The HbA1c level is most often determined by intravenous blood sampling, but in some cases the material for the study is a sample taken from a finger. Each laboratory chooses its own analysis method.
Diagnosis of gestational diabetes mellitus: indicators and norms
In 2012, experts from the Russian Association of Endocrinologists and experts from the Russian Association of Obstetricians and Gynecologists adopted the Russian national consensus “Gestational diabetes mellitus: diagnosis, treatment, postpartum care” (hereinafter referred to as the Russian national consensus). According to this document, GDM is identified as follows:
Management of patients with GDM
Within 1–2 weeks after diagnosis, the patient is advised to be monitored by obstetricians-gynecologists, therapists, and general practitioners.
Rules for conducting an oral glucose tolerance test (OGTT)
- The test is carried out against the background of normal nutrition. At least 150 g of carbohydrates should be consumed per day for at least three days before the study.
- The last meal before the test should contain at least 30–50 g of carbohydrates.
- The test is performed on an empty stomach (8–14 hours after eating).
- Drinking water before the test is not prohibited.
- You are not allowed to smoke during the study.
- The patient must sit during the test.
- If possible, on the eve of and during the study, it is necessary to avoid taking medications that can change blood glucose levels. These include multivitamins and iron supplements, which contain carbohydrates, as well as corticosteroids, beta blockers, beta adrenergic agonists.
- OGTT should not be performed:
- with early toxicosis of pregnant women;
- if necessary, on strict bed rest;
- against the background of an acute inflammatory disease;
- with exacerbation of chronic pancreatitis or resected stomach syndrome.
Recommendations for a pregnant woman with diagnosed GDM according to the Russian national consensus:
- Individual correction of the diet depending on the woman’s body weight and height. It is recommended to completely eliminate easily digestible carbohydrates and limit the amount of fat. Food should be distributed evenly over 4-6 meals. Non-nutritive sweeteners can be used in moderation.
For women with a BMI >30 kg/m2, average daily caloric intake should be reduced by 30–33% (approximately 25 kcal/kg per day). It has been proven that this measure can reduce hyperglycemia and plasma triglyceride levels [12].
- Aerobic physical activity: walking at least 150 minutes per week, swimming.
- Self-monitoring of key indicators:
- glucose level in capillary blood on an empty stomach, before meals and 1 hour after meals;
the level of ketone bodies in urine in the morning on an empty stomach (before bedtime or at night, it is recommended to additionally take carbohydrates in an amount of about 15 g for ketonuria or ketonemia);
- arterial pressure;
- fetal movements;
- body mass.
In addition, the patient is recommended to keep a self-monitoring diary and a food diary.
What does the indicator mean?
Blood contains a large number of different substances that circulate in the human body constantly.
One of the parts of total hemoglobin contained in the blood, and also closely related to glucose, is HbA1c. Its unit of measurement is percentage. Deviation of the indicator from the established target value indicates the presence of health problems. The analysis is carried out in two cases:
- by doctor's direction (if indicated);
- if the patient wishes to independently monitor the indicator, even if there are no obvious signs of the disease.
The HbA1c indicator reflects the average glycemic level over 3 months. The test result can usually be obtained the next day or in the next 3 days, since the production speed depends on the chosen laboratory.
Indications for insulin therapy, recommendations of the Russian national consensus
Sulfonylurea drugs (glibenclamide, glimepiride) penetrate the placental barrier and can have a teratogenic effect, therefore they are not used for GDM.
- Failure to achieve target plasma glucose levels
- Signs of diabetic fetopathy by ultrasound (indirect evidence of chronic hyperglycemia [13])
- Ultrasound signs of diabetic fetopathy:
- large fetus (abdominal diameter greater than or equal to the 75th percentile);
- hepatosplenomegaly;
- cardiomegaly and/or cardiopathy;
- dual-circuit head;
- swelling and thickening of the subcutaneous fat layer;
- thickening of the neck fold;
- newly identified or increasing polyhydramnios with an established diagnosis of GDM (if other causes are excluded).
When prescribing insulin therapy, a pregnant woman is treated jointly by an endocrinologist (therapist) and an obstetrician-gynecologist.