Vaginal discharge and smear are normal
All you can read about in letters from women is about doctors’ enthusiasm for treating leukocytes in the vagina, because there is an opinion that leukocytes are a sign of inflammation. Is it so? Far from it! Leukocytosis plays a huge role in a woman’s reproductive function, including during pregnancy. We'll talk about this a little later.
Amount of vaginal discharge Most women do not know what and how much vaginal discharge should be normal. This leads to the fact that they often try to achieve almost sterility of the vagina, absorbing large amounts of medications, douching, using various chemical solutions, gels, and “ionic” pads. Discomfort due to discharge is often created artificially as a consequence of using too many drugs in the fight against leukocytes, candida, ureaplasma, cocci and bacilli (read an article on this topic about the dangers of douching). Normally, from 1 to 4 ml of vaginal fluid is released during the day, which in most cases is whitish, viscous and without an unpleasant odor. Usually, by the end of the day, the pad on your underwear becomes damp. The color of the discharge can be different shades of white, cream, yellow, pink.
Quality of vaginal discharge Vaginal discharge consists of mucous secretion (1), produced by the glands of the cervical canal, desquamated cells of the integumentary epithelium of the walls of the vagina and cervix (2), microorganisms (3) living in the vagina, and vaginal transudate or effusion (4) from adjacent blood vessels. It is important to understand that the vagina does not have its own glands that produce secretions. During the menstrual cycle, the quantity and quality of discharge changes (monitoring of discharge is used as part of contraception or, conversely, when planning pregnancy). In the first half of the cycle, especially closer to ovulation, the mucous component, a derivative of the cervix, predominates. Before menstruation, the amount of discharge may be minimal, although some women complain of spotting, which may be a manifestation of normality or pathology. Cervical mucus also contains a large number of leukocytes, especially during the period of ovulation, in the second half of the luteal phase of the menstrual cycle, but most of all during pregnancy. Young women often complain of copious mucous discharge - this may be due to the presence of physiological pseudo-erosion (ectopia). This condition does not require treatment, but in rare cases, with severe discomfort, surgical treatment of the cervix is performed, although it is not advisable in nulliparous women.
What determines the number of discharges? What determines the number of discharges? Not only on the day of the menstrual cycle, but also on many other factors. First of all, it depends on the woman’s build. Thin women who lack fat tissue have more discharge, especially during intercourse, and it is more watery. To understand why this phenomenon occurs in thin women, it is important to remember the importance of adipose tissue in the human body. Adipose tissue is involved in the metabolism, including sex hormones (therefore, thin women often experience long menstrual cycles of up to 40 days or more, as well as anovulation). It is important as a depot of many nutrients that the body accumulates in a stressful situation. Adipose tissue is an excellent protective layer between organs and other structural parts of the body. It performs many other functions.
A woman’s reproductive organs are richly supplied with blood vessels, because it is important for nature to ensure the process of reproduction and bearing offspring. If we recall the anatomical location of the vagina and uterus, then in front they are in contact with the posterior wall of the bladder, and in the back - with the anterior wall of the rectum. All these organs are very closely interconnected, both by blood supply and nerve fibers (innervation), as, for example, the eyes, nose and throat are connected. The strong odor can cause watery eyes and throat discomfort. Crying is often accompanied by nasal congestion and the appearance of copious discharge (not only the eyes, but also the nose turn red). There is exactly the same close relationship between the vagina, bladder and rectum. So close that a problem in one organ can lead to a problem in another. Many women know that when the bladder becomes inflamed (cystitis), vaginal discharge increases; dysbiosis of the intestinal flora (which most often occurs due to excessive use of antibiotics) is almost always accompanied by vaginal dysbiosis; sexually transmitted infections often affect not only the vagina and cervix, but also the urethra and anus, primarily due to the structural features of the mucous membrane of these organs. Intense sexual intercourse can lead to cystitis. Sexual activity with constipation is often accompanied by pain in the pelvis. But to prevent these organs from touching too closely to each other, nature took care of protection against friction, against the rapid exchange of extracellular fluid and the spread of infection, as well as to protect the blood vessels and nerves with which this area of the body is abundantly supplied - she “invented » fat layer.
In thin women, especially tall and thin (model type), the fat pad is extremely thin. This causes more blood plasma to leak through the blood vessel wall and into the vagina, forming thin (almost watery) vaginal discharge. During sexual intercourse, when arousal occurs, as well as friction of the penis against the walls of the vagina, blood flow in the vessels of the external and internal genital organs increases, and therefore more of the liquid part of the blood sweats into the vagina. Such women often complain that during sexual intercourse they produce so much “lubricant” that it simply “squishes,” putting the woman in a state of shame and discomfort. Helping women prescribe medications is not easy. Obese women may also have an increased amount of discharge, mainly due to stagnation of blood in the pelvic organs. Constipation is also accompanied by a violation of the vaginal microflora - the discharge becomes yellowish-green, often with an unpleasant odor. Increased physical activity and, conversely, inactivity are accompanied by increased secretions. The amount of discharge is also influenced by the hygiene of the external genitalia, the use of chemical solutions for intimate hygiene (not all intimate gels are natural), synthetic sanitary pads (almost all pads increase discharge), synthetic washing powders and liquids, wearing synthetic underwear and tights jeans and pants.
Methods for examining vaginal discharge Vaginal contents can be examined using various methods. The most common are: • Microscopic examination of a smear (fresh native unstained, stained) - most often such a study is carried out poorly due to the imposition of too much secretion on the glass. • Cytological smear (study of integumentary epithelial cells) - used as a screening for precancerous and cancerous conditions of the cervix. • Determination of acid-base balance (pH) - this type of study is simple and informative, but almost forgotten by many doctors. • Isolation of culture (bacterial inoculation using various media) - most often carried out incorrectly with contamination of the inoculum by microorganisms of the perineum and vaginal vestibule. • Immunological research (PCR, etc.) - such methods are carried out on a commercial basis, so they began to be abused, ignoring cheaper examination methods.
Vaginal microflora Vaginal microflora represents certain types of microorganisms (bacteria, viruses, fungi, etc.) that live in the vagina or were introduced there in various ways (trauma, foreign body, surgery, sexual intercourse, etc.) It is important to understand that the perineal area is the dirtiest part of the skin of the human body. During the act of defecation, billions of microorganisms come out along with feces. The skin around the anus is always contaminated with a large number of bacteria, the so-called intestinal group. This is the norm of life, even if it is accompanied by an unpleasant odor and discharge accumulated between the legs by the end of the day.
Factors influencing the microflora of the vagina The bacterial flora of the vagina of women depends on the following factors: • Pregnancy (candidiasis is a physiological norm of pregnancy) • Age • Hormonal levels • Acid-base balance of the vaginal environment (pH) • Number of sexual partners • Smoking • Menstrual cycle • Method of contraception • Presence of infectious diseases • Presence of certain common diseases (for example, diabetes) • Taking medications • Douching • Frequency of sexual intercourse
Bacteria living in the vagina Traditionally, many years ago, it was believed that the main inhabitants of the vagina should only be Dederlein bacilli from the group of lactobacilli. But with the development of microbiology, scientists have come to the conclusion that up to 100 species of microorganisms can live in a woman’s vagina (mostly up to 5 in one woman), most often from the opportunistic group. Opportunistic pathogens are bacteria, viruses, fungi and protozoa that live in the human body without causing harm, but under certain conditions (decreased defenses, chronic diseases, anticancer therapy, etc.) can lead to an inflammatory process. The role of most microorganisms living on the surface and inside the human body has not yet been fully studied and is not entirely understood. Thus, in more than 50% of healthy women, such vaginal flora is considered normal.
The most common microorganisms in vaginal contents are the following bacteria: • Atopobium vaginae • Bacteroides sp. • Candida • Corynebacteria • Enterococcus faecalis • Esherichia coli • Lactobacillus • Leptotrichia • Megasphaera • Mycoplasma • Neisseria meningitis • Neisseria sp. • Proteus spp. • Staphylococcus aureus • Staphylococcus epidermidis • Streptococcus mitis • Streptococcus pneumoniae • Streptococcus pyogenes • Ureaplasma
Most of these microorganisms are representatives of the normal flora of the intestines and perineal skin. There is still some debate among doctors about whether all these types of bacteria and other microorganisms should be considered normal or opportunistic vaginal flora. After all, they can live in the vagina for a long period of life without causing disease. Each woman can have her own individual set of microorganisms, so the old “norms” of vaginal contents have long been no longer used by doctors in most countries of the world. The definition of “normal” flora takes into account the presence of complaints and the absence of signs of infectious diseases.
Dynamics of changes in the vaginal flora With the birth of a child, his contact with the outside world (air, water, objects, people) leads to the fact that the child’s body is quickly populated by different types of bacteria, viruses, fungi and protozoa, mainly living on the skin of the perineum, buttocks, pubis, which in most cases are completely safe for the child. Most often these are corynobacteria, staphylococci, non-purulent streptococci, Escherichia coli and partly Dederlein's bacilli (lactobacteria). It is a mistake to look for lactobacilli in bacterial cultures of secretions and microscopic smears in a girl and be horrified when bacteria of the intestinal group are detected. Lactobacilli appear in a girl’s vagina with the onset of menstruation. With growth and the period of maturation, as well as under the influence of various factors, some types of bacteria are replaced (suppressed) by other types of bacteria. Even with strict adherence to body hygiene, under certain conditions (defecation, sexual intercourse, taking antibiotics), various microorganisms constantly enter the woman’s vagina. The vaginal flora normalizes quickly without additional intervention, usually within 24 hours.
Lactobacilli of the vagina For a long period it was believed that lactobacilli are the only “healthy”, that is, beneficial, bacteria that live in the vagina and normalize the vaginal environment. However, scientists later discovered that 10-42% of healthy women do not have lactobacilli or their number is small. Thus, the concept of the “vaginal ecosystem” was created, which includes many factors, including opportunistic microorganisms, to maintain its balance. There are about 135 species of lactobacilli that can live in a woman's vagina. The name "lactobacillus" comes from the ability of these types of microorganisms to convert lactose (sugar) into lactic acid. Typically, the vagina is home to one to several species of lactobacilli. All lactobacilli are divided into three groups according to their dominant function (some species can perform several functions): (1) species that produce hydrogen peroxide - L. acidophilus, L. crispatus, L. gasseri, L. johnsonii, L. vaginalis; (2) species that produce lactic acid - L. salivarius, L. johnsonii, L. acidophilus, L. jensenii; (3) species that attach to bacterial cells of the vaginal epithelium - L. agilis, L. jensenii, L. Johnsonii, L. ruminus. Hydrogen peroxide acts as a destructive factor directly on pathogenic bacteria and fungi of the vagina, lactic acid creates an acidic environment, which also has a detrimental effect on bacteria, and the attachment (adhesion) of lactobacilli to pathogenic microorganisms (Escherichia coli and other intestinal bacteria) limits the spread of infection in the vagina and beyond.
Triad: intestines, vagina, bladder Dr. Elena Berezovskaya
Lactobacilli do not inhibit the growth of yeast fungi . They stimulate the body's immune system and ensure a normal balance of vaginal flora, preventing the excessive growth of other 20-30 types of opportunistic bacteria that normally live in the vagina in small quantities. Most textbooks and articles from the past on women's health state that the dominant lactobacilli in the vagina are Lactobacillus acidophilus - acidophilus lactobacilli. However, this is a misconception because numerous clinical studies have shown that the most common types of lactobacilli found in the vagina are L. fermentum, L. crispatus, L. jensenii and L. johnsonii. This explains the ineffectiveness of the use of commercial lactobacilli preparations to treat a number of vaginal infections and restore normal flora - all of these preparations contain lactobacilli acidophilus.
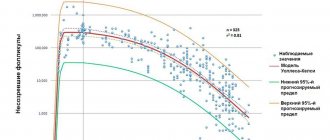
Leukocytes and the reproductive system There are many misconceptions among doctors about how many white blood cells (leukocytes) should be in the vaginal contents. Errors begin with incorrect sampling of the test material. Most often, doctors apply copious amounts of secretions to glass and smear these secretions over the surface of the glass, but the results of such studies are extremely uninformative. Vaginal smears should not be thick in consistency, and smearing the contents on the glass with several movements is strictly not recommended, since this destroys the epithelial cells. Any smears from different points of the vagina and cervix should be taken with separate instruments.
Leukocytes and a woman’s reproductive system are inseparable. This is far from a sign of an inflammatory process, but a dynamic process that is observed in the body of women, and this process completely depends on the hormonal background. The number, as well as the type of leukocytes, changes depending on the day of the menstrual cycle. Physiological leukocytosis is observed before ovulation and in the second half of the cycle, especially before menstruation. During pregnancy, leukocytosis is an integral and necessary condition, without which pregnancy will not proceed normally. Leukocytes are present in vaginal secretions, since they are formed from the liquid part of the blood that has leaked through the wall of the vagina and adjacent vessels and migrating leukocytes. Without exception, all types of leukocytes can penetrate the capillary wall. Also, cervical mucus is a depot of leukocytes, the number of which depends on hormonal levels. During pregnancy, a dense cervical plug forms from white blood cells and mucus from the cervical canal (which is why it is white in appearance). In most cases, microscopy of cervical canal secretions is not recommended.
Dr. Elena Berezovskaya - About leukocytosis
The endometrium also contains different leukocytes: T and B lymphocytes, macrophages, neutrophils and a number of others . It contains a unique type of white blood cells - uterine natural killer cells (uNK) , which appear at the end of the luteal phase and at the beginning of pregnancy. Without a sufficient number of these leukocytes, implantation, placentation and pregnancy are impossible . Unlike other natural killer cells, uterine NKs have a specific structure and are sensitive to hormonal fluctuations, so their number completely depends on the level of sex hormones and progesterone. Since an increase in leukocytes is observed in the endometrium at the beginning of menstruation, the amount of human leukocyte antigen class 1 (HLA or HLA 1) increases, which is normal, especially on the surface of endometrial stromal cells. This antigen plays a very important role. MNA leukocytes participate in the process of death and rejection of the endometrium and help in the splitting (lysis) of exfoliated cells - without this, menstruation is impossible. But they can also lead to lysis of the basal layer of the endometrium and stroma. However, this does not happen in nature, because human leukocyte antigen binds to this type of leukocyte and protects the stroma and basal endometrium from damage. Uterine prolactin stimulates the production of lymphocytes .
Neutrophils are present in endometrial tissue in small numbers throughout almost the entire menstrual cycle, but a few days before the onset of menstruation, their number increases significantly and they dominate the entire period of menstrual bleeding. It is believed that it is the rapid decrease in progesterone levels from the second half of the luteal phase that is the trigger for the appearance of a large number of leukocytes in the reproductive organs. The main neutrophils of the uterus are polymorphonuclear leukocytes (PMNs). In all textbooks and publications you can find that this type of leukocyte appears at the site of inflammation. Indeed, based on the number of these types of leukocytes and their ratio to squamous epithelial cells in vaginal discharge, an inflammatory process can be suspected . Leukocyte counts should be carried out in relation to the number of epithelial cells detected. Normally, the ratio is up to 10 leukocytes per epithelial cell. But in reality, this indicator is not determined or taken into account by most post-Soviet laboratories, and the results indicate the total number of leukocytes in the field of view, and the count is rough and inaccurate (for example, 50-100 leukocytes in the field of view). What is the role of PMNs in the vagina, uterine cavity and endometrium if there is actually no inflammation? This type of leukocyte is involved not only in the fight against the inflammatory process, absorbing (phagocytosing) microorganisms, but also dead cells and tissue scraps. During menstruation, a large number of endometrial cells die, and it also mixes with blood, creating an excellent breeding ground for microorganisms that can enter the uterine cavity from the vagina. Neutrophils become orderlies, cleaning the surface of the area where the old endometrium has been rejected from its remains and prevents bacteria, viruses, and fungi from entering the endometrial and uterine tissue.
Another type of leukocyte, macrophages, also play an important role in the function of the endometrium. They make up up to 20% of all leukocytes appearing in the uterus by the end of the luteal phase, including in vaginal discharge. Although macrophages do not have progesterone and estrogen receptors, their number in the endometrium and other tissues of the genital tract depends on the level of hormones and the day of the menstrual cycle. Macrophages contain enzymes that break down dead endometrial cells; they also produce a number of organic substances that are important in the processes of tissue regeneration (repair).
10% of women experience a large number of white blood cells in vaginal discharge over a long period of life. Treatment with antibiotics, antimicrobials, and douching usually does not change the smear pattern, so most doctors recommend observing such women without treatment. Thus, leukocytosis in any form is a very important stage in the physiological norm of a woman’s menstrual cycle.
Red blood cells in the vagina Normally, a smear of vaginal discharge may contain single red blood cells. Before and after menstruation, the number of red blood cells may be increased, so examination of vaginal discharge is recommended after the complete cessation of menstrual bleeding. When taking a smear roughly with an instrument with sharp edges, the microvessels of the cervix and vagina are damaged, which will affect the quality of the smear and may be the cause of a large number of red blood cells in the test material.
Epithelial cells of the vagina The walls of the vagina are covered with squamous epithelium, which is constantly renewed. Therefore, squamous epithelial cells must be present in the vaginal contents. In women with low estrogen levels and high androgen levels, the number of epithelial cells is reduced. If there are a large number of squamous epithelial cells, it is always necessary to conduct an additional examination to exclude an inflammatory process.
pH of vaginal contents Normally, most women have a pH of 4.0-4.5. The acid-base balance may change depending on the day of the menstrual cycle, as well as under the influence of other factors. Determining the acid-base balance of vaginal discharge is an important diagnostic method in differentiating vaginal dysbiosis, candidiasis, trichomoniasis and normal discharge.
Hygiene of the external genitalia Body hygiene is the key to health, including the vagina and vaginal discharge. Once upon a time in the recent past, hygiene of the external genitalia was almost absent. Only the aristocracy could afford special devices in toilets for women - bidets. There was no toilet paper (as, indeed, there was no underwear for a long period), so the women washed themselves after each urination and defecation, and dried themselves with towels. Modern women prefer toilet paper, but it is important to remember that hand movements after defecation should always be from the vagina towards the anus and the intergluteal fold posteriorly, and not vice versa. After urination, on the contrary, the movements should be from the vagina to the pubis. Before and after sexual intercourse, it is necessary to wash yourself with warm water and soap - this is the prevention of many inflammatory processes of the reproductive system and pelvic organs. A separate article will be devoted to the topic of hygiene of the external genitalia.
Dr. Elena Berezovskaya - About colpitis, cervicitis, etc.
Share link:
- Click to share on WhatsApp (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Skype (Opens in new window)
- Send this to a friend (Opens in new window)
- Click to print (Opens in new window)
By
How to properly perform cervical cytology?
Cytological examination of cervical smears is carried out by a gynecologist directly upon examination of the patient. The doctor carefully examines the woman's vagina using miniature mirrors. Next, he examines the cervical canal and cervical mucosa. Biological material is collected by the doctor directly from the vagina, cervical canal and the entrance to the cervix.
The material remaining on the brush is carefully distributed over a glass slide, dried and transferred to the laboratory, where it will be studied. For analysis, laboratory assistants will stain the smear with special preparations and carefully examine it under a microscope.
Laboratory technicians conducting the analysis are concerned about such characteristics of the material being studied as the size of the cells, their number and location.
After the test, the patient does not have to stay in the clinic. She can return to her daily duties outside. However, young specialists sometimes touch blood vessels, and in this case the patient will have to put up with pain in the perineum and bleeding for 1-2 days.
Advantages of the cytological method:
- absolutely harmless to the patient
- painlessness
- possibility of using multiple cytological studies
- rapidity
- diagnosis of malignant tumors of any location and at any stage of the process.
The study usually takes several hours to complete. Intraoperative cytological examination can be performed within 10 minutes.
Due to its harmlessness, the cytological method is indispensable for assessing the dynamics of morphological changes in tumor cells during treatment and for determining the therapeutic effect of the treatment. For such patients, it has undoubted advantages over other, more invasive research methods.
Cytological research methods are constantly being improved. The development of endoscopic technology makes it possible to purposefully obtain material for research from internal organs that were previously inaccessible for morphological analysis without surgical intervention.
Thus, cytological examination, due to the combination of high information content, harmlessness to the patient and speed, in the absence of tissue trauma, is of great importance in oncology.
What is the difference between cytology and histological examination?
The difference between a cytological study and a histological one, first of all, is that it is the cells that are studied, and not tissue sections. For histological examination, either surgical material or material collection by trephine biopsy is required. For a cytological examination, a smear from the mucous membrane, a scraping from the surface of the tumor, or material obtained with a thin needle is sufficient.
Preparing a histological specimen requires more effort and time than preparing for cytological analysis.