Despite the fact that humanity learned about cholesterol back in the 18th century, people began to actively talk about it in the late 90s. With the advent of the joke that lard is pure cholesterol from a slaughtered animal, we began to associate this term with something bad or a direct threat to our health. Today, we often hear “I have high cholesterol” or “I need to get my cholesterol checked.” Let's try to figure out what cholesterol is and whether we should be afraid of it.
Cholesterol is a fat-like substance that we need to:
- Creation of healthy cells (red blood cell membranes, liver cell membranes, brain (gray and white matter)
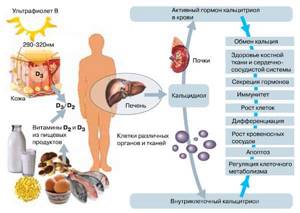
- Normal digestion (cholesterol is needed for the production of cholic or bile acids, which break down fat and fat-soluble vitamins (for example vitamin D)
- Synthesis of hormones (testosterone, estrogen, progesterone and even cortisol)
- Vitamin D synthesis
- The work of the immune, reproductive, nervous systems and generally normal functioning of the body.
Where does cholesterol come from?
Sources of cholesterol are partly the foods we consume (about 20% of the total amount of cholesterol in the body). But the main percentage of the substance is synthesized in the liver, which is responsible for producing 80% of endogenous cholesterol. Other sites of synthesis, but to a much lesser extent, are the adrenal cortex, testes, ovaries and intestines.
The liver synthesizes cholesterol for export to other cells and also helps remove excess cholesterol from the body. This is achieved by converting cholesterol into bile salts and transporting it into bile, from which it is ultimately excreted. In addition, the liver synthesizes most of the essential lipoproteins needed to transport cholesterol throughout the body. Since cholesterol is transported through the blood, but having a fat-like structure, it does not dissolve in it, but attaches to proteins that act as its carriers. The combination of proteins and cholesterol is called lipoproteins.
Lipid synthesis and destruction
During the digestion process, we consume fats, proteins and carbohydrates. The main place of collection and subsequent processing of fats is the liver. It produces lipoproteins and cholesterol. All cholesterol that is not used by cells returns to the liver and is processed again. If these metabolic processes are in balance, the walls of the arteries remain clean and elastic; if these metabolic processes are disturbed, the level of lipids in the blood changes, the walls of the arteries are damaged and lose their smoothness and elasticity.
High-density lipoproteins (HDL) and low-density lipoproteins (LDL) or “bad” and “good cholesterol”
There are several important types of lipoproteins responsible for the movement of cholesterol. The main ones are:
- Low-density lipoproteins ( LDL ), which move cholesterol from the liver to other cells in the body. They are often called " bad cholesterol" . They carry cholesterol particles throughout the body and can accumulate on the walls of damaged blood vessels, making them less elastic and narrowed.
- High-density lipoprotein ( HDL ) or " good" cholesterol , which absorbs excess cholesterol in the body and transports it to the liver for excretion in bile. These lipoproteins are highly soluble and do not tend to precipitate cholesterol on the walls of blood vessels (that is, they do not contribute to the formation of atherogenic plaques).
Often, when people talk about high cholesterol, they mean elevated levels of low- and very low-density lipoprotein cholesterol (LDL-C). When LDL increase, your risk of heart disease increases.
| Low-density lipoprotein cholesterol (LDL) or "bad cholesterol" | High-density lipoprotein (HDL) cholesterol or good cholesterol | Very low density lipoprotein cholesterol (pre-beta lipoproteins), triglycerides |
|
|
|
Controlling your bad cholesterol levels is an important part of reducing your risk of heart disease, heart attack or stroke.
When cholesterol levels rise, fatty deposits can develop in the blood vessels. Over time, these deposits grow, making it difficult for enough blood to pass through the arteries. Sometimes these deposits can suddenly break away and form a clot that causes a heart attack or stroke by traveling through the bloodstream to the heart or brain.
Where do lipids come from in our blood?
95% of all the fats we eat are triglycerides (TG). The remaining 5% comes from phospholipids, free fatty acids, fat-soluble vitamins and cholesterol. Lipids are needed by the cells of our body to produce energy - 1 g. lipids generates 9 calories, and 1 g. proteins or carbohydrates only 4 kcal. And for many other purposes, for example, for the production of hormones, the synthesis of cell membranes, and the synthesis of bile acids.
Lipids enter the blood from two sources: from food and during metabolism in the liver and adipose tissue. They circulate in the blood not on their own, but with the help of carriers - lipoproteins. Our body needs different types of lipids to function normally.
Triglycerides are a special type of fat that we consume along with food, which is used to produce and maintain energy, or are stored in adipose tissue. Triglycerides are also the main raw material for the production of cholesterol in the liver.
Cholesterol
Cholesterol is necessary for the synthesis of bile, and we need bile for digestion. Cholesterol is also used for the synthesis of certain hormones and for the construction of cell membranes. Cholesterol is almost entirely produced in the liver, but small amounts reach us through food of animal origin. Plant foods do not contain cholesterol.
Lipoproteins
Lipids are fat-soluble organic substances. They do not dissolve in water, and therefore in blood. In order to circulate in the blood and reach organs and cells, fats must bind to special carriers - lipoproteins. The protein shell of lipoproteins reliably protects the lipids contained in it, like a shell stores its pearl, and also helps lipids get into those cells where these lipids are needed, opening them like a key opens a lock.
The main types of lipoproteins are:
| VLDL – very low density lipoproteins | LDL – low density lipoproteins | HDL – high density lipoproteins |
| Major triglyceride transporters. Transport triglycerides to places of their storage and use. In a small part, they are also responsible for the transport of cholesterol. | The main carriers of cholesterol to the cells of the body. LDL cholesterol is often called “bad” cholesterol, as it can be deposited on the walls of arteries, which leads to a narrowing of their lumen and obstruction of blood flow. | HDL consists mainly of protein shells. The cholesterol they contain is referred to as HDL cholesterol and is conventionally considered “good” cholesterol. They help remove excess cholesterol from the bloodstream. |
Heredity or inherited high cholesterol
High cholesterol can often run in families and can only be diagnosed through laboratory tests as a result of a heart attack or stroke. Tell your doctor right away if anyone in your family has had these conditions, especially at a young age, and consider getting tested.
Familial hypercholesterolemia is an inherited disorder that causes atypically high levels of low-density lipoprotein cholesterol (LDL-C). With this disease, the liver is not able to utilize the natural supply of cholesterol, which is constantly being produced. As a result, cholesterol becomes dangerously overabundant, which dramatically increases the risk of atherosclerotic plaque deposits and the development of coronary heart disease (lack of oxygen reaching the heart due to vasoconstriction). Imagine faulty waste disposal through a garbage chute. Every night you have to throw out new trash and spoiled food, but previous waste has already clogged the pipes. As you may have guessed, this will soon lead to disaster. If your liver doesn't filter and process LDL cholesterol properly, it's not much different from improperly disposing of garbage. The vessels suffer the most due to the deposits of cholesterol plaques; they narrow and have less elasticity.
Possible causes of decreased cholesterol levels
Fatty alcohol or cholesterol is another name for the well-known cholesterol. The mechanism for reducing its concentration in the body has been poorly studied, but based on the available data, the following conclusions can be drawn. Experts call the probable causes of the pathology:
- Severe liver diseases. It is this organ that synthesizes up to 80% of the total amount of cholesterol, so liver diseases lead to a drop in its level.
- Irrational diet. We are talking about ignoring foods containing fats and preferring foods with fast carbohydrates.
- Vitamin deficiencies. Deficiency of substances necessary for the body due to starvation, severe infectious diseases, anorexia.
- Prolonged state of stress. Adrenaline, produced during nervous overload, is an antagonist of fatty alcohols.
- Pathologies of the thyroid gland. For example, hyperthyroidism is accompanied by severe disruption of the production and balance of essential hormones. Changes in hormonal levels are another reason for the decrease in its concentration in the blood.
- Taking drugs that suppress the synthesis of fatty alcohols. Inadequate dosage of statins, fibrates, and nicotinic acid can lead to an excessive reduction.
In addition, prolonged febrile states caused by infectious diseases (tuberculosis, pneumonia) or injuries are recognized as provoking hypocholesterolemia. Unfavorable factors of occurrence also include anemia or hereditary abnormalities, often associated with liver dysfunction.
In women, changes in blood cholesterol concentrations often occur during pregnancy. Especially if it is complicated by a relapse of chronic diseases.
Symptoms of High Cholesterol
Sometimes cholesterol is deposited on the surface of the skin (in the form of plaques on the skin of the face, lower eyelids, limbs and torso, but the most dangerous deposits of cholesterol are inside our body, which are not visible. Often, high levels of low-density cholesterol in the body have no symptoms. And in In most cases, the disease remains undetected in time, which can lead to a heart attack, myocardial infarction, stroke at an early age, as well as problems with atherosclerosis.
Cholesterol and lipid profile tests
Lipid profile measures:
- total cholesterol;
- cholesterol associated with HDL ( high-density lipoprotein or alpha lipoprotein ), which can reduce or inhibit the increase in “bad” cholesterol in the blood);
- olesterol of very low density lipoproteins (pre-beta lipoproteins which are the main transport form of triglycerides . They are classified as highly atherogenic lipoproteins involved in the mechanism of formation of atherosclerotic plaques;
- olesterol carried by LDL particles ( low -density lipoproteins, beta lipoproteins ), that is, bad cholesterol, which contributes to vascular disease);
You can take these basic indicators separately or order a more extensive lipid profile analysis using the 112 lipid complex or 113 extended lipid complex , which include additional studies
- Triglyceride levels;
- Atherogenic index;
- Presence of Apolipoprotein – A 1, Apolipoprotein – B;
- Lipoprotein (a) - additional factors in the development of atherosclerosis;
How to decipher a blood test
You can find out whether total cholesterol is elevated by conducting a blood test in the laboratory. If total cholesterol is elevated, what does this mean, how to act, and everything about treatment will be explained by your doctor. But you can try to decipher the test results yourself. To do this, you need to know that the biochemical analysis contains three indicators: LDL cholesterol, HDL cholesterol and total cholesterol.
A lipidogram is a comprehensive study that allows you to evaluate lipid metabolism in the body, which allows you to determine how lipid metabolism occurs and calculate the risk of atherosclerosis and coronary artery disease.
Correct interpretation of the blood lipid profile is also important from the point of view of assessing the need to take statins and the daily dose of such drugs. Statins are drugs that have many side effects, and their price is quite high. Therefore, based on what it is - a lipid profile, this analysis allows you to find out what a person’s blood consists of and prescribe the most effective therapy for the patient.
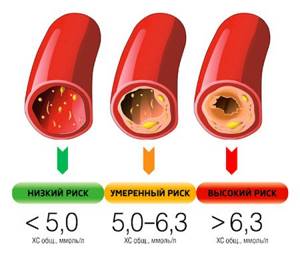
Cholesterol levels and the development of vascular atherosclerosis
After all, total cholesterol is an indicator that in itself does not make it possible to clearly assess the likelihood of a patient developing atherosclerosis. If total cholesterol is elevated, what to do can be assessed using the full range of diagnostic indicators. Therefore, the following indicators are determined:
- HDL (alpha cholesterol) - determines whether high-density lipoproteins are increased or decreased. It is taken into account when determining the parameters of β-lipoproteins that this substance performs a protective function, preventing the development of atherosclerosis.
- LDL - low-density lipoproteins are increased or decreased. The higher the beta cholesterol level, the more activated the atherosclerotic process.
- VLDL are very low-density lipoproteins, thanks to which exogenous lipids are transported in plasma. Synthesized by the liver, they are the main precursor of LDL. VLDL takes an active part in the production of atherosclerotic plaques.
- Triglycerides are esters of higher fatty acids and glycerol. This is a transport form of fats, therefore, their increased content also increases the risk of atherosclerosis.
What normal cholesterol should be is determined depending on age; it can be different for women and men. In addition, it is important to understand that there is no exact number that indicates the norm of cholesterol. There are only recommendations on what the index should be. Therefore, if the indicator is different and deviates from the range, then this is evidence of some kind of disease.
However, those who are planning to take the test should take into account that certain errors may occur during the analysis. The data from the study showed that in 75% of laboratories in the country such errors are allowed. What to do if you strive to get an accurate result? It is best to do such analyzes in those laboratories that are certified by the VCS (Invitro, etc.)
Normal cholesterol levels in women
- Normally, in women, total cholesterol is: 3.6 - 5.2 mmol/l;
- hn, moderately elevated: 5.2 - 6.19 mmol/l;
- hn, significantly increased: more than 6.19 mmol/l.
- LDL cholesterol: normal – 3.5 mmol/l, elevated – from 4.0 mmol/l.
- h-HDL: the normal level is 0.9-1.9 mmol/l, a level below 0.78 mmol/l is considered dangerous to health.
| № | Age (years) | Total cholesterol (mmol/l) |
| 1 | under 5 | within 2.90-5.18 |
| 2 | 5-10 | within 2.26-5.30 |
| 3 | 10-15 | within 3.21-5.20 |
| 4 | 15-20 | within 3.08-5.18 |
| 5 | 20-25 | within 3.16-5.59 |
| 6 | 25-30 | within 3.32-5.75 |
| 7 | 30-35 | within 3.37-5.96 |
| 8 | 35-40 | within 3.63-6.27 |
| 9 | 40-45 | within 3.81-6.53 |
| 10 | 45-50 | within 3.94-6.86 |
| 11 | 50-55 | within 4.20-7.38 |
| 12 | 55-60 | within 4.45-7.77 |
| 13 | 60-65 | within 4.45-7.69 |
| 14 | 65-70 | within 4.43-7.85 |
| 15 | from 70 | within 4.48-7.25 |
Normal cholesterol levels in men
- Normal total cholesterol in men is: 3.6 - 5.2 mmol/l;
- LDL cholesterol: normal – 2.25 – 4.82 mmol/l;
- h-HDL: normal value - 0.7 - 1.7 mmol/l.
| № | Age (years) | Total cholesterol (mmol/l) |
| 1 | up to 5 | within 2.95-5.25 |
| 2 | 5-10 | within 3.13-5.25 |
| 3 | 10-15 | within 3.08-5.23 |
| 4 | 15-20 | within 2.93-5.10 |
| 5 | 20-25 | within 3.16-5.59 |
| 6 | 25-30 | within 3.44-6.32 |
| 7 | 30-35 | within 3.57-6.58 |
| 8 | 35-40 | within 3.78-6.99 |
| 9 | 40-45 | within 3.91-6.94 |
| 10 | 45-50 | within 4.09-7.15 |
| 11 | 50-55 | within 4.09-7.17 |
| 12 | 55-60 | within 4.04-7.15 |
| 13 | 60-65 | within 4.12-7.15 |
| 14 | 65-70 | within 4.09-7.10 |
| 15 | from 70 | within 3.73-6.86 |
Triglycerides
Triglycerides are a certain type of fat that is found in human blood. They are the main source of energy and the most abundant type of fat in the body. A complete blood test determines the amount of triglycerides. If it is normal, then these fats are beneficial for the body.
As a rule, triglycerides in the blood are elevated in those who consume more calories than they burn. When their levels are elevated, the so-called metabolic syndrome , in which there is high blood pressure, increased blood sugar, a low content of good henna, and also a large amount of fat around the waist. This condition increases the likelihood of developing diabetes, stroke, and heart disease.
The normal triglyceride level is 150 mg/dl. The normal level of triglycerides in the blood of women, as well as men, is exceeded if the level is more than 200 mg/dl. However, the rate is up to 400 mg/dl. is designated as acceptable. A high level is considered to be 400-1000 mg/dl. very high – from 1000 mg/dl.
If triglycerides are low, what does this mean, you need to ask your doctor. This condition is observed in lung diseases, hyperthyroidism , cerebral infarction, parenchymal damage, myasthenia gravis, when taking vitamin C , etc.
When is it recommended to get tested for cholesterol?
Young people without risk factors for cardiovascular disease are usually tested once between the ages of 17 and 19. Repeat testing for adults without risk factors for heart disease is usually done every five years.
The American Heart Association recommends cholesterol testing every 4 to 6 years for people age 20 and older.
Patients taking medications for high cholesterol, such as statins, should have their cholesterol levels checked as directed by their doctor or 4 to 12 weeks after the first dose and then every 3 to 12 months thereafter. It is recommended to test your cholesterol levels at least once every five years if a person has a total cholesterol level of 5.2 mmol or there are prerequisites for the development of cardiovascular diseases and stroke. Additional causes of possible heart disease include diabetes, high blood pressure or use of antihypertensive medications), low HDL levels, a family history of coronary artery disease (CHD) and hypercholesterolemia, and cigarette smoking.
Complexes with this research
Fitness monitoring Examination to select physical activity and monitor the state of the body RUR 4,970 Composition
Nutritionist recommends Metabolic status assessment RUR 5,640 Composition
Preventive check-up Universal annual preventive screening 8,710 RUR Composition
IN OTHER COMPLEXES
- Male anti-aging diagnostics RUB 10,140
- Metabolic profile RUR 4,740
- Anti-aging diagnostics in postmenopause RUB 9,620
- Advanced women's anti-aging diagnostics RUB 22,900
- Monitoring the diet of a nursing mother RUB 2,250
Risk factors for having high cholesterol include:
- Eating an unbalanced diet, consuming saturated fat found in animal products and trans fat found in some cookies, sauces, crackers and even popcorn, red meat, and full-fat dairy products can increase cholesterol levels;
- Obesity. Having a body mass index (BMI) of 30 or higher increases your risk of high cholesterol;
- Lack of exercise. Exercise helps raise HDL, or “good” cholesterol;
- Smoking. Smoking cigarettes damages the walls of blood vessels, making them more prone to the accumulation of fatty deposits. Smoking can also lower your HDL or “good” cholesterol levels;
- Elderly age. As chemical processes change with age, the risk of high cholesterol increases. For example, as we age, the liver becomes less able to remove LDL cholesterol;
- Diabetes. High blood sugar increases levels of dangerous cholesterol called very low-density lipoprotein (VLDL) and decreases HDL cholesterol. High blood sugar also damages the lining of the arteries, which promotes the deposition of cholesterol in damaged areas;
- High blood pressure. This is a signal of problems with the cardiovascular system that occur with high cholesterol levels;
- Diseases of the liver and gastrointestinal tract contribute to disruption of cholesterol metabolism;
- Endocrine diseases also affect cholesterol synthesis.
Complications of high cholesterol
- Development of atherosclerosis. High cholesterol levels can cause a dangerous buildup of cholesterol and other deposits on the walls of your arteries (atherosclerosis). These deposits (plaques) can reduce blood flow through the arteries;
- Angina pectoris (coronary heart disease). If the arteries that supply the heart with blood (coronary arteries) are affected, chest pain (angina) or other symptoms of coronary heart disease may occur;
- Heart attack. If cholesterol plaques on the walls of blood vessels rupture, a blood clot (thrombus) can form at the site of damage. The clot blocks the flow of blood, blocking the vessel downstream. If blood flow in part of an organ stops, tissue necrosis (death) occurs, which is observed, for example, during myocardial infarction;
- Stroke. Like a heart attack, a stroke occurs when a blood clot blocks blood flow to part of the brain.
Normal blood lipid levels
In the modern world, in countries where there is no shortage of food, to maintain normal levels of lipids in the blood, the main condition is to limit the calorie content of the daily diet and eat the “right” fats. The desired level of cholesterol in the blood, which is often called the target level, is maintained by the normal functioning of the liver, which is able to synthesize the missing amount of any of the lipids. If all these processes are balanced, no harmful deposits occur on the walls of the arteries.
Prevention
To help prevent high cholesterol, you can:
- Be regularly examined in Deal's laboratory;
- Follow a diet low in salt and high in fruits, vegetables, and whole grains;
- Limit the amount of animal fats and use vegetable fats in moderation;
- Maintain a healthy weight;
- Quit smoking and reduce alcohol consumption;
- Do physical exercise for at least 30 minutes a day;
- Control the level of stress you are exposed to;
Reduced cholesterol levels
Decreased is also a problem. Since cholesterol is an important component of cell membranes, a precursor to hormones, bile acids and other components that are important in a living organism, reducing its amount has negative consequences
- It turns out that people with low cholesterol are more likely to have symptoms of depression and anxiety;
- There are studies that show a possible link between low cholesterol levels and the risk of cancer;
- Cholesterol is necessary for the normal synthesis of sex hormones, pregnancy and a normal menstrual cycle. Low cholesterol may be associated with a risk of premature birth or having a low birth weight baby;
The external symptoms of hypocholesterolemia may manifest differently in each person, but laboratory diagnostics can help determine their cause.
When can you suspect low cholesterol or hypocholesterolemia?
- With regular malnutrition, strict diets;
- In the presence of diseases with reduced liver function (including cirrhosis, hepatitis);
- Inflammatory bowel diseases or protein-losing enteropathies;
- For hyperthyroidism or hypoadrenocorticism (Addison's disease). Reduced amounts of glucocorticoids may reduce intestinal absorption of cholesterol;
- If you are exposed to chronic stress;
- For hyperthyroidism or an overactive thyroid gland;
- Adrenal insufficiency;
- With malabsorption (insufficient absorption of nutrients from the intestines), for example, with celiac disease;
- For leukemia.
Secondary hypogonadism in men
28.12.2020
4570
0
In continuation of the first report on primary hypogonadism in men, andrologist, urologist, head of the department of andrology and urology of the National Medical Research Center for Obstetrics, Gynecologists and Perinatology named after V.I. Kulakova, Professor Safar Israidovich Gamidov gave an extensive lecture on the features of secondary hypogonadism in men and available treatment regimens.
S.I. Gamidov
Doctor of Medical Sciences, Professor, Federal State Budgetary Institution “National Medical Research Center for Obstetrics, Gynecology and Perinatology named after. Academician V.I. Kulakov" (Moscow)
As Safar Israilovich recalled, it is mandatory for an andrologist to understand the physiological role of hormones, the ability to interpret endocrine indications for diagnostic purposes, as well as prescribe hormonal drugs with the expected therapeutic effect.
There are a number of cases when an andrologist should think about prescribing hormonal therapy:
- pediatric urology: cryptorchidism, hypospadias, micropenis;
- hypogonadism, including with associated erectile dysfunction;
- hyperprolactinemia;
- infertility (oligozoospermia, sperm DNA fragmentation);
- the need for male contraception;
- priapism;
- benign prostatic hyperplasia;
- prostate cancer with unfavorable prognostic features.
The reproductive function in men works thanks to the hypothalamic-pituitary-gonadal system. In the hypothalamus, the infundibular nucleus is important, containing KNDy neurons (a subpopulation of arcuate nucleus neurons) and GnRH neurons. In the anterior pituitary gland, gonadotrophs produce luteinizing hormones (LH) and follicle-stimulating hormones (FSH). In turn, the gonads produce sex steroids and gametes under the influence of LH and FSH.
Testosterone, estradiol, LH, FSH, prolactin, activins and inhibins, as well as anti-Mullerian hormone play an important role in the regulation of the hypothalamic-pituitary-gonadal system.
In 1977, the groups of A. Schally and R. Guillemin were awarded the Nobel Prize for the discovery of GnRH (gonadotropin-releasing hormone, GnRH). It is a fairly simple decapeptide. At first it was called “LHRH”, but then it turned out that it regulates the secretion of not only LH, but also FSH. As Safar Israilovich explained, a person has on average only 1000–1500 GnRG neurons. They produce GnRH, which enters the portal vein system of the hypothalamic-pituitary apparatus. GnRH circulates in the coronary network of the hypothalamus and pituitary gland.
In women, pulse secretion and GnRH releases play an important role in the regulation of the menstrual cycle. Healthy men have only one mode of its secretion - pulse secretion. About 10–20 secretory impulses occur per day, and there are no pacemakers who could clearly regulate them. The secretion of gonadotropins (LH and FSH) from the anterior pituitary gland is stimulated by the pulsatile release of GnRH and inhibited by the release of gonadotropin-inhibiting hormone from the hypothalamus. LH and FSH have a common a-subunit and a separate ß-subunit. LH stimulates and increases the production of testicular androgen by Leydig cells, and FSH stimulates spermatogenesis in Sertoli cells [1–3].
FSH is a useful indicator for assessing the functional state of the male germinal epithelium, although it is far from perfect. Despite the wide range of standard values (1.4–18.1 IU/l), according to some authors, values of this hormone > 4.5 IU/l already indicate a high risk of impaired spermatogenesis. In addition, unstimulated FSH is a poor predictor of successful sperm surgery in men with non-obstructive azoospermia (NOA) [4, 5].
In practice, mutations of the FSH and LH receptors occur. Mutations of the FSH-ß gene in men invariably lead to azoospermia and a decrease in testicular size. According to some scientific data, existing mutations in FSH receptors provide varying degrees of effects on male fertility. Moreover, depending on the nature of the mutation, the severity of changes in spermatogenesis can manifest itself from severe oligozoospermia to normozoospermia with the possibility of conception naturally. These clinical data correlate well with experimental results obtained in mouse models. Mouse models with altered LH receptors demonstrate decreased levels of serum and intratesticular testosterone and the occurrence of a late block in spermatogenesis [3, 6, 7].
An important factor in the formation of fertility is the level of testosterone. In particular, a large prospective cohort study of 357 men with idiopathic infertility and 318 fertile men found that infertile men had significantly lower levels of total and free testosterone, testosterone/LH ratio, and testosterone/estradiol (p < 0.001) [8].
The main known endocrine regulators of spermatogenesis include testosterone (regulates the number of pale spermatogonia, the effect on other stages of spermatogenesis has not been proven) and FSH (the main factor regulating all stages of spermatogenesis, except meiosis). From a clinical point of view, the synergism of testosterone and FSH is necessary for the initiation and maintenance of active spermatogenesis [3].
With regard to androgen receptors, immunohistochemical analysis of testicular tissue from infertile men showed isolated distribution of androgen receptors only to Sertoli cells. Expression of these receptors in Sertoli cells and adequate intratesticular testosterone concentrations are required for both completion of germ cell meiosis and spermatogonia proliferation. Damage to androgen receptors in Sertoli cells in mice leads to early arrest of spermatogenesis. Insufficient intratesticular testosterone concentrations are associated with impaired integrity of the blood-testis barrier in mice. Increasing the dose of testosterone and FSH promotes the in vitro development of germinal cells obtained from men with early and late block of spermatogenesis into spermatids, and this allows the ISCI procedure to be performed [9–12].
Testicular aspiration biopsy studies in fertile men have confirmed that testosterone is the predominant intratesticular androgenic hormone. The intratesticular testosterone concentration is 60,000 ng/dL, which is much higher than the average serum testosterone concentration in men (500 ng/dL). In the study, intratesticular testosterone concentrations exceeded SHBG concentrations, indicating that the majority of intracellular testosterone is likely in a bioavailable form [13].
Using new analytical methods, the same authors showed that 70% of all intratesticular testosterone is a biologically active substance. However, the concentration of total serum testosterone weakly correlated with the concentration of intratesticular testosterone (p = 0.38). According to new tests, serum bioactive androgens also weakly correlate with intratesticular levels of bioactive androgen (r = 0.46; p = 0.03).
Serum and intratesticular testosterone levels measured simultaneously were highly correlated across studies (r = 0.67, p = 0.03). In addition, significant variability in intratesticular testosterone levels was found, which was highly correlated with serum LH (r = 0.87; p = 0.01). According to the authors, pulsatile LH secretion may reflect a similarly pulsatile secretion of intratesticular testosterone. Pulsatile secretion of intratesticular testosterone was also confirmed when assessing the concentrations of testosterone and estradiol in cannulated gonadal veins in men with varicocele. Sampling every 15 min revealed hourly testosterone pulses (3-5 pulses per hour) with a mean amplitude of 176 +/- 42 ng/mL, 6.6 times the nadir. However, today the effect of intratesticular pulsatile testosterone secretion on spermatogenesis is unknown [14]. However, the same experimental work showed that spermatogenesis in the testicle persists until the level of intratesticular testosterone falls below 75% of the baseline concentration. However, the exact level of intratesticular testosterone at which human spermatogenesis is impaired is not fully clarified.
A promising biomarker of intratesticular androgen status is insulin-like protein 3 (INSL3), which is secreted by mature Leydig cells. Testicular aspiration and serum analysis confirmed that INSL3 was closely correlated with intratesticular testosterone both during induced hypogonadism and after hCG treatment (r = 0.79, p < 0.001). However, inhibin B and anti-Mullerian hormone did not correlate with intratesticular testosterone. Despite these promising results, INSL3 is not yet used in routine clinical practice as a biomarker of Leydig cell function and intratesticular androgen status [15].
An important indicator of the degree of spermatogenesis is inhibin B. In the case of hypospermatogenesis, its secretion decreases, and the secretion of FSH increases. One prospective study found that inhibin B and FSH were significantly correlated with vital semen parameters. At the same time, the values of the correlation coefficient for inhibin B are higher than for FSH (inhibin B: 0.48; p < 0.0001, FSH: 0.41; p = 0.0007) [16].
Activin has the opposite effect. It is a heterodimer or homodimer of ß subunits and is also produced in the testes. Activin has an agonistic effect on the secretion of FSH by the pituitary gland, and its release is inhibited by inhibin B. Activin is not currently used in the clinical assessment of male fertility [17].
In 2001, the peptide kisspeptin was discovered. It has an agonistic effect on GnRH release and pulsatile LH release. Kisspeptin has been used experimentally in men to induce gonadotropin secretion. It has been experimentally shown that the administration of kisspeptin is accompanied by a more pronounced increase in LH than FSH. Currently, kisspeptin is not used in clinical practice [18].
Estradiol is produced from testosterone by aromatase, a member of the cytochrome P450 family. The concentration of estradiol in the blood is low in men, but extremely high in sperm, and its content in the testicle can reach 250 pg/ml, which is higher than in the serum of women. According to available scientific data, only the use of testosterone and estradiol leads to a decrease in the levels of LH and FSH in the blood serum. The inhibitory effect of estradiol on LH is due to a decrease in sensitivity to GnRH. Dihydrotestosterone, which is not converted to estradiol, did not have an inhibitory effect on gonadotropin secretion [19, 20].
For normal spermatogenesis, a sufficient level of estradiol in the testicle is necessary, which has been proven by clinical studies involving infertile men with congenital aromatase deficiency. Estradiol receptors are expressed in Sertoli and Leydig cells, as well as in germ cells. Experimental animals with damaged estradiol receptor are infertile and have abnormal spermatogenesis. Estrogen downregulates spermatogenesis-related genes and induces spermatocyte apoptosis through estrogen receptors 1 and 2. Estrogen regulates luminal fluid reabsorption in the caput epididymis. According to available data, infertility in this category of animals occurs due to impaired reabsorption of fluid from the proximal epididymis and a subsequent increase in intraluminal pressure. This finding raises concerns about the potential direct effects of environmental androgens on male reproduction and reports of decreased sperm count in humans [21–23].
Also involved in the reproduction of aromatase are cytochrome P450 enzymes, which irreversibly convert androgens to estrogens in various tissues, including the testicle, liver, brain and adipose tissue [21, 24]. In the testis, aromatase is localized in Leydig cells [25]. A large retrospective cohort study found an association between infertility, vital semen parameters and reduced testosterone/estradiol ratios. This ratio <10 was considered to be the 20th percentile cutoff point among fertile men. In particular, a similar decrease in the testosterone/estradiol ratio is observed in obese men due to increased peripheral aromatization [26].
Sertoli cells also express thyroid hormone receptors. In addition, thyroid hormones influence the development of Leydig cells and steroidogenesis. Thus, thyroid hormones can maintain different populations of germ cells. There is a connection between teratozoospermia and the presence of a clinical picture of hyper- or hypothyroidism [27, 28].
Under physiological conditions, with a sharp increase in the concentration of prolactin in the blood, testosterone secretion may increase. Many researchers believe that the sleep-related peak in testosterone secretion in men is partly due to an increase in plasma prolactin levels. With chronic hyperprolactinemia in men, GnRH impulses are inhibited, and, consequently, the secretion of gonadotropins and the level of testosterone in the blood are reduced [29].
As Safar Israilovich recalled, there are several types of regulation in the body. Autocrine regulation - the presence of receptors for GnRH, cannabinoids and opioids in the hypothalamus. Paracrine regulation - the presence of receptors for GnRH II and LH, which retrogradely enter the hypothalamus through the portal blood flow. Endocrine regulation - testosterone and estradiol close the negative feedback loop on the pituitary gland and hypothalamus, respectively.
Regulators of GnRH neuron activity in general include estradiol, progesterone, dihydrotestosterone, testosterone, estradiol, cortisol, prolactin, gamma-aminobutyric acid, activins and inhibins, endocannabinoids, opioids, serotonin, leptin and melatonin.
Hypogonadotropic hypogonadism is associated with a deficiency in the production of GnRH and LH/FSH. It can be congenital (with or without anosmia) and acquired (traumatic brain injury, neuroinfections, tumors, operations). Isolated LH deficiency (Pascalini syndrome) is very rare, and isolated FSH deficiency is casuistically rare [30].
Intracranial tumors are the most common cause of acquired forms of hypogonadotropic hypogonadism. Unlike acquired forms, the etiology of congenital hypogonadotropic hypogonadism is more complex and in most cases is idiopathic in nature. The prevalence of congenital hypogonadotropic hypogonadism in men is 1/10,000 [31].
Up to 90% of cases of secondary hypogonadism are not accompanied by signs of organic damage to the testicles or other components of the hypothalamic-pituitarygonadal axis. For these situations, the term “functional hypogonadism” has been proposed [32, 33]. Up to 85% of men with sexual dysfunction due to low testosterone levels have signs of metabolic syndrome.
The list of medications used for hypogonadism is quite wide:
- serotonin reuptake inhibitors;
- antiarrhythmic drugs (amiodarone);
- anticonvulsants (phenytoin);
- antifungal drugs (ketoconazole);
- opiates;
- antipsychotics;
- statins in high doses;
- thiazide diuretics;
- spironolactone;
- cimetidine
To differentiate hypogonadotropic hypogonadism from the constitutional form of delayed puberty, it is necessary to take into account the results of the following tests:
- physical examination;
- karyotype analysis;
- determination of the level of sex hormones;
- test with GnRH analogue;
- determination of bone age;
- MRI of the hypothalamic-pituitary region.
A number of main goals and objectives of the treatment of hypogonadotropic hypogonadism are identified. Thus, the goals of hormonal therapy in this case are to maintain testicular function, develop secondary sexual characteristics, improve quality of life and restore reproductive function. The key to successful treatment of hypogonadotropic hypogonadism is the choice of an adequate drug with an appropriate dose. Preparations of testosterone, gonadotropins and GnRH with a pulsatile pump can be used in the hormonal regulation of patients with hypogonadotropic hypogonadism. If it is necessary to preserve reproductive function in this category of patients, gonadotropins are most preferable [34].
When treating hypogonadotropic hypogonadism, hCG 1000–1500 units. 3 times a week or 2500 units. 2 times a week for 3-6 months, the main goals are normalization of testosterone levels, transition of dark A cells to pale A cells and proliferation of the germinal cell pool. During FSH therapy, 75–150 units. 3 times a week (recombinant, purified or as part of menopausal gonadotropin), the injection area should not coincide with hCG. FSH stimulates the transformation of pale A cells into B cells and subsequent meiosis, and initiates spermatogenesis [35].
Spermatogenesis usually recovers within 6–9 months, although in some patients the process can take up to two years. In approximately 10% of patients, despite therapy using hCG and FSH, spermatogenesis is not restored at all [36]. The effectiveness of therapy does not depend on the etiology of hypogonadotropic hypogonadism: only testicular volume allows predicting the result [37]. The threshold value for testicular volume to predict the effectiveness of gonadotropin therapy is 4 cm3 [38].
In particular, in a study of 36 men from 11 to 42 years old with hypogonadotropic hypogonadism (81% - primary and 19% - secondary), long-term therapy with chorionic gonadotropin drugs was practiced - from 12 to 240 months (average 56). An increase in the number of sperm among patients with reduced testicular size was noted in 36% of cases, and with normal testicular size, an increase in sperm concentration was noted in 71% of patients.
Some authors today mistakenly believe that hCG is an analogue of LH. This is wrong. In particular, oligosaccharide chains protect hCG from biodegradation. The development of immune-mediated resistance to hCG is also possible [39]. In general, combination therapy with hCG and FSH achieves greater success than monotherapy. Side effects of this treatment included acne and gynecomastia.
According to one of the available studies of ten years of experience using hCG and MCG separately and together for the treatment of patients with hypogonadotropic hypogonadism, during combination therapy, compared with hCG, an increase in testicular volume was significantly more often observed (75 versus 50%, respectively). 86% of patients receiving the combination treatment eventually achieved spermatogenesis, compared with 81% of those receiving hCG alone [40]. In approximately 10% of cases, hypogonadotropic hypogonadism resolves spontaneously after stopping the combination treatment. Risk factors for treatment failure include cryptorchidism and small testicular volume (less than 4 ml).
An alternative way to stimulate spermatogenesis in this category of patients may be a pulsatile infusion of GnRH. Hoffman and Crowley in 1982 used gonadorelin as a subcutaneous pulse infusion in patients with hypogonadotropic hypogonadism and achieved spermatogenesis induction in them [41, 42]. Also Chinese researchers in 2010 and 2011. reported the successful use of pulsed subcutaneous infusion of GnRH to trigger spermatogenesis in hypogonadotropic hypogonadism, but the sample size of these studies was relatively small [43, 44].
Pulse therapy with GnRH analogs requires the installation of a subcutaneous or venous pump and mimics the natural pulse secretion of GnRH, requiring regular cannula changes every 2–3 days. This method is considered justified only for hypogonadotropic hypogonadism with azoospermia. Compared with hCG + FSH therapy, this method requires less time to restore spermatogenesis, with it there are fewer testosterone peaks, a lower incidence of acne and breast pain, but a higher incidence of local skin reactions [43].
In 2021, the CONSORT randomized controlled trial was undertaken to comparatively evaluate the effectiveness of hormonal therapy for hypogonadotropic hypogonadism in different regimens, involving 220 patients. Participants were divided into four groups. Group 1 - GnRH for congenital hypogonadotropic hypogonadism, group 2 - GnRH for acquired hypogonadotropic hypogonadism, group 3 - hCG/MCG for congenital hypogonadotropic hypogonadism and group 4 - hCG/MCG for acquired hypogonadotropic hypogonadism. Efficacy assessment was carried out after 18 months [45]. The GnRH group received subcutaneous infusions of gonadorelin at a dose of 100 to 500 mg per day using a special pump every 90 minutes (16 pulses per 24 hours). Depending on the level of FSH, LH and testosterone, the dose of the drug was adjusted. Simultaneously, a solution of hCG at a dose of 5000 IU and MCG at a dose of 75 IU were used. The dose of MHC ranged from 75 to 150 IU in intramuscular injections once or twice a week. The dose of hCG is from 5,000 to 10,000 IU intramuscularly once or twice a week. The dosage of the drugs was adjusted depending on the testosterone level and spermatogenesis productivity, and the testosterone level was maintained at 10–15 nmol/l. The authors showed that either approach to therapy was effective: 25 months after the start of therapy, 90% of patients achieved at least a minimal presence of sperm in the ejaculate, but sperm concentrations of 10–15 million/ml were achieved in only 50% of men. Patients who achieved higher peak LH levels during therapy had a higher rate of sperm recovery in the ejaculate.
In some cases, patients may be prescribed selective estrogen receptor modulators (SERMs), but a common mistake is the unnecessary use of such drugs, in particular clomiphene. In true hypogonadotropic hypogonadism, there is no substrate for SERM activity. In the case of secondary pituitary hypogonadism, there are no pituitary gonadotrophs, and there are no cells capable of synthesizing LH and FSH. Hypothalamic hypogonadism is “tertiary”, in which there is no point in eliminating negative feedback if there is no positive stimulating factor (GnRH). Finally, in hypogonadism associated with hyperprolactinemia, GnRH production does not normalize unless excess prolactin levels are corrected. When prolactin levels are elevated, in particular, the use of cabergoline can significantly improve patients' hormonal levels and help restore sexual function [46].
In conclusion, Safar Israilovich recalled that the hypothalamic-pituitary-gonadal axis is a fragile structure, the functioning of which is better not to interfere without reason and a clear understanding of your actions. The best treatment for hypogonadism in men who are not interested in preserving their fertility is testosterone replacement therapy. Monotherapy with hCG in most cases, with some exceptions, is unjustified and carries risks. It should be remembered that both testosterone and FSH are necessary for normal spermatogenesis. Finally, in case of hypogonadism and erectile dysfunction, it makes sense to conduct a test for serum prolactin.
Sources:
- Ubuka T et al. Front Endocrinol, 2014
- Kumasi TR. Cell Endocrinol, 2007
- Layman LC et al. J Clin Endocrinol, 2002
- Kwee J et al. Fertil Steril, 2008
- Ramasamy R et al. J Urol, 2013
- Kumar TR. Molec Cell Endocrinol, 2007
- Siegel et al. Reprod Sci, 2013
- Andersson AM et al. J Clin Endocrinol Metab, 2004
- Tesarik J et al. Fertil Steril, 2002
- Kato Y et al. Andrology, 2014
- De Gendt K et al. A Proc Nat Acad Sci USA, 2004
- Cheng CY et al. Prarmacol Rev, 2012
- Jarow JP et al. Ann NY Acad Sci, 2005
- Roth MY et al. J Androl, 2010
- Roth MY et al. Fertil Steril, 2013
- Meacham SJ et al. Euro J Endocrinol, 2001
- Hedger, MP et al. Mol Cell Endocrinol, 2012
- Skorupskaite K. Hum Reprod Upd, 2014
- Bagatell C et al. J Androl, 1994
- Hayes FJ et al. Clin Endocrinol Metab, 2000
- Carreau S et al. Adv Med Sci, 2012
- Hess RA et al. Nature, 1997
- Eddie E.M. et al., 1996
- Schlegel PN. Fertil Steril, 2012
- Inkster S.J. J Clin Endocrinol Metab 1995
- Saylam B et al. Fertil Steril, 2011
- Mintziori G. Endocrinol Invest, 2016
- Kumar A. Indian J Endocrinol Metab, 2014
- Corsello SM et al. Clin Endocrinol, 2003
- Mao JF et al. Asian J Androl, 2017
- Varimo T et al. Hum Reprod, 2017
- Grossman, Matsumoto, 2017
- Corona, Maggi, 2015
- Lin et al. Medicine, 2019
- Arroyo et al., 2015
- Schiff et al., 2007
- Farhat et al., 2010
- Miyagawa Y, Tsujimura A. J Urol, 2005
- Leao, Esteves, 2014
- Yang L. Int Urol Nephrol, 2012
- Belchetz PE et al. Science, 1978
- Dwyer AA. Best Pract Rec Clin Endocrinol Metab, 2015
- Zhang G.Y. Reprod and Contracept, 2010
- Sun Y et al. Clin J Endocrinol Metab, 2011
- Lin et al. Medicine, 2019
- De Rosa M et al. J Clin Endocrinol Metab, 2004
The material was prepared by Shaderkina V.A. The video can be viewed on Uro.TV
Comments
To post comments you must log in or register