Author:
- Markaryan Daniil Rafaelevich senior researcher at the Department of Surgery of the International Scientific and Research Center, coloproctologist, oncologist, surgeon
0 (Votes: 0)
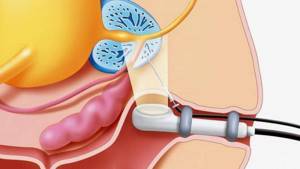
3D ultrasound examination of the anal canal and rectum (transrectal ultrasound, TRUS) is the introduction of a special sensor into the anus to create a three-dimensional image, which opens up new opportunities for the diagnosis and treatment of diseases of the rectum and anal canal.
In medical practice, there are several types of examination of the rectum: percutaneous (does not cause any discomfort, but is the least informative), intravaginal (performed for women if for some reason it is impossible to examine through the anus) and rectal technique (TRUS).
The principle of the study is based on ultrasonic waves emitted by the device’s sensor. These waves are reflected from tissues in the human body, returned through a sensor and converted into a three-dimensional image on a special monitor. The procedure is absolutely harmless and painless.
Transrectal ultrasound helps to evaluate in detail the structure of the anal canal and the condition of the layers of its walls. For example, if there is incontinence, it is possible to evaluate the anal sphincter and its functioning.
The first examination procedure can be confusing for the patient. The patient lies on his left side and is warned that inserting the probe into the anus will be slightly unpleasant. A rectal probe the thickness of a little finger is inserted to a depth of approximately 5-6 cm. The examination itself is painless, so no anesthesia is required, lasts on average 5-6 minutes, the patient receives the results immediately after the examination.
Ultrasound can also serve as a navigation function when performing diagnostic or surgical procedures. This may be puncture of the tumor to take a biopsy or placement of catheters and drainages. Ultrasound is also often performed to monitor after surgery.
TRUS allows you to accurately and quickly determine the presence of a pathological process, localization, size, nature and quantity of contents in the presence of a cavity, the depth of the pathological focus from the skin, infiltration of subcutaneous tissue, the presence of fistulous tracts and additional purulent leaks, which is especially important for establishing diagnosis followed by choice of treatment volume. Among other things, it has become routine in our clinic to perform intraoperative ultrasound examinations during laparoscopic and open surgeries for various colorectal diseases.
Indications for ultrasound of the intestines
Direct indications for an intestinal ultrasound are symptoms such as: defecation disorders (incontinence or constipation), pain and discomfort from the gastrointestinal tract, identified during palpatic examination of intestinal formation, deformations and displacements detected during other studies
.
Endometriosis diagnosed in women is a direct indication for intestinal ultrasound, the same can be said about prostate cancer in men and diagnosed cancer of any part of the intestine. Ultrasound of the intestine is done after surgical interventions related to the removal of tumors to avoid relapses.
Advantages of TRUS
- Unlike other methods of radiation diagnostics, ultrasound examination can be performed repeatedly, since it is not a source of ionizing radiation and can be used without harm even in pregnant women and newborns;
- In men, during the examination it is also possible to assess the condition of the prostate gland and seminal vesicles;
- In women, during the examination it is also possible to assess the condition of the uterus, fallopian tubes and ovaries (on days 5-9 of the menstrual cycle);
- Currently, it is the gold standard for assessing the anatomy and diagnosing pathological processes of the anal canal;
- The study is highly informative in the diagnosis of acute and chronic diseases of the rectum, as well as in assessing the condition of the pararectal space;
- Does not require anesthesia;
- Quite simple to implement;
- Easily tolerated by patients;
- The information content of the method is close to MRI (magnetic resonance imaging), but is a safer, faster and much cheaper method.
Ultrasound of the intestines: preparation for the procedure
The examination results may be distorted by gas formations in the intestinal cavity, so care must be taken to prepare for an intestinal ultrasound. What an ultrasound of the intestines will show in an adult or a child depends on the type of study, which determines the progress of preparation for the examination. For a transabdominal ultrasound, you need to prepare by refusing to eat or drink 6 hours before the procedure. You need to drink at least 1 liter of unsweetened tea or still water per hour. During transrectal ultrasound, an enema or a laxative will be required within the period specified by the doctor. In any case, preparing for an ultrasound of the intestine involves following a diet.
Diet
Products that cause gas formation in the intestines are excluded from the diet. These are all legumes, high fiber foods, milk and dairy products, fatty fish and meat, sweet foods and drinks, carbonated and alcoholic drinks.
Preference is given to boiled meat and fish, porridge with water, no more than 1 egg. in a day. Meals should be fractional - divided into small portions throughout the day. Your doctor may prescribe a drug to prevent flatulence. It would also be a good idea in the evening, if the procedure is scheduled for the morning, to take a laxative and do an enema.
How is an intestinal ultrasound done?

Patients are most concerned about how bowel ultrasound is performed in women and men and how unpleasant or painful the procedure is. It all depends on what type of ultrasound is supposed to be done, as well as on the gender of the patient. Ultrasound of the intestine for women and men can be performed differently. In some cases, both methods are used for a more detailed study.
Transrectal ultrasound
The patient is asked to lie on his side and bend his knees so that they rest against the abdomen.
Transrectal ultrasound of the intestine is performed using a special thin sensor, which is inserted into the anus, then into the colon at a distance of no more than 10-12 cm. The procedure is painless and safe, but requires ideal cleanliness of the intestinal walls.
Transabdominal ultrasonography
With transabdominal ultrasonography, the procedure is more complex as it is carried out in three stages. At the first stage, the patient exposes his stomach, the doctor examines the abdominal cavity in the intestinal area in the usual way using a sensor. In the second stage, the patient is asked to lie on his side, after which saline solution is injected into the intestines.
Fluid in the intestine, straightening its walls, will improve visibility on ultrasound. After a bowel movement, the bowel is scanned again through the abdomen to assess movement status.
Ultrasound research method in assessing the effectiveness of treatment of patients with hemorrhoids

Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Introduction
Drug treatment of hemorrhoids consists of topical and systemic therapy [1] and has the following goals: relief of symptoms of acute hemorrhoids, prevention of complications, prevention of exacerbations in chronic cases.
The pathogenesis of hemorrhoids is dominated by the vascular theory - changes in local hemodynamics, therefore the basis of systemic pharmacotherapy is drugs that improve microcirculation in the area of the hemorrhoidal choroid plexus and anal cavernous glomeruli. For this reason, phlebo- and lymphotropic drugs are widely and effectively used in the treatment of hemorrhoids. Such drugs include Phlebodia-600, the active principle of which is semi-synthetic diosmin. Phlebodia-600 improves microcirculation, accelerates venous outflow, has an anti-inflammatory effect and analgesic effect [2, 4]. These properties of the drug are realized due to an increase in venous tone, anti-complementary activity, inhibition of the reaction of release of inflammatory mediators, a decrease in the production of leukotrienes, an anti-exudative (anti-edema) effect, an increase in tissue oxygenation, a decrease in capillary permeability, and an increase in capillary resistance.
The purpose of this study is to evaluate the effectiveness of the drug Phlebodia-600 for acute hemorrhoids using endorectal ultrasonography.
Materials and methods
To achieve this goal, 20 patients were examined, among them 6 men and 14 women aged from 20 to 65 years, average age - 47.1 years. In 6 cases stage II of hemorrhoids was established, in 10 - stage III, in 4 - stage IV. In 13 out of 20 patients, intense anal bleeding was noted in the form of drops and streams of blood after each bowel movement. Episodic hemorrhoidal bleeding was noted in 7 people who consulted a proctologist due to the appearance of drops of blood in the stool or on toilet paper in the absence of any other symptoms of the disease. All patients underwent sigmoidoscopy, and 14 underwent colonoscopy, during which no pathological changes were detected in various parts of the colon, which could be a source of intestinal bleeding. All patients underwent endorectal ultrasonography using a linear rectal probe with a frequency of 7.5 MHz. To study the effect of the drug "Phlebodia-600" on blood flow in the hemorrhoidal system, Dopplerography was also performed in 14 out of 20 patients in energy and pulse-wave modes with a convex rectal sensor with a frequency of 7.5 MHz, inserted into the vagina. Due to technical difficulties in inserting the rectal convex probe into the anal canal, men were excluded from this group. The studies were carried out using modern ultrasound diagnostic devices before and after the course of treatment with Phlebodia-600. 2 patients did not show up for the re-examination, so further analysis of the research results was carried out in 18 people. Statistical processing of the obtained data was carried out in Microsoft Excell 200. Differences in average values were considered significant at the significance level p
results
During ultrasound examination, the wall of the anal canal has a four-layer structure. The first layer, represented by signals of medium echogenicity, corresponds to the epithelium and subepithelial connective tissue. The second layer, which does not contain reflected signals, is the internal sphincter. Behind it, a band of medium echogenicity is determined, which corresponds to the longitudinal muscle. Next comes a band represented by signals of increased echogenicity, corresponding to the external sphincter (Fig. 1). Below are the muscles that form the pelvic floor [5]. The upper and lower boundaries of the anal canal were considered to be the proximal edge of the internal sphincter and the edge of the anus, which corresponds to the “surgical” concept of the obturator canal.
Rice. 1.
Ultrasonogram of a longitudinal section of the anal canal, endorectal examination. 1 - internal sphincter; 2 - external sphincter; 3 - longitudinal muscle.
The anatomical anal canal is shorter, its upper border is determined by the dentate line, the lower - by the edge of the anus. The location of the dentate line corresponds to the middle of the internal sphincter.
L.P. Orlova studied the angioarchitecture of the rectum and anal canal using triplex scanning in energy mode. Using this technique, it is possible to visualize the first-order branches of the superior rectal artery, which penetrates the wall of the rectum to the submucosal layer at 7 (58%) or 8 cm (42%) from the edge of the anus along the anterior semicircle, which is confirmed by filling the vessels with a contrast agent on macroscopic specimens after abdominoperineal extirpation of the rectum. The diameter of the vessel ranges from 1 to 3 mm (Fig. 2).
Rice. 2.
Ultrasonogram of the rectal wall at the confluence of the first-order branch of the superior rectal artery. Endorectal examination, longitudinal section. Between the marks (++) is a vessel.
The terminal arterial vessels of the superior rectal artery were visualized above the proximal border of the internal sphincter. The number of arteries ranges from 3 to 7, their diameter was 0.07 cm, they are localized at 12, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 and 11 o’clock on the dial in various combinations (Fig. 3 a, b). The superior rectal artery provides more than 70% of the arterial blood flow to the hemorrhoidal plexuses [1]. The internal hemorrhoidal plexus together with the veins form cavernous bodies, which are the main substrate of internal hemorrhoids located in the submucosal space, which is located between the mucous membrane and the proximal part of the internal sphincter.
Rice. 3.
Internal sphincter - transvaginal examination, cross section.
A)
Terminal branches of the superior rectal artery in the anal canal.
b)
With Doppler ultrasound in energy mode; in triplex comparison.
With ultrasound examination, hemorrhoids are a thickening of the epithelial-subepithelial layer with a change in its structure, which becomes hypoechoic. Depending on the stage of the process, the thickening of this layer can be either local and located above the proximal part of the internal sphincter, or above its entire length, or behind its distal part when hemorrhoids prolapse (Fig. 4 a-c).
Rice. 4.
Ultrasonogram of the anal canal - endorectal examination, longitudinal section.
A)
Above the proximal part of the internal sphincter.
b)
Over the entire length of the anal canal.
V)
Behind the distal part of the internal sphincter when the hemorrhoidal node prolapses.
1 - thickening of the epithelial-subepithelial layer, 2 - internal sphincter, 3 - longitudinal muscle, 4 - external sphincter.
The effect of the drug "Phlebodia-600" was assessed by the size of hemorrhoids, the thickness of the epithelial-subepithelial layer, and by quantitative indicators of blood flow, such as peak systolic velocity (PS), end-diastolic velocity (ED), resistance index (RI) and pulsatility index ( PI), which allow one to judge the value of peripheral vascular resistance.
For the convenience of analyzing the results of ultrasound examination in B-mode, the circumference of the anal canal was divided into three segments: anterior (at 10-12 o’clock on the dial), left (at 2-5 o’clock), posterior-right (at 6-9 o’clock), which corresponds to the location main hemorrhoids at 3, 7 and 11 o'clock. According to ultrasound data, thickening of the epithelial-subepithelial layer was detected in the anterior segment in 7 cases (4.0±1.15), in the left - in 10 (3.6±1.65), in the posterior right - in 13 (3, 38±0.5). During the control study after the course of treatment, a statistically significant decrease in the thickness of the epithelial-subepithelial layer was noted in the left and posterior right segment, and in the anterior segment there was an increase in this indicator, but no statistically significant difference was determined (Fig. 5).
Rice. 5.
Changes in the thickness of the epithelial-subepithelial layer during the treatment of hemorrhoids with the drug "Phlebodia-600".
The structure of the epithelial-subepithelial layer has changed, becoming more echogenic, indicating a decrease in edema and the development of connective tissue. Moreover, in 3 out of 14 women, dilation of the veins along the vaginal walls was noted.
Hemorrhoidal nodes identified in the distal part of the anal canal decreased by 2 times in 3 out of 5 patients, disappeared in 1, and remained unchanged in 1. In 1 patient, in the absence of positive ultrasound dynamics and clinically, there was no effect from the therapy - the patient with stage II hemorrhoids still had episodic bleeding. Subsequently, he underwent ligation of hemorrhoids with latex rings.
According to a preliminary analysis of the dynamics of quantitative indicators of blood flow, the following was noted:
- peak systolic velocity in the terminal branches of the superior rectal artery decreased in 10 of 14 women, increased in 3, and remained unchanged in 1 patient;
- end-diastolic velocity in the terminal branches of the superior rectal artery was not determined in any observation;
- the pulsation index decreased in 12 out of 14 women, increased in 2 patients;
- the resistance index remained practically constant.
The average values of peak systolic velocity, resistance index and pulsatility index before and after treatment of patients with hemorrhoids with Phlebodia-600 are presented in Fig. 6.
Rice. 6.
Hemodynamics in the terminal branches of the superior rectal artery in patients with hemorrhoids before and after treatment with Phlebodia-600.
A)
Peak systolic velocity.
b)
Resistance index.
V)
Pulsation index.
Thus, blood flow in the terminal branches of the superior rectal artery in patients with hemorrhoids is characterized by high peripheral resistance and a decrease in the linear velocity of blood flow. After a week's course of treatment of patients with hemorrhoids with the drug "Phlebodia.600" there is a tendency to reduce the peak systolic velocity and resistance index.
When comparing the results of ultrasound examination in B-mode with Doppler sonography data, we can talk about a good effect of the drug “Phlebodia-600” in 11 out of 18 patients, satisfactory in 5, in 2 patients there were no changes in the above listed indicators. It should be noted that in 1 case, a patient with stage IV hemorrhoids had a decrease in the subjective manifestations of the disease, and in another case, there was no clinical effect from the therapy. Thus, the effectiveness of therapy with semisynthetic diosmin is 89%.
Conclusion
Ultrasonography is an objective and reproducible research method that is valuable for assessing the effectiveness of treatment for patients with hemorrhoids. "Phlebodia-600" significantly reduces the size of hemorrhoids, the thickness of the epithelial-subepithelial layer, and also improves hemodynamics in the cavernous bodies, apparently due to increased lymphatic drainage and reduction of perivasal edema.
Literature
- Vorobyov G.I., Shelygin Yu.A., Blagodarny L.A. Haemorrhoids. - M.: Mitra.Press, 2002. - P. 12, 66-81.
- Maamer M., Haring J., Huet V., Dutour G., Rousseau M.Au. Active anticomplimentaire de la diosmine d, hemisynthese. J. Pharmacologie, 1984, 15, 485-6.
- Bodiner MC, Ly SM, Finet M., Jean T. Etude in vitro de l-effet antiinflammatoire de la diosmine d-hemisynthese dans un sisteme de co-culture de celles endothellales veineuses et de granulocytes humaines. Arteres et veines, 1994, 13, 124-8.
- Chauvenet M., Libeskind M. Advantage of using semisynthetic diosmin in acute hemorrhoidal attack. A cross-site, double-blind, cross-site trial versus placebo. Rev. Fr. Gastroenterol, 1994, 304, 3-8.
- Orlova L.P., Markova E.V. Ultrasound anatomy of the anal sphincter. Abstract. report 2nd All-Russian conf. coloproctologists. October 3-4, 1995, Nizhny Novgorod.
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
What will an intestinal ultrasound show?

The doctor makes conclusions based on what the intestinal ultrasound shows. Ultrasound is used to examine the location of the intestine in the abdominal cavity, its structure and wall thickness, the condition of the lymph nodes, possible anomalies, neoplasms, as well as inflammatory processes and injuries. By examining each section of the intestine, many diseases can be diagnosed.
Ultrasound of the rectum
Ultrasound of the rectum can detect ulcers and diverticulosis, indirect signs of the presence of neoplasms (thickening or narrowing of the walls), parasitic cysts, abscesses and hematomas. Also, ultrasound of the rectum allows you to visualize nearby lymph nodes.
Ultrasound of the duodenum
Ultrasound of the duodenum allows you to monitor the healing of the organ in case of an ulcer, and also helps to diagnose duodenitis, neoplasms, and gastritis. Intestinal ultrasound in this case shows spasms and deformations, which accompany many diseases.
Ultrasound of the small intestine
The results of an ultrasound of the small intestine can indicate damage and inflammation, various types of neoplasms, the presence of fluid, as well as diverticulitis, appendicitis, intussusception, and Crohn's disease.
Ultrasound of the large intestine
Like rectal ultrasound, colon ultrasound may indicate neoplasms in the intestine and neighboring organs, diverticulosis, abscesses and cysts, and Crohn's disease.