Colposcopy is a modern, absolutely safe and painless method for diagnosing a number of diseases of the cervix and vagina, including precancerous conditions and oncology in the early stages of development. The simplicity of the equipment and low cost of the procedure, combined with high information content, make it almost irreplaceable. Therefore, it is recommended that all women, without exception, undergo colposcopy at least once a year for the timely detection of dangerous pathologies.
Capabilities and features of the method
The method was first proposed in 1924 by the German gynecologist Hans Ginzelmann. He believed that cervical cancer develops from a small nodule in the epithelium, which cannot be seen with the naked eye. He was also able to find substances that stain areas of abnormal epithelium, detect colposcopic signs of some pathological changes, and propose the use of color filters to facilitate diagnosis. This significantly expanded the capabilities of the method and laid a powerful basis for its further development and implementation in everyday gynecological practice.
Today, colposcopy is one of the leading methods of examining women of any age. The main purpose of its implementation is to study the condition of the mucous membrane of the vagina and especially the cervix with multiple magnification, as well as by conducting special tests. This allows:
- detect even minor changes in the mucosa that go unnoticed during a routine gynecological examination;
- correctly determine the site for collecting biomaterial for cytological analysis or taking an image for biopsy;
- track the dynamics of the course of a previously diagnosed disease and evaluate the effectiveness of the treatment;
- distinguish truly pathological changes from physiological ones and avoid prescribing unnecessary therapy.

To conduct the study, a special device is used, which is a binocular microscope mounted on a tripod - a colposcope. Today, most clinics, including government ones, have modern digital colposcopes that transmit images to a computer monitor. This significantly increases the efficiency of diagnosis, as it allows you to notice even minor changes in the mucous membrane of the vagina and cervix.
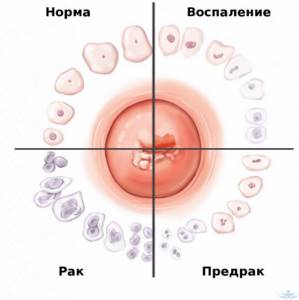
Cytological analysis is necessarily carried out when performing colposcopy, as it allows one to assess the structure and cellular level of damage to the tissues of the exocervix (vaginal part of the cervix) and endocervix (canal of the cervix), taken by scraping the surface layers of epithelial cells. If a gynecologist diagnoses abnormalities during a colposcopy, he may immediately decide to take a tissue sample for a biopsy or a smear to test for bacterial or viral infections.
How is colposcopy performed?
The procedure is performed by a gynecologist and is absolutely painless. To carry out the manipulation, the cervix is examined in mirrors and remotely with a colposcope located 20-25 cm from the patient.
During the examination, the doctor evaluates the condition and appearance of the mucous membrane, the location and type of vascular growth, the level of the epithelium; in the presence of neoplasms, its boundaries, structure, and shape are determined. In the presence of altered areas, one can suspect the presence of benign, precancerous conditions, which can subsequently transform into cervical cancer.
Based on the results of colposcopy, it may be recommended to take samples for a more accurate diagnosis of the detected changes. The collection of material for examination under the control of colposcopy is carried out as accurately as possible, since it allows taking material specifically from the changed areas of the cervix.
In addition, according to indications, secretions are collected for infections and sexually transmitted viruses. If a pathology caused by the human papillomavirus (HPV) is suspected, a Didgene test is also performed - a screening method for identifying oncogenic types of the virus. In addition to diagnosis, your doctor may recommend a biopsy—a removal of a small area of the cervix for subsequent histological examination (tissue analysis).
Colposcopy indications
The procedure is classified as a screening procedure, and therefore it is recommended that every sexually active woman perform it once a year. Colposcopy is mandatory for:
- detection of ectopia during a classic gynecological examination, i.e. erosion of the cervix;
- spotting between periods;
- detection of genital warts of the vulva, vagina, cervix;
- pain and discomfort during or outside of sexual intercourse;
- deviations from the norm in the results of cytological analysis;
- suspicions of the occurrence of malignant processes;
- control of treatment of a number of gynecological diseases.
Indications for colposcopy:
- differential diagnosis of the nature of cellular changes;
- cytology result in which atypical cells were found;
- routine screening at the onset of menopause;
- changes in the mucous membrane that the doctor saw during the examination;
- pregnancy;
- prolonged spotting from the vagina;
- If human papillomavirus is detected, the examination is done annually.
It must be remembered that cervical cancer ranks among the most common cancers in the Russian Federation. Every year it is increasingly detected in young women, which is why you should regularly visit a gynecologist and carry out this procedure. Regular colposcopy, which obstetricians and gynecologists at the Oxy Center recommend once a year, will help you prevent the development of serious problems.
If at the moment you want to have a colposcopy, you can sign up for this procedure at our reproductive center in Krasnodar.
Kinds
There are 2 types of colposcopy: simple and extended. The first involves performing exclusively an examination of the surface of the cervix and vagina with a standard magnification of 8-40 times. When performing it, the gynecologist pays attention to several parameters:
- color and nature of the surface of the mucous membrane;
- features of the location, shape of the vessels;
- localization and type of junction of the cylindrical epithelium typical of the cervical canal and the stratified squamous epithelium (MSE) characteristic of the vaginal part of the cervix;
- the presence of any formations.
Extended colposcopy has broader capabilities and involves the additional performance of several epithelial and vascular tests to identify pathologies that cannot be detected with a simple examination. This is what makes it possible to diagnose initially invisible signs of pathologies and provides indications for performing a biopsy or immediately prescribing certain treatment procedures. Therefore, today extended colposcopy is most often performed. With its help you can:
- evaluate in detail the structure of the epithelium of the cervix and vagina;
- detect the location and extent of the lesion;
- distinguish benign changes from those with signs of malignancy;
- targeted collection of cytological smears and biopsies from the most suspicious areas.
As part of extended colposcopy, after examination under magnification, tests with acetic acid and Lugol's solution are performed. The latter is also called the Schiller test.
Separately, colpomicroscopy is distinguished, which is also called intravital histological examination of the cervical epithelium using dyes. Its main difference is the ability to examine the mucous membrane under a magnification of 160-280 times. But the method requires certain preparation and cannot be used in all cases, and therefore is used for special indications.
Test with acetic acid solution
This test is based on the ability of the epithelium to swell for a short period of time under the influence of a 3% solution of acetic acid. As a result, cell swelling, a decrease in the lumen of subepithelial blood vessels, and a decrease in tissue sensitivity are observed. All this is expressed by a change in the color of the mucous membrane.
The effect of using acetic acid lasts 1-3 minutes.
The test allows you to:
- clearly differentiate MPE from CE, which looks like bunches of grapes;
- detect even mild changes in the squamous epithelium, expressed in the form of white spots with different color saturation and different outlines of the boundaries (this is how areas of atrophic, metaplastic epithelium can appear);
- identify atypical blood vessels, since normal ones temporarily disappear from view under the influence of acetic acid.
The presence of atypia, i.e. the formation of cells with irregular structure, shape and size, is indicated by areas with an intense white-gray color and clear boundaries.
Test with Lugol's solution
The test is based on assessing the degree and uniformity of staining of the mucous membrane with 2-3% Lugol's solution. It is based on the ability of iodine to interact with glycogen concentrated in mature cells of the surface layer of MPE, and as a result give them a brown color.
Based on the intensity and uniformity of staining of the mucous membrane, the following areas can be detected:
- columnar epithelium;
- metaplastic epithelium;
- atrophic epithelium;
- local inflammation;
- atypia.
Colposcopy technique
Before colposcopy, patients are advised to:
- do not use vaginal tablets;
- don't have sex;
- do not wash the vagina with disinfectants;
- do not use tampons.
The colposcopy itself is completely painless and usually lasts from 3 to 5 minutes.
It begins with a routine gynecological examination in the following order:
- Installing a mirror.
- Lubricating the cervix with 3% acetic acid (30 seconds).
- Schilling's test - the cervix is covered with Lugol's solution (iodine solution). It helps visualize tissue and highlight changes that require further examination. This is extremely important to correctly determine the appropriate therapy.
- Targeted biopsy is the removal of a tissue sample from a suspicious location identified by previous methods. The procedure is painless. The doctor examines the sample under a microscope and makes a final diagnosis of the change.
A slight burning sensation may be felt during the application of acetic acid and Lugol's solution, and minor bleeding and vaginal discomfort may occur after the biopsy.
Features of the event
Colposcopy is a routine screening procedure that is in many ways similar to a standard gynecological examination. The only difference is that the doctor enhances his vision with a special device and can conduct additional tests that will detect pathological changes in the mucous membrane, even when it visually looks completely healthy.
The best time to conduct the study is 3-4 days after the end of menstruation. Although in general it can be performed on any day of the cycle, with the exception of menstruation. 3-4 days before the examination, it is recommended to refrain from:
- sexual intercourse without the use of barrier methods of contraception;
- use of intravaginal products;
- douching.
Immediately before visiting the gynecologist, you should empty your bladder.
The procedure is performed on a gynecological chair. The doctor uses a mirror to expose the cervix and brings the colposcope to the chair. Its eyepieces are usually located at a distance of 20-30 cm from the area of interest. Thus, the device does not directly contact the patient’s body. After setting up the colposcope, the image is displayed on the computer screen and the gynecologist, as well as the woman herself, can examine the cervix in detail under high magnification.
The procedure takes no more than a quarter of an hour, and its benefits are invaluable. Indeed, sometimes it is thanks to colposcopy that it is possible to notice signs of a malignant process in the early stages, carry out treatment and save the patient’s life.
Immediately after extended colposcopy, minor discomfort may be observed, which goes away during the day. Scanty bloody discharge may also occur. This is a normal reaction of the body and also goes away on its own. But in order for the woman to feel comfortable, it is recommended to use hygiene products for daily use for several days after the procedure. In all other respects, the patient can lead a normal lifestyle, play sports, etc.
Colposcopy is performed before a bimanual (two-handed) gynecological examination.
Colposcopy during pregnancy
If necessary, the study can be performed even during pregnancy. Although it is advisable to undergo it before its onset and, if violations are detected, carry out appropriate treatment. This will make the pregnancy easier and reduce the likelihood of complications. However, if indicated, colposcopy during pregnancy can be performed. They refrain from carrying it out only in the early stages, since irritation of the mucous membrane of the cervix in some women can provoke spontaneous abortion.
If signs of malignant neoplasms are detected, a biopsy may also be taken from the patient.

Indications for colposcopy
Pap test (cytological method) and colposcopy, as additional screening methods, have a high diagnostic value in detecting precancerous (CIN I, II, III) and malignant lesions of the cervix.
Colposcopy can be performed at every gynecological examination or, most often, if there are indications:
- there are changes in the cervix, such as ulcers;
- bleeding after intercourse.
Other indications include:
- condylomas on the external genitalia, vagina and cervix;
- white changes in the cervix (leukoplakia);
- inflammation of the cervix (cervicitis);
- cervical polyps;
- unexplained vaginal bleeding;
- monitoring the effect of therapy.
Contraindications
Colposcopy is a safe and highly informative diagnostic method. But its implementation is impossible if:
- acute inflammatory process in the cervix, which reduces the diagnostic information and leads to discomfort in the patient during epithelial and vascular tests;
- menstruation;
- allergic reaction to iodine preparations and acetic acid solution.
In such situations, you can limit yourself to a simple colposcopy.
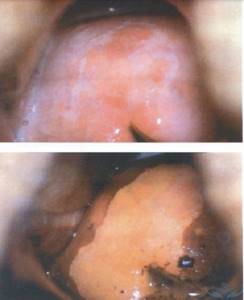
Normal colposcopic picture
If there are no abnormalities during colposcopy, the following will be observed:
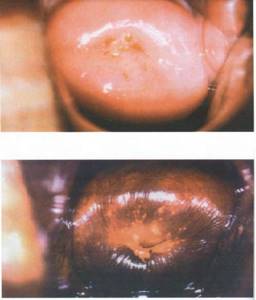
- Original squamous epithelium or genuine MPE. Normally, it covers the vagina and the vaginal part of the cervix and has a light pink tint. But on the eve of menstruation or during pregnancy, it becomes bluish as a result of active blood filling of the blood vessels. When exposed to acetic acid, blanching is observed, and when exposed to Lugol's solution, a uniform dark brown color is observed.
- Columnar epithelium (CE). It lines the cervical canal, but during the development of the organs of the reproductive system it can protrude beyond the external os, which indicates congenital ectopia. In other cases, it should be absent on the surface of the exocervix. CE has a red color due to the thinness of the layer of epithelial cells and an uneven papillary surface. Since its cells are practically devoid of glycogen, it almost does not interact with Lugol's solution, but is more clearly released after treatment with a solution of acetic acid.
- Normal transformation zone (NT) or transformation zone. It is formed when the CE is replaced by a multilayer flat one and is located at the junction of the CE and natural MPE, which is found both on the outer part of the cervix and inside its canal. It contains metaplastic epithelium of varying degrees of maturity, as well as open and closed glands, areas of columnar epithelium with blurred contours.
Ectopia (erosion) refers to areas of columnar epithelium on the surface of the vaginal part of the cervix. Some of its types are considered normal and do not require invasive treatment.

Most women who exhibit a normal transformation zone are considered healthy and do not require treatment. But many patients of reproductive age have a transformation zone and signs of ectopia. Although the transformation zone is considered a benign process, some experts find differences between the stratified squamous epithelium of the ST and conventional MPE. This, in their opinion, can be the basis for the development of cancer and requires monitoring over time.
If large nabothian cysts (closed glands of the cylindrical epithelium) are detected during colposcopy, their opening, removal of contents and coagulation of the bottom are indicated, since they can act as a depot of infections.
Colposcopy
Colposcopy is a method of gynecological examination of the cervix using an optical device - a colposcope . This device resembles a binocular microscope equipped with a light source. If necessary, the doctor can choose the required magnification from 2 to 40 times. The use of color filters during colposcopy allows you to assess the condition of surface capillaries and vessels.
Types of colposcopy:
- Simple - without the use of medications, it has no particular clinical significance.
- Advanced - the use of various special tests to examine the cervical mucosa:
- 3% acetic acid - constricts unchanged blood vessels, the test is mandatory and has the greatest clinical significance;
- Schiller's test - a test with Lugol's solution (iodine reveals glycogen in the epithelium);
Main goals:
- identification of the lesion;
- analysis of the general condition of the mucous membrane of the cervix and vagina;
- differentiate benign neoplasms from malignant ones;
- taking a smear and biopsy for further diagnosis.
During colposcopy, the appearance is assessed (tissue color, vascular pattern; epithelial disorders; presence and shape of glands; boundaries of identified formations).
Preparation for cervical colposcopy
- It is recommended to carry out the procedure after the end of menstruation.
- If an examination is scheduled and the woman begins to have menstrual flow, the procedure should be rescheduled.
- Preparations for colposcopy:
- 2 days before colposcopy you should abstain from sexual intercourse
- do not use various suppositories, sprays, vaginal tablets, unless the doctor specifically recommends using something.
- Do not use intimate hygiene products, but wash your genitals only with water.
- Do not douche yourself a few days before colposcopy.
No painkillers are required before colposcopy - this is an absolutely painless examination, the same as before an examination by a gynecologist, speculums are simply inserted, and the cervix is examined under magnification, nothing touches it.
What diseases can be detected by this study:
| Disease | Definition | Signs detected during colposcopy |
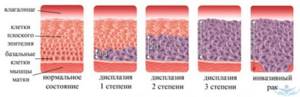
| Cervical intraepithelial neoplasia or dysplasia | A disease of the cervix in which the cells of the stratified squamous epithelium are damaged. Accompanied by the appearance of atypical cells, it is therefore considered a precancerous condition. | Areas of acetowhite epithelium. Leukoplakia is dense white plaques that rise above the surface of the mucosa. Puncture: gentle at the initial stages of dysplasia, and rough at a high degree of damage. When stained with iodine, clear boundaries of the affected area are determined. |
| Congenital ectopia | A congenital condition in which the boundary between columnar and stratified squamous epithelium is located on the outer surface of the vaginal part of the cervix. If there are no complications, then it is a physiological condition and not a disease. | Simple colposcopy: the mucous membrane around the external pharynx is bright red. The area of redness has a regular round shape. After acid treatment, the ectopic area does not turn pale, has clear, even boundaries, and is evenly covered with columnar epithelium. There is no transformation zone. Lightly stained with Lugol's solution. |
| Acquired ectopia, or pseudoerosion | Displacement of the columnar epithelium on the vaginal part of the cervix. An acquired condition associated with viruses, infections, injuries, pregnancy, changes in ovarian function. | The columnar epithelium has a granular surface. The spot has clear boundaries and uneven outlines. In the complicated form, closed or open glands are found. |
| True cervical erosion | Temporary rejection of the upper layers of stratified squamous epithelium as a result of chemical and physical damage, inflammation, and hot douching. | Areas of epithelial damage. The bottom of the erosion is located below the surface of the mucosa. It has an uneven relief and a bright red surface. |
| Eroded ectropion | Eversion of the mucous membrane of the cervical canal. | Deformation of the cervix. A significant increase in organ volume is possible. Overgrowth of scar tissue is visible. Erosion, open and closed glands are formed along the periphery. In a complicated course, there are signs of inflammation - swelling, redness, uneven staining with iodine. |
| Endometriosis | Extension of endometrial cells beyond the inner lining of the cervix. | Rounded lesions of the endometrium, rising above the mucosa. On different days of the cycle, the color changes from pink to bluish. Do not change under the influence of acid and iodine. |
| Condylomas | Small growths of mucous membrane that appear when infected with the human papillomavirus. | Exophytic condylomas - appear above the surface of the mucosa. They have a mushroom-shaped body on a stalk in the form of a dome, papilla or cone. The result of tests with acid and iodine depends on the size of condylomas and the degree of keratinization of the epithelium. Flat condylomas do not rise above the surface. Weakly noticeable during conventional colposcopy. |
| Polyps of the mucous membrane of the cervical canal | Proliferation of the mucous membrane of the cervical canal. | Round or lobed formations in the area of the external pharynx. The color is red. Do not change under the influence of acid and iodine. |
| Erythroplakia of the cervix | A pathological condition in which areas of atrophy and dyskeratosis appear on the mucous membrane of the cervix. Causes: infections, immunity disorders, hormonal status, chemical or mechanical influences. | Bright red areas of thinned squamous epithelium that bleed easily when touched. Blood vessels are visible through the epithelium. Erythroplakia turns pale when treated with acetic acid. Does not stain with iodine. |
| Atypical transformation zone | A term describing changes and pathologies in the zone of transformation of columnar epithelium into squamous epithelium. Depending on the severity of the process, the area of atypical transformation may be borderline with normal or have a high level of atypia (a large number of atypical cells) and indicate a precancerous condition. | Vivid hyperemia – redness of the mucous membrane. Hypertrophy is an increase in the volume of the cervix. Multilayered squamous epithelium with inflammatory changes, deformed transformation zone. Delicate mosaic – pinpoint hemorrhages, delicate punctures. Dilated branching vessels. Open and closed glands may be detected. Areas of chronic inflammation are weakly stained with iodine. |
| Cervicitis | Inflammation of the mucous membrane of the cervix. | The contours are not clear. Closed glands and large Nabothian cysts are detected. Along the periphery there are open gland ducts. There are foci of leukoplakia, acetowhite epithelium, atypical vessels (short tortuous capillaries), mosaic and punctation. |
| Cervical cancer | Malignant tumor of the cervix. | Glassy swollen areas on which outgrowths of various shapes can form. Atypical capillaries in the form of a corkscrew, comma, and hairpin are visible. The capillaries do not connect to each other and do not disappear when exposed to acid. Coarse mosaic and coarse punctation are detected. When treated with acid, the areas become white. |
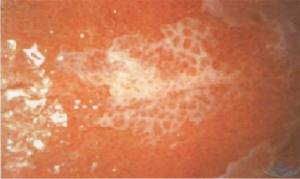
| Leukoplakia of the cervix | A pathology manifested by areas of increased keratinization of the stratified squamous epithelium of the vaginal part of the cervix. | A white spot raised above or at the level of the surrounding epithelium. Has unclear boundaries. |
Abnormal colposcopic patterns
The presence of pathological changes may be indicated by detection during extended colposcopy:
- acetowhite epithelium;
- iodine-negative zones;
- signs of leukoplakia;
- punctuation;
- mosaics;
- atypical transformation zone;
- signs of invasive cancer.
All these cases require an individual approach and additional diagnostic procedures, including biopsy, PAP test, etc. Mild lesions are characterized by the detection of dense acetowhite epithelium with clear boundaries, delicate mosaics and punctures. With pronounced changes, rapid whitening of the treatment area is observed with the appearance of dense acetowhite epithelium and a rim around the open glands. Also in such situations, rough mosaic and punctation, signs of tuberosity, are observed.

Separately, mixed colposcopic patterns are distinguished, which are difficult to unambiguously classify. These include such “findings” as genital warts, inflammatory processes, atrophic changes in the mucous membrane, endometriosis, polyps, etc. In such cases, treatment is also prescribed, which can be either conservative or surgical, or additional examination.
Acetowhite epithelium
The appearance of areas of white or acetowhite epithelium when exposed to 3% acetic acid is one of the most important signs of pathology. Most researchers agree that the vast majority of areas in which the development of malignant processes is observed turn white with varying intensity under the influence of acetic acid.
Detection of acetowhite epithelium is typical for all degrees of CIN and makes it possible to diagnose the presence of changes at the earliest stages of development. CIN refers to cervical dysplasia, which is accompanied by the formation of cells with varying degrees of atypia in the covering epithelium. Untreated dysplasia can lead to cervical cancer, and each case of its development is the result of missed opportunities and ignoring the importance of regular colposcopy.
It is important to differentiate white epithelium from areas of dyskeratosis, i.e. leukoplakia. Some blanching of the mucous membrane can also be observed with:
- disturbances in the structure of epithelial cells;
- inflammatory process;
- papillomavirus infection;
- some other benign changes.
The more intense the whitening of the tissue and the longer it persists after exposure to acetic acid, the more serious and profound the changes.
Iodine-negative zones
A typical sign of pathology is the identification of so-called silent iodine-negative areas of the mucosa after applying Lugol's solution. In most cases, they are represented by keratinized epithelium and require a more detailed examination by performing a biopsy.
Leukoplakia
Leukoplakia is a pathology accompanied by keratinization of the epithelium of the vagina, vulva or cervix. Colposcopically, it looks like a white spot of arbitrary shape with clear boundaries, which can be noticeable even before treatment of the mucous membrane with solutions. Most often, leukoplakia is observed in the area of the transformation zone and can have different sizes. The true size of the modified area is determined after treatment with Lugol's solution, since it does not turn brown. The main danger of leukoplakia is the inability to determine, without the use of invasive methods, what changes are located under the layer of keratinized cells. Therefore, if it is detected, a targeted biopsy is indicated.
punctuation
Puncture refers to multiple red dots on the background of the epithelium, caused by its atypical vascularization, i.e., the formation of blood vessels. The degree of violation is determined based on the size and uniformity of the points. They are clearly visible after exposure to acetic acid, and sometimes have the appearance of papillae.
Mosaic
This term refers to the zone of the mucous membrane, which, after treatment with acetic acid, is delimited by red lines into yellowish-white segments. This area is devoid of open and closed glands. Based on the intensity of the mosaic, the degree of tissue damage is determined. Thus, with a rough mosaic, the mucous membrane takes on the appearance of a paved pavement, but more often a delicate mosaic is observed - the segments do not protrude above the level of the surrounding tissues and have a marble pattern. Most often, the mosaic is iodine-negative.
Atypical transformation zone
It is formed on the basis of normal ST, but differs in the presence of:
- atypical blood vessels;
- acetowhite epithelium;
- keratinized glands;
- leukoplakia;
- mosaics;
- punctuation;
- areas not stained with iodine.
This indicates the presence of significant changes in the structure of the epithelium and the likelihood of developing dysplasia.
Invasive cancer
The most distressing “finding” during colposcopy may be the discovery of signs of invasive carcinoma:
- atypical transformation zone with uneven tuberosity and the presence of a limited area rising above the level of surrounding tissues (plus tissue);
- ulcers;
- atypical vessels, characterized by fragility, which leads to bleeding.
As a rule, oncology develops against the background of benign changes in the cervix, which were not diagnosed and eliminated in time.
Thus, the possibilities of colposcopy are truly wide, and its accessibility, low cost and ease of implementation are its indisputable advantages. Therefore, it is important not to ignore preventive gynecological examinations and doctor’s recommendations to perform colposcopy. Often this is what makes it possible to diagnose severe pathologies in the early stages, carry out the necessary treatment and save the patient’s life.
0 0 votes
Article rating