Scintigraphy: history, what it is used for
The use of this diagnostic technique makes it possible to obtain a two-dimensional image of the area under study after a radiopharmaceutical (RP) has been introduced into the body. This process detects the gamma radiation emitted by the drug using a scintillation camera.
Substances labeled with a gamma-emitting marker isotope can accumulate in tissues and organs. This, in turn, allows the doctor to detect pathological foci in which radiopharmaceuticals have accumulated.
The technique is used to search for foci of the disease. It is based on recording the passage of a radioactive tag through the area of interest. The technique is highly informative, if we take into account the characteristics of the organs.
During the procedure, radiation exposure to the patient’s body is minimal, since a radioactive pharmaceutical is used in microdoses.
From the history
We can say that the birth of the technique was 1911. György de Hevesy, a promising young scientist, living in a dormitory, made the assumption that the canteen was using stale food left over from the day before.
He decided to test his guess by adding an indicator to the uneaten portion. The radiation recorder found it in the food served the next day. This brought to light the cooks who were cheating, but most importantly, a new page was opened in the research.
More than forty years have passed and the method has entered medical practice. This happened thanks to the invention of gamma cameras, which are devices for absorbing and converting the energy of gamma quanta.
The invention made it possible to understand how radionuclides move and distribute in the body. A little later, the methods used for this began to be called:
- Radiometry;
- Radiography;
- By scanning.
The development of computer technology and the improvement of gamma cameras pushed to a new stage. A comprehensive study emerged that made it possible to obtain, process and store information about the activity of a particular organ or system. Here, the dependence of their ability to accumulate radiopharmaceuticals was taken into account. This is how scintigraphy was born.
Now the technique is widely applicable in Europe and the USA. And in our country it also begins its march.
Static and dynamic scintigraphy
Radionuclide scanning can be carried out in static or dynamic mode:
- Static radioisotope scanning is performed once and takes a short period of time, during which the required number of images are obtained in several projections.
Such an examination allows one to identify characteristic changes in tissues, but does not give an idea of the functional state of the organ.
- Dynamic scintigraphy involves sequential multiple scanning at certain time intervals, obtaining a series of scintigrams in the same projections.
By comparing images, doctors estimate the rate of accumulation and/or removal of radionuclides. This gives them the opportunity to judge the preservation or disruption of the functions of various tissues and structures, slowing down or accelerating the metabolic process.
What is the method used for?
The method is applicable for diagnostic purposes, and also works as an assessment of the effectiveness of treatment of various organs.
The method has advantages that are difficult to overestimate. Among them:
- Recognition of the disease at its early stage, much earlier than X-ray examination;
- Safety;
- Possibility of conducting research regularly, since radiation doses are minimal;
- The ability to assess the functional characteristics of the organ being studied;
- Ability to assess the scale of damage;
- Distinguishing between malignant and benign neoplasms;
- No preliminary preparation for the study is necessary.

Laparocentesis
Skeletal bone scintigraphy (osteoscintigraphy)
Philips Bright View gamma camera for scintigraphy
Radionuclide examination of bone tissue can be prescribed both for suspected primary malignant neoplasms and for the diagnosis of metastases. During the examination, all bones are scanned. This is especially valuable when metastasis is suspected, since secondary tumors are most often multiple and develop in different parts of the skeleton. The location of metastases depends on the type of cancer.
Advantages of osteoscintigraphy:
- On X-rays, cancerous foci are detected only when the process affects more than half of the bone tissue. During radioisotope examination of the skeleton, metastases are detected in the early stages.
- Skeletal bone scintigraphy allows you to detect all neoplasms during one examination.
Thyroid scintigraphy
Radioisotope scanning of the thyroid gland makes it possible to study its functional state, as well as to identify zones of increased or decreased accumulation of radionuclides - “hot” and “cold” nodes.
The presence of “hot” nodes more often indicates benign tumors of the thyroid gland (nodular goiter), while cold nodes indicate cancerous degeneration.
The specificity of thyroid scintigraphy in the differential diagnosis of tumors is low. In this regard, examination, as a rule, is prescribed when ultrasound and other methods are insufficiently informative.
Scintigraphy of the parathyroid glands
Using radionuclide scanning, doctors differentiate between benign and malignant nodes, and also analyze the functional state of the parathyroid glands, which play an important role in human metabolism.
The sensitivity of the method is 70-90%, specificity is 98%. Thus, this method of examining the parathyroid glands is more informative than CT and MRI.
Renal scintigraphy (nephroscintgyraphy)
When performing static renal scintigraphy, a tumor with a diameter of 20 mm or more can be detected. The study also makes it possible to identify changes in various tissues and structures of the organ, by the nature of which doctors judge the presence of certain problems.
Studying the absorption and excretion of radioisotopes by the kidneys over time is more informative. The main advantage of dynamic nephroscintigraphy compared to other methods for diagnosing renal cell cancer is the ability to detect atypical cells at the very beginning of the disease, that is, when the tumor is not visible on x-rays.
Due to the fact that radioisotopes are quickly accumulated by the kidneys and also quickly eliminated, the examination does not take much time. The study is especially indicated in cases where it is necessary to determine the possibility of kidney surgery and its volume.
The study may also be part of a comprehensive diagnostic examination for suspected cancer of the mammary glands (mammoscintigraphy), lungs, esophagus, liver, testicles and prostate gland.
The advantages of performing scintigraphy with us:
Our department is equipped with a single-photon emission computed tomograph combined with an X-ray computed tomograph, which allows us to conduct studies of almost all human organs and systems, including skeletal scanning, obtaining cross-sectional images of organs for precise localization of the pathological process.
Each report is prepared by two doctors of the department (the “double reading” method), if necessary, with the involvement of employees of the Department of Radiation Diagnostics and Therapy of the leading medical university of Russia - RNRMU named after. N.I. Pirogov.
The conclusion is issued on the day of the study, usually within 40-60 minutes after completion of the study.
If necessary, images in additional projections or SPECT are taken free of charge.
A modern department, built according to modern building and sanitary standards, equipped with a waiting room before the examination, will ensure the comfort of the procedure, whether it is scanning the skeleton or any other organ.
Scintigraphy"
Side effects
Mammoscintigraphy is a relatively safe diagnostic method. In most cases, the procedure is painless and well accepted by the body.
Some women may experience side effects such as:
- headache;
- vomit;
- insomnia;
- increase in blood pressure;
- nausea;
- fatigue;
- discomfort in the back or neck.
Such manifestations are considered normal, go away on their own within a few hours, and do not require special treatment.
Indications and contraindications for the study
Skeletal bone scanning is recommended in the following cases:
- to identify oncological pathologies with bone metastasis;
- for diagnosing fractures and tumor processes in bones;
- as a monitoring method for the dynamics of treatment;
- to identify areas with altered bone tissue during dystrophic processes.
Also, scanning the skeleton bones is indispensable if radiography could not detect cracks, fractures and other bone injuries.
How does the procedure work?

Standard protocols recommend performing scintigraphy on days 5 to 10 of the menstrual cycle. However, the relationship between this factor and the results of the study has not been reliably established. Postmenopausal women can be examined at any time.
In some cases, scintigraphy will have to be postponed:
- after surgery - for 2 months;
- if a fine-needle puncture biopsy was performed - for 14 days;
- after a pistol biopsy - for 4-6 weeks.
The procedure does not require complex special preparation. Two weeks before the procedure, you need to take a biochemical blood test. Four hours before the procedure you should stop eating. When going to the clinic, you need to wear clothes that will be comfortable for you to get an injection in your leg.
The doctor injects a radioisotope (99mTc-Technetril) into a vein. The patient is sent to the waiting room, where she spends from 15 minutes to 3 hours (when analyzing the presence of metastases in the bones).
After the injection, the patient is a source of ionizing radiation for some time. During the waiting period, it is necessary to avoid contact with other people, especially small children and pregnant women.
Then the woman lies down in a tomographic gamma camera, where she takes pictures in several projections:
- straight - lying on your back with your hands behind your head;
- two lateral ones - in a position on the stomach. The arms are extended forward, the detector from the side approaches as close as possible to the area under study;
- oblique - it is required only if it is necessary to clarify the localization of the tumor.
On the tomograph table you need to be in a state of complete rest and breathe regularly. Any movement distorts the image. All metal items of clothing and jewelry must be removed in advance.
The patient stays in the gamma chamber from 20 minutes to an hour. Then the girl is given the scan results and can go home. The complete examination takes 1.5-2 hours.
Contraindications
Due to the good tolerance of the examination, it can be performed quite often. To monitor cancer treatment, the procedure is done several times a year. Despite the relative safety of the study, there are a number of limitations for its conduct:
- Pregnancy is an absolute contraindication to scintigraphy due to the risk of harmful effects on the fetus. If there is a danger to the life of the pregnant woman, the examination can be done at a later stage.
- The lactation period is a relative contraindication. Since radionuclides are excreted in breast milk, a woman is advised to stop breastfeeding for a day and express milk.
- The procedure should be performed with caution in patients with a history of anaphylactic shock and angioedema.
- The limitation is early childhood. However, if the benefit outweighs the harm, then the child can be examined.
- Terminal stage of cardiac, renal, liver failure - due to the risk of fatal complications.
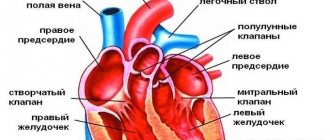
Myocardial scintigraphy results
When reading the scintigraphy results, the doctor can determine:
- intensity of coronary circulation;
- degree of blood supply insufficiency;
- localization of necrotic areas;
- foci of ischemia during exercise;
- scars after a heart attack.
Also, based on the results of the study, the likelihood of developing possible complications is calculated, a program of conservative treatment is planned, or the method of surgical intervention is determined.
Scintigraphy is not informative in assessing the size of the heart and the condition of the coronary vessels. That is, this method will not allow one to determine the location and degree of narrowing of blood vessels.
Scintigraphy of the thyroid gland with 99mTc-pertechnetate
Diagnosis of thyroid cancer (TC) is a single dynamic process that combines physical examination data with a whole arsenal of the most informative diagnostic tools, one of which is radionuclide testing of the thyroid gland (thyroid). Radionuclide testing today remains the main method for obtaining images, assessing the functional activity of the thyroid gland and identified solitary nodular formations.
Indications:
- Assessment of the functional state of thyroid nodules identified by any examination method in primary patients;
- Timely detection of recurrent thyroid cancer in the projection of the bed of the removed gland and/or lobes in patients with a history of thyroid cancer;
- Detection of regional and distant metastases of thyroid cancer in patients after radical treatment;
- Suspicion of the presence of a retrosternal goiter;
- Search for an atypically located thyroid gland;
- Determination of the connection between tumor formations palpated in the neck area and the thyroid gland.