Colposcopy is considered a non-traumatic and very informative method for diagnosing cervical diseases. As before most other studies, before colposcopy, patients are recommended to have some restrictions, one of which concerns intimate life. However, for most women, the question regarding the advisability of refusing sex before the procedure remains unclear.
Can intimacy affect the diagnostic result? Is it possible to have sex with a condom without any consequences? What happens if you hide the fact of proximity from the doctor? Patients have no less questions about sexual relations after the procedure. If no interventions were performed, is it possible to have sex after colposcopy without fear for health? The answers to these questions can be found in this material.
What is colposcopy in gynecology?
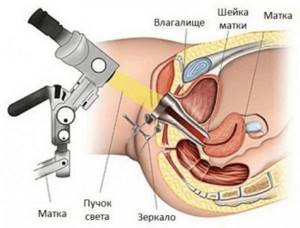
Colposcopy is a special examination of the cervix, which is carried out using a special microscope. This examination method allows the doctor to examine the tissue of the cervix under high magnification. Colposcopy of the uterus is an opportunity to conduct an early diagnosis of cervical pathology, determine the presence of precancerous processes and the stage of cervical cancer.
A specialist performing a colposcopy can suspect the occurrence of a malignant tumor at an early stage, determine its location and the required area for a targeted biopsy, and also collect material for a cytological smear.
It is important to remember that if you are scheduled for colposcopy, this procedure is completely safe. There are several varieties of this examination method:
- — simple colposcopy (in this case, special medications are not used);
- — extended colposcopy (examination of the cervical mucosa using special tests).
The main task of the procedure:
- Assessment of the condition of the mucous membrane of the cervix and vagina.
- Identification of the true source of the lesion.
- Differentiation of all benign changes from suspicious formations into malignancy.
- Targeted collection of biopsies and smears from suspicious areas.
How gynecological colposcopy is performed in our medical center
- For gynecologists (diagnosticians) at Leib-Medic, gynecological colposcopy is not just an ordinary, standard procedure. In the office you will be met by a doctor - a PERSON, for whom your current problems will be a priority!
- For most women, visual examination of the cervix using a colposcope causes embarrassment in front of the doctor. In our center, delicacy and caring attitude towards patients is the basis of everything.
- During the preliminary conversation, you will build trust and feel comfortable with the procedure.
Distrust of new examinations is natural. But at the Life-Medic antenatal clinic you will get rid of your fear during colposcopy. You will know that everything is fine inside!
What does colposcopy show?
This study allows you to diagnose many diseases, among which are inflammation, precancerous tissue changes or cervical cancer, precancerous tissue changes or vaginal cancer, vulvar cancer, genital warts, etc. This is a very important procedure, which is not recommended to be abandoned without serious reasons.
Why is colposcopy done?
Many women are interested in when to do a colposcopy? What indications are needed to carry it out?
The examination is best carried out after the end of menstruation or before its start, since colposcopy during menstruation can interfere with normal diagnosis.
It is worth noting that experts consider this research method to be subjective. The patient’s health is in the hands of one doctor, who performs the procedure. If the gynecologist turns out to be inexperienced, it is likely that he will not be able to establish the real picture of what is happening. Based on this, you should only contact trusted clinics with experienced specialists.
An important question is: why is colposcopy of the vagina and cervix done? The main purpose of the procedure is to determine the signs of benign diseases of the squamous cervical epithelium. The study is also necessary when it is necessary to establish signs of a possible malignant neoplasm.
If your cytological smears reveal manifestations of cellular atypia, you definitely need to undergo this examination. The results of colposcopy will help to establish an accurate diagnosis of a particular pathology and determine the affected areas of the epithelium.
Colposcopy is also needed to draw a conclusion about the general condition of the cervix. This is important during pregnancy, when the doctor determines the form of subsequent labor.
Extended colposcopy protocol
Each patient can receive examination results containing the following items:
- Type and shape of the cervix (cylindrical, conical, deformed, hypertrophied).
- Type of external os of the uterus (round, semilunar, slit-like).
- Post-traumatic deformation (present, absent).
- Erotic ectropion – inversion of the mucous membranes of the cervical canal (yes, no).
- Endocervicosis – ectopia of the cervix (yes, no).
- Transformation zone (ZZ): normal (open, closed or keratinized glands); atypical (epithelium is iodine-negative or acetate, punctation and mosaic are gentle or rough).
- Vessels (absent or present, what type - regular, enhanced, atypical).
- Leukoplakia of the cervix is a nonspecific process that occurs in the squamous epithelium and is characterized by its keratinization and thickening (yes, no).
- Relief of the mucous membrane (smooth, raised, uneven).
- Cicatricial changes, polyps, true erosions, fine punctate ulcerations, exophytic (visible) condylomas, signs of post-coagulation syndrome, endometriosis, local and diffuse inflammatory processes (present, absent).
In a healthy woman, the mucous membranes of the vaginal part of the cervix are covered with an epithelial layer with an even texture, have a pale pink tint (bluish is observed in the 2nd half of the cycle), the vascular pattern has the correct type and uniform distribution. Any change in the listed indicators is a reason for further examination.
Colposcopy of the cervix
You can learn everything about how cervical colposcopy is done directly from your gynecologist before the procedure. This research method shows high efficiency for identifying cervical diseases:
- — erosion;
- — dysplasia;
- - ectopia;
- - cancer and precancerous conditions;
- - erythroplakia.
Indications for colposcopy are the diagnosis of any disease through cytological examination. For example, during an examination, a gynecologist may discover some suspicious areas on the cervix, which will be the reason for a subsequent colposcopy.
This procedure should be carried out approximately once a year and for preventive purposes. To determine the nature of the mucous membrane and discharge, a routine examination of the vagina and cervix occurs.
Do not be nervous if you are scheduled for a procedure such as cervical colposcopy - reviews of this type of examination are almost always positive. It is worth noting that there are no contraindications to its implementation. The study is completely safe; it is canceled only in case of hypersensitivity to a certain drug.
Cervical colposcopy results may be inaccurate if the procedure is performed during menstruation. Insufficient cleansing of ointments and menstrual blood makes examination much more difficult. In this case, the specialist may prescribe a re-examination after the end of menstruation.
The price of cervical colposcopy can be found at the Endoscopic Surgery Center LLC clinic. Typically, the cost of cervical colposcopy ranges from 800-3000 rubles. It all depends on the specifics of the research. You can find out detailed prices from the gynecologist who will conduct the appointment.
Extended colposcopy
If you need to have a colposcopy due to erosion, the doctor will choose an advanced examination method. Extended colposcopy of the cervix is carried out with a special device - a colposcope, which allows you to carefully examine pathological formations on the vaginal mucosa and cervix with multiple magnification. Thanks to this study, the doctor can determine the location and size of the erosion, its boundaries, zones of leukoplakia and the presence of pathological angiogenesis. The transformation zone during colposcopy at the border of healthy epithelium and cervical erosion is also important.
Extended colposcopy of erosion does not cause the woman any noticeable discomfort or pain. If a specialist discovers atypical vessels during colposcopy, he must take the suspicious area for histological examination. This is often done using a stab biopsy of the cervix, followed by stitches to the affected area.
With the extended method of examination, the cervix must be treated with a special Lugol's iodine solution. In this case, healthy epithelium should stain well and acquire a rich brown color. This is how an iodine-negative zone is detected during colposcopy. The test helps to determine the boundaries of erosion and identify areas of leukoplakia. But only histological examination gives a final diagnosis.
Colposcopy and smear for oncocytology are procedures that are often performed simultaneously. A smear is taken using a special endobranche to examine it for atypical cells.
Survey options
There are three main types of cervical colposcopy:
- Observational or simple type - does not require additional surface treatment with special substances. The method is indicative; it determines the shape and size of the uterine cervix, the general condition of the surface, the presence or absence of damage, and their nature. During the manipulation, the gap between flat and cylindrical epithelial structures, the relief of the mucous membrane, its color, the location of the vessels are studied, and the nature of the existing secretions is assessed.
- Extended - testing is carried out by treating the surface of the mucous membrane with medications. The procedure begins by covering the surface with a 3% acetic acid solution. After its application, a process of coagulation of intracellular and extracellular mucous secretions, short-term swelling of the epithelium, and narrowing of the vessels located in it are observed.
The test begins a minute after applying the solution and lasts no more than 3-4 minutes. The final reaction of the vessels to the treatment is of important diagnostic importance: the newly formed vascular networks do not have muscle layers and are incapable of contraction, all others disappear from view.
The second stage of the examination includes treatment of the mucous membrane with 3% Lugol's solution with glycerin, the second name of the test is Schiller's test. In the absence of pathological changes, the entire surface is painted a uniform dark brown color. The affected areas remain unchanged, which allows you to accurately determine their location and area.
- A variation of the extended type of colposcopy is chromocolposcopy. It uses various staining substances - hematoxylin, methylene blue, etc. The research indicators remain standard: pathological areas do not change shade, healthy areas are evenly stained.

Additional methods for cervical colposcopy are two forms of testing:
- Colored version - carried out to clarify the characteristics of existing tumors. The mucous membrane is treated with specialized blue or green dyes.
- Luminescent - special dyes applied to the area being studied are absorbed by cancer cells. The tumor changes color to a bluish-pinkish tint when examined with ultraviolet light.
Colpomicroscopy differs from the standard procedure by magnifying the area being viewed from 160 to 280 times. Manipulation is considered to be an intravital histological examination of the epithelial layers of the cervix. During diagnostics, equipment is brought to the uterine cervix, which makes it possible to examine the features of the surface epithelium, its cytoplasm and nuclei.
The analysis is highly informative, requires preliminary preparation, and does not detect carcinoma or invasive cancer. Contraindications to the study include vaginal stenosis, severe bleeding of the mucous surfaces of the organ, and tissue necrosis.
The cost of cervical colposcopy depends on the type of procedure prescribed.
Colposcopy during pregnancy
Today, many pregnant women are prescribed a colposcopic examination. The reason for this may be such a fairly common disease as cervical erosion - colposcopy in this case is mandatory. However, many pregnant women wonder how safe the procedure itself is and is it possible to do colposcopy for pregnant women?
According to experts, colposcopy of the cervix during pregnancy is absolutely safe for both the expectant mother and the baby. The study makes it possible to identify pathologies, as well as timely diagnose precancerous conditions. If the patient has erosion, the doctor will determine its degree, which will help decide the form of the upcoming birth, that is, whether it will be natural or by cesarean section.
The examination cannot affect the course of pregnancy and the health of the woman and fetus. Before a colposcopy is performed during pregnancy, the gynecologist must perform a routine examination and smear examination. If a suspicion of erosion is detected, the doctor refers the patient to colposcopy to obtain more accurate information about the suspected pathology. If the diagnosis is confirmed, follow-up examinations should be done every 3 months. In this case, you will also need a colposcopy after childbirth.
If you are just planning to become pregnant, you can prevent this test from being performed while you are pregnant. To do this, you need to go through the procedure at the planning stage. The doctor will be able to determine whether there are any serious gynecological problems or not. Almost everyone who has undergone a procedure during pregnancy, such as colposcopy, leaves positive reviews.
If you are planning or are pregnant, your doctor may prescribe one or more procedures such as colposcopy (the cost in this case remains the same as for non-pregnant patients).
Preparatory stage
The attending physician explains in detail the preparation rules to eliminate false positive results. These include:
- the need to avoid sexual intercourse 48 hours before the appointed date;
- the use of vaginal suppositories, sanitary tampons, and douching is prohibited - to preserve the natural indicators of the vaginal microflora;
- If the patient has a low pain threshold, then before colposcopy she takes weak painkillers from the pharmacological subgroup of NSAIDs - Ibuprofen or Paracetamol.
The cost of the colposcopy procedure in Novorossiysk allows you not to wait for a queue at the state gynecology department, but to apply at any time convenient for the patient.

Colposcopy of the intestine: what is it?
This procedure is often called colposcopy, although the correct medical name is colonoscopy. During the diagnostic procedure, the endoscopist examines and evaluates the condition of the inner surface of the colon and rectum, while he uses a set of instruments for colposcopy - a special probe.
Why is rectal colposcopy performed?
Indications for this may be suspicions of any pathology of the large intestine: inflammatory and tumor processes, pain, bleeding, constipation, sensation of a foreign body.
Contraindications to colonoscopy include:
- — acute infectious diseases;
- - severe pulmonary and heart failure;
- - ulcerative and ischemic forms of colitis;
- - peritonitis;
- - blood clotting disorder.
Colposcopy of the rectum in most cases is tolerated normally and does not cause discomfort. There may be only some discomfort, but with the help of a doctor and nurse, this can be avoided.
The specialist will advise you to take an antispasmodic before the study - it will relax the muscles of the intestinal wall and significantly reduce discomfort. You will also need to cleanse the intestines naturally or with an enema. There is no pain from the procedure when using an anesthetic. If modern equipment is used for diagnosis, then anesthesia is not necessary.
An experienced specialist will be able to perform a colposcopy of the intestines in 10-20 minutes. Before the procedure, you must remove your clothing below the waist, including underwear. During the examination, the colonoscope is inserted through the anus into the intestinal lumen, after which it is slowly advanced further with a moderate supply of air (it is necessary to straighten the lumen of the intestinal tube). After the procedure is completed, the air introduced into the intestine will be aspirated using a special channel of the endoscope. The feeling of bloating that appears will go away immediately.
In pathological conditions, a colonoscopy alone may not be enough - the doctor also performs a biopsy. In some cases, the patient also undergoes medical procedures, for example, polypectomy.
To find out how much a rectal colposcopy costs, you need to contact the clinic. The approximate price is about 3000 rubles.
How safe is it? Are there any complications?
Colposcopy is an absolutely safe examination, because during it the instrument does not come into contact with the vagina, only speculums are inserted inside. But a biopsy is an invasive procedure. In rare cases, complications arise after it. You should see a doctor if pain and bleeding persist for a long time, or if you experience the following symptoms:
- Heavy bleeding from the vagina.
- Severe pain in the pelvic area.
- Fever - an increase in temperature over 39 degrees.
Preparing for colposcopy
You already know the answer to the question when is the best time to do a colposcopy. This is the time before or after menstruation. But does a procedure such as colposcopy require preparation for the study? There are some things you need to know before going to the gynecologist.
Particularly serious preparation for the examination is not required. Most often, specialists prescribe the procedure for the first 3 days after the end of menstruation. A couple of days before the procedure, it is recommended to refrain from any sexual contact with a partner, as well as from douching, using vaginal ointments, suppositories and tampons.
For women with an easily excitable nervous system, the doctor may advise taking any over-the-counter pain reliever, for example, paracetamol or ibuprofen. Compliance with any diet or diet during a procedure such as cervical colposcopy does not require preparation. It is also important not to be nervous during the examination, especially for pregnant women.
After the main procedure, the doctor may decide to also do a biopsy. If cell collection is carried out under anesthesia, then 12 hours before it begins, you must stop drinking water and eating. In this case, colposcopy and drinking are incompatible things. If a biopsy is not planned, you can drink water.
Contraindications for carrying out
Prohibitions on examinations are divided into relative and absolute. The first include bleeding, an acute inflammatory or strophic process, the first two months after the birth of a child, one quarter after surgical manipulations on the cervix. A complete ban on colposcopy is considered to be allergic reactions to the reagents used, adhesions in the vagina that interfere with access to the organ.
You can sign up for a cervical colposcopy after an initial gynecological examination and obtaining the approval of the attending physician, in the absence of obvious contraindications to the procedure.
How is colposcopy done?
If you are having a colposcopy, you already know how to prepare. Let's look at the next important question - how is colposcopy of the cervix done?
How colposcopy is performed is of greatest concern to impressionable women, as well as those who are pregnant, since many of them believe that this procedure is dangerous and very painful. Any gynecologist will confirm the fact that the study is absolutely safe for both the woman and the fetus.
The procedure takes from 10 to 20 minutes. It is carried out only in medical institutions with the participation of a highly qualified gynecologist. There are two types of this study: simple and extended colposcopy. The method for each is slightly different.
So, how is colposcopy of the cervix performed using a simple method? The woman sits on the gynecological chair, as during a routine examination by a gynecologist, after which the doctor, using mirrors, exposes the cervix. Then he uses a tampon to remove any existing discharge. After this, the mucous membrane is examined through a colposcope (this device is large and difficult to miss). This research method can be performed before extended colposcopy.
If the doctor has warned you that he will use an advanced research method, then you will be examined as follows. The inspected part is treated with 3-5% acetic acid, as well as Lugol's solution. The first drug, when exposed to the mucous membrane, causes its slight swelling, which makes it possible to identify the condition of the vessels and evaluate the general appearance of the cells. When applying the medication, a slight burning sensation may be felt; it goes away in a few seconds. The second drug (Lugol's solution) is capable of staining tissues in a dark color - thanks to this, the iodine negative zone is determined during colposcopy. Pathological cells look like light spots against the background of normal tissue.
Specialists can use several solutions to stain tissue (with color colposcopy) or examine the area under ultraviolet rays and apply various preparations to the tissue (with fluorescent colposcopy - for diagnosing cancer). In some cases, the colpomicroscopy method is used. This is a study of part of the tissue under 350x magnification. During the examination, the doctor can also take pathological tissue and send it for analysis (colposcopy with biopsy).
Examination algorithm
Diagnostic testing is performed on an outpatient basis and does not require the patient to be admitted to a hospital. The check is carried out in a gynecological office.
- a standard gynecological chair is used for the procedure;
- a gynecological speculum is inserted into the patient to visualize the uterus;
- the colposcope is located a few centimeters from the entrance to the vagina;
- the organ is treated with a solution of 3% acetic acid, the reaction of the mucosal cells is expected;
- After a short period of time, an iodine solution is applied and the reaction is assessed again;
- a smear is taken;
- a biopsy is taken from questionable tissue areas;
- the procedure is completed by removing excess medication and removing the speculum.
Colposcopy of the cervix practically does not cause any discomfort in women; during the procedure there is no direct contact with the equipment. The duration of the examination does not exceed thirty minutes; after filling out the medical history, the patient can go home.
Is colposcopy painful?
Is it painful to have a colposcopy? This is one of the main questions that women ask their gynecologist. In fact, this procedure does not cause pain, only some discomfort may be felt.
At the beginning of the study, the specialist uses a plastic or metal dilator: he inserts it into the vagina. This allows you to expose the cervix and assess the condition of the tissues, seeing clearly visible general changes. This manipulation is practically painless; only if there is a focus of inflammation, it can cause slight discomfort. To prevent pain, you need to relax and not strain your stomach.
But the colposcopy procedure itself, is it painful? It doesn't hurt at all! Try not to stress yourself out so as not to worsen your moral and physical well-being. Modern equipment and comfortable gynecological chairs, which are made to fit the curves of a woman’s body, allow manipulations to be performed absolutely painlessly.
After colposcopy: norm and deviations
Colposcopy is recognized as a safe procedure that does not cause complications for women’s health. After colposcopy, the patient may experience a slight feeling of discomfort and burning due to the use of acidic reagents in the diagnosis. Scanty spotting for up to 3 days is normal.
Early diagnosis and accurate diagnosis are the key to successful treatment. High-precision equipment and the professionalism of our clinic staff will not leave the disease the slightest chance.
Consequences of colposcopy
You can often hear from women who have visited a gynecologist for this procedure that scarlet discharge appeared after colposcopy or that the lower abdomen began to hurt. When preparing for this type of research, you need to be prepared for consequences and complications, which are rare, but do happen.
Colposcopy is a relatively simple and safe gynecological examination. Only in rare cases can it cause minor harm to health.
A woman may experience a slight discharge after colposcopy mixed with blood, as well as dull aching pain in the lower abdomen (these symptoms in most cases disappear after a few days). Very rarely, the test may lead to an infection in the vagina or cervix.
Consequences of colposcopy in women:
- - heavy or slight bleeding from the vagina;
- - copious vaginal discharge that produces an unpleasant odor;
- — elevated temperature (above 38º C);
- - severe pain in the abdomen;
- - chills
If after colposcopy there is bleeding or other of the above symptoms appear, you should definitely consult a doctor. Similar phenomena can occur after a biopsy.
Gynecologists give some recommendations that should be followed after the examination. Remember, if you bleed slightly after colposcopy, scanty dirty green or dark brown discharge appears and the lower abdomen is tight, do not panic, as this is a completely normal course of events. Such consequences can bother a woman for 5-10 days, after which they simply disappear.
Within 3 weeks after colposcopy you cannot:
- - have a sexual life;
- - use vaginal tampons (give preference to regular pads);
- - do douching;
- — take a bath, go to a sauna or steam bath (showering is allowed);
- - take medications that contain acetylsalicylic acid (aspirin, etc.);
- - engage in intense sports or heavy physical labor.
If your lower abdomen hurts after a colposcopy...
Pain in the lower abdomen after the examination is absolutely normal. However, the pain should go away fairly quickly. If after colposcopy the lower abdomen hurts, while enough time has already passed after the procedure, you need to consult your doctor as soon as possible. He will determine the real cause of the pain and prescribe treatment or recommend special medications for pain relief.
In the first few days after the examination, if you have unpleasant pain in the lower abdomen, you can take regular antispasmodics, for example, paracetamol. They will help eliminate pain and improve well-being. If the drug does not eliminate your symptoms or you have been taking it as needed for more than one day, you should definitely visit your doctor.
How to prepare
Colposcopy is best done 8-12 days after menstruation. Preparing for colposcopy is an important stage; it is important to meet the following conditions:
- Tell your doctor about the medications you are taking and any allergies you have to medications if you have one.
- If you are pregnant or suspect pregnancy, tell your doctor before colposcopy. Most often this is not a contraindication, but the gynecologist should know.
- Do not have sex 1-2 days before the test.
- For 24 hours, do not douche, use tampons, vaginal creams or other products.
- Your bladder should be empty during the test.
- You can take a painkiller 30-60 minutes before. Talk to your doctor about whether you need pain relief.
How often can a colposcopy be done?
The question of how often a colposcopy should be done is best answered by the attending physician, because he is the one who knows the patient’s medical history or complaints.
Colposcopy is a visual examination of the cervix using a special optical device with high magnification and additional lighting. This is just an examination, therefore, according to experts, it can be done at least daily. This is absolutely harmless, although there is simply no point in performing the procedure so often.
In the CIS countries, gynecologists recommend that all women of reproductive age undergo such studies. According to the rules, this must be done at least once a year. These recommendations have a serious basis - recently the incidence of cervical cancer has increased significantly. In addition, timely diagnosis is difficult due to the lack of mandatory cytological screening.
Colposcopy is very important for a woman, as it makes it possible to make a clear diagnosis in the presence of erosion, as well as diagnose the following diseases:
- - inflammatory process in the cervix;
- - leukoplakia;
- - ectopia;
- - cervical cancer or precancerous condition;
- — dysplasia;
- - genital warts and others.
After the colposcopy procedure, interpretation of the results is an important and serious process that is carried out only by an experienced specialist. If colposcopy is unsatisfactory, your doctor may recommend a biopsy. This procedure should not be abandoned. The material obtained during the biopsy is sent to the laboratory, where specialists conduct additional examination using special reagents. This helps determine whether the cells are normal or abnormal. A report with the results obtained is sent to the attending physician. In some cases, laboratory test results may have to wait several days.
How often you have a colposcopy is up to you. Remember how important it is to take care of your body’s health and visit your doctor in a timely manner!
Carrying out colposcopy: duration, stages, tasks
The most informative in terms of assessing the patient’s female health condition is an extended colposcopy. Extended colposcopy refers to a procedure using reagents to detect abnormalities and pathological epithelial changes.
The colposcope is installed in close proximity to the gynecological chair. An appointment with a doctor lasts up to 30 minutes and begins with a standard visual examination performed using mirrors. After a general examination of the cervix, it is treated with a three percent solution of acetic acid, which makes it possible to clearly differentiate the localization of pathologically altered areas. The use of an iodine reagent (Schiller test) makes it possible to identify glycogen-depleted epithelium, signaling precancerous diseases.
If altered areas of the cervix are detected, the doctor takes a biopsy sample. The biopsy is performed with special forceps and can cause discomfort, to avoid which in some cases it is recommended to use a local anesthetic (when taking a sample from the lower part of the vagina).
At the MART clinic on Vasilyevsky Island
- Experienced doctors (including those practicing in the USA and Europe)
- Prices affordable for everyone
- Expert level diagnostics (MRI, ultrasound, tests)
- Daily 8:00 — 22:00
Make an appointment
Where to get a colposcopy in Krasnoyarsk?
In the city of Krasnoyarsk there are many public and private medical institutions where you can undergo gynecological examinations and colposcopy. However, it is important to understand that even an inexperienced gynecologist can conduct a routine examination, while only a professional should perform a colposcopic examination. It is the doctor’s experience that will determine how well he will conduct the examination and how accurately he will determine the diagnosis.
If you are scheduled for a colposcopy, where can you get it done with the most accurate results? Contact a trusted clinic and only an experienced specialist. The Center for Endoscopic Surgery employs professionals who will help you resolve this issue.
The clinic is located at Krasnoyarsk, st. Vesny, 14, room No. 75, tel., 258-18-54. Use the services of professionals and take care of your health!
What do the results mean? What to do if a pathology is detected?
Based on the results of colposcopy, if pathology is detected, the doctor may prescribe treatment or additional examination to clarify the diagnosis. It is important not to let the problem get worse and follow all the gynecologist’s recommendations in a timely manner.
Biopsy results are usually available within ten days. Ask the doctor when the lab report comes back. Based on the results, a final diagnosis will be established, and further treatment tactics will become clear.
At the ProfMedLab clinic you can undergo a colposcopy quickly, without queues, using a modern device. Our doctors carry out the procedure as carefully as possible, we make sure that you are comfortable. Our gynecologist will make an accurate diagnosis and recommend the optimal treatment. Contact us to sign up for the procedure: +7 (495) 120-08-07
Proper nutrition for polyps in the cervical canal
To stabilize the general condition, a woman should follow simple rules:
1. We eat for health. It is necessary to include cereals and legumes in your diet. Among vegetables, you should give preference to carrots, cabbage, zucchini, beets, bell peppers and pumpkin. As for fruits, it wouldn’t hurt to include apples and fenchoya in your diet. Fiber-rich berries include blackberries, strawberries and sea buckthorn. Dairy products can be consumed, but with low fat content.
2. We refuse some products. Margarine will not bring any benefit to a healthy woman, and a patient with cervical canal polyps should absolutely not use it. It is not recommended to get carried away with flour products and sweets. It is better to replace carbonated drinks and coffee with green tea, juices and compotes. Red meat should be excluded from the menu, replacing it with rabbit and poultry meat.
General rules for eating:
- five meals a day in small portions;
- The norm for fat consumption is 100 g per day;
- fluid intake - at least 2 liters per day;
- ban on overeating.
Causes of abdominal pain after colonoscopy
Painful sensations after colonoscopy are quite common; patients usually note that there is pain in the lower abdomen; the unpleasant sensations, which are not too intense, are bursting and pulling in nature.
Pain syndrome occurs as a result of several factors:
- Bloating that occurs as a result of the colon becoming overfilled with gases that are introduced during the procedure to improve vision.
- Irritation of the mucous membrane as a result of exposure to a colonoscope.
- The occurrence of damage to the mucous membrane after medical procedures (biopsy, removal of polyps).
Often, the appearance of pain syndrome is facilitated by impaired motility of the smooth muscles of the intestine. They occur in a small proportion of patients and usually resolve quickly. Usually a muscle spasm develops, which leads to cramping pain of low intensity.