How is cervical cancer diagnosed?
Despite the fact that screening for early diagnosis of cervical cancer has been developed, the mortality rate from this disease remains high. It is rarely detected on time. Although it takes years for the tumor to reach the stage of invasion, during this time precancerous processes can be identified if the woman undergoes regular examinations with a gynecologist.
If cervical cancer is suspected, diagnosis includes:
- Smear for oncocytology - for screening detection of pathological changes in the epithelium
- Colposcopy – if changes are detected in the smear
- Blood tests for tumor markers
- Biopsy of a suspicious lesion
Imaging methods are also important in diagnosing cervical cancer. These are ultrasound, x-ray, CT, MRI. But they are not used for the initial detection of a tumor, but to establish the extent of the oncological process and determine the stage of cancer.
Possibilities of modern ultrasound techniques in the diagnosis of endometrial cancer
Ultrasound scanner HS70
Accurate and confident diagnosis.
Multifunctional ultrasound system for conducting studies with expert diagnostic accuracy.
Introduction
According to world statistics, uterine cancer ranks 7th among malignant diseases. An analysis of the oncological situation in the last decade in Russia indicates a steady increase in the incidence of endometrial cancer, which by 2007 took 2nd place among all malignant tumors in women. The share of uterine cancer in the structure of the incidence of malignant neoplasms per 100,000 female population of Russia in different regions ranges from 4.5 to 22.5. There is a steady increase in the incidence rate from 9.8 in 1990 to 13.9 in 2005, which corresponds to the 3rd place in terms of the increase in the incidence of malignant neoplasms [1]. Currently, the increase in the number of newly diagnosed cases of uterine cancer is not inferior to that of breast tumors. In third world countries, the risk of developing endometrial cancer is generally lower, but the mortality rate remains high. In North America and Europe, this disease is much more common, being the most common malignant tumor of the female reproductive system, and ranks 4th among all malignant neoplasms after breast, lung and colon cancer. The incidence of endometrial cancer increases sharply between the ages of 40 and 54 years, with the peak incidence occurring between the ages of 60 and 64 years. The incidence of endometrial cancer and its dynamics in different countries, taking into account the influence of migration processes and age, indicate the specific features of the disease and the dependence of its occurrence on a complex of causes of endo- and exogenous nature [2].
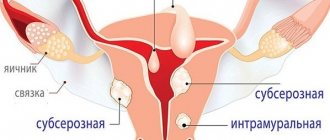
Among the risk factors for the development of uterine cancer, attention is drawn to a low number of births or infertility, obesity, late menopause, and diabetes mellitus, mainly type 2. In most cases, the risk of developing endometrial cancer is associated with various forms of endometrial hyperplasia - 81.3%, dysfunction due to polycystic ovary syndrome - 25%, endometrial polyposis - 5.3-25%, uterine fibroids - 1.6-8%. Recently, there has been a significant increase in locally advanced forms of endometrial cancer, which is associated with ineffective primary diagnostic measures. Issues of clarifying diagnosis of endometrial cancer are the subject of close study [3].
In the pathogenesis of the disease, the theory of excessive estrogen stimulation of the endometrium, combined with progesterone deficiency, is of leading importance. It is believed that excessive estrogen exposure can lead to endometrial hyperplasia, which can progress to an atypical variant and in 20-25% of cases to transition to adenocarcinoma. At the same time, the existing relationship between the degree of endometrial proliferation and the concentration of estrogen in the blood is observed up to a certain threshold value, and even intense proliferation is not in all cases accompanied by malignant transformation of the endometrium. The discovered correlation between estrogen content and DNA damage in normal and malignant endometrium forces us to pay more attention to the role of molecular genetic and morphological factors in the formation of different types of uterine cancer. Endometrial cancer is characterized by a heterogeneous nature, which manifests itself at the level of both risk factors and its pathogenesis, which determines the features of the formation of risk groups for this disease.
Currently, to identify endometrial pathology, diagnostic curettage of the uterine cavity, hysteroscopy and aspiration cytological examination, as well as radiation diagnostic methods, among which ultrasound (US) is of leading importance, are mainly used [4-6]. However, there are no uniform methodologically based echographic criteria for invasive tumor growth. The introduction of new ultrasound technologies into programs for integrated examination of patients, such as pulsed Doppler, ultrasound angiography and three-dimensional image reconstruction, has significantly increased the efficiency of primary diagnosis and monitoring of patients with endometrial cancer in the process of specific therapy [7, 8].
The purpose of this work was to study the capabilities of complex ultrasound using color Doppler and energy mapping (CDC and EC), pulsed Doppler and three-dimensional image reconstruction in the primary and clarifying diagnosis of endometrial cancer.
Material and methods
We examined 139 patients aged from 21 to 87 years with suspected endometrial cancer in the peri- and postmenopausal period. In 34 patients, hyperplastic processes of the endometrium were detected, in 105 - malignant processes of the endometrium. The average age of patients with benign pathology was 42.6±7.2 years, of patients with endometrial cancer - 65.4±7 years. In all cases, histological verification of the diagnosis was obtained.
All patients were comprehensively examined by ultrasound using transabdominal (3.5 MHz convex sensor) and transvaginal (6.5-7 MHz sensor) approaches on modern ultrasound machines Logiq S6 (GE, Healthcare) and Accuvix-XQ (Medison) according to a certain program using the latest ultrasound techniques, including Doppler ultrasound of the uterine vessels, color circulation and EC with three-dimensional image reconstruction. During transabdominal examination in patients with a full bladder, the condition of the uterus and ovaries was assessed, the volumes of the body and cervix, and the width of the M-echo were determined. During transvaginal ultrasound (TVUS), Doppler measurements were used to measure blood flow and resistance index in the uterine arteries, and to evaluate the intensity of intratumoral blood flow. At all stages of the study, the state of the endo- and myometrial structure, their relationship and homogeneity were determined. When focal changes were detected, their size, extent of prevalence and relationship with surrounding organs and structures were determined, and a comparative assessment of the thickness of the uterine wall in the tumor area and outside the area of the tumor focus was carried out. If possible, the linear and volumetric parameters of the tumor, the clarity of its contours were accurately determined, and the condition of the adjacent mucous membrane was assessed. The main parameter for assessing the endometrium remains the change in its thickness [9]. Endometrial volume is also used for the earliest diagnosis of the disease. Its values are more reliable in the differential diagnosis of cancer and benign hyperplastic processes than measurements of endometrial width. The criteria for malignant endometrial lesions are endometrial volume values exceeding 13 cm3. This ensures 100% sensitivity and 92% predictability of a positive test in the diagnosis of endometrial cancer [10].
The most important characteristics of an endometrial neoplasm were the degree and nature of its vascularization, which was assessed in the cine-loop mode in order to obtain the most complete and visual representation. A qualitative assessment of blood supply was carried out according to the number of color signals from the vessels of the neoplasm: hypovascular, moderately vascular, hypervascular. We used Multi-Slice View technology to convert volumetric data into a series of sequential slices up to 0.5 mm thick. Purposeful selection of certain sections from 3D volumetric data made it possible to select optimal sections of the body and uterine cavity and estimate their sizes as accurately as possible, and determine the relationship of the identified changes with the condition of surrounding organs and tissues. Volume CT View technology made it possible, based on 3D scanning, to evaluate the contours and structure of the endometrium, the nature of its blood supply, and the use of the histogram option made it possible to accurately determine the vascularization index [11].
Particular attention was paid to assessing the depth of myometrial invasion, the possible transition of the malignant process to the cervical canal and the condition of the regional lymph nodes, which was crucial in determining the stage of the disease and choosing treatment tactics [12].
Results and discussion
As a result of the study, endometrial hyperplastic processes were identified in 34 patients, which we identified into separate nosological forms that comply with WHO recommendations. In table Figure 1 shows the distribution of patients depending on the morphogenesis of the identified endometrial hyperplastic processes.
Table 1
. Distribution of patients according to the type of endometrial hyperplastic processes.
| Number of patients | ||
| abs. | % | |
| Morphological form of endometrial hyperplastic processes | 34 | 100 |
| Glandular cystic hyperplasia | 19 | 56 |
| Glandular fibrous polyps | 5 | 15 |
| Atypical hyperplasia | 10 | 29 |
Hyperplastic processes of the endometrium were manifested by menstrual cycle disorders such as menometrorrhagia, anemia of I-II degrees. In case of benign endometrial pathology, in 24 (71.4%) patients, an increase in the thickness of the M-echo on average was determined by gray scale ultrasound of 14.6 ± 3.2 mm. With transvaginal echography, glandular cystic hyperplasia was defined as the formation of increased echogenicity, a homogeneous structure, with multiple point hypo- or anechoic inclusions up to 1.5 mm, sometimes with an acoustic amplification effect. With atypical hyperplasia, a heterogeneous hyperechoic solid structure was detected in the uterine cavity. Polyps were defined as round, oval or oblong, in some cases on a long stalk, hyperechoic formations of various sizes, deforming the uterine cavity and clearly differentiated against the background of the liquid contents of the uterine cavity. Using pulsed Doppler mode, hemodynamic parameters in the uterine arteries were quantitatively assessed, which were: MSS - 9.3±2.1 cm/s, resistance index - 0.56±0.05 [13].
Using the color Doppler technique, intratumoral blood flow in glandular cystic hyperplasia was recorded in the form of single signals from vessels located along the periphery. In fibroglandular polyps, moderately pronounced venous and arterial peripheral blood flow with average values of peripheral vascular resistance was visualized. In 2 patients with glandular hyperplasia, pronounced hypervascularization of the endometrium was determined. In atypical hyperplasia, central and peripheral intratumoral blood flow of moderate intensity was recorded. In 5 patients with glandular cystic hyperplasia and atrophic endometrium, blood flow was not recorded. Characteristic signs of a benign neoplasm, even in the presence of multiple polypoid growths, were the preservation of the shape of the uterine cavity, a clear definition of the outer contour of the endometrium and a uniform distribution of myometrial vessels (Fig. 1 and 2).
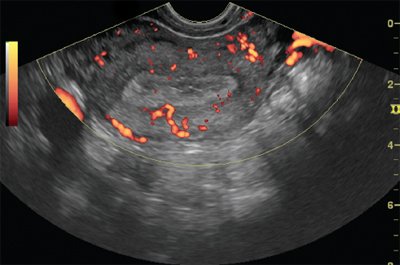
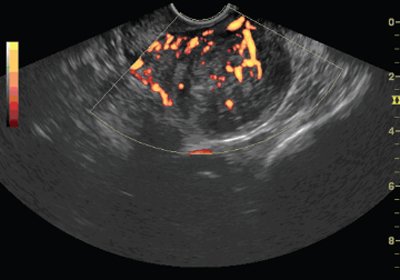
Rice. 1.
TVUS, energy mapping mode. Glandular cystic endometrial hyperplasia.
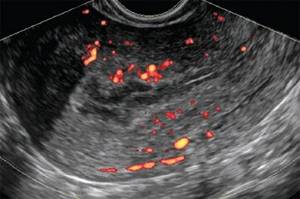
Rice. 2.
TVUS, energy mapping mode. Endometrial polyp.
Malignant endometrial pathology was diagnosed in 105 patients. 80% of those examined with this pathology were aged from 50 to 69 years, of which 82 (78%) had malignant transformation of the endometrium accompanied by postmenopausal bleeding. An examination of patients with suspected endometrial cancer revealed an increase in the thickness of the M-echo to 18.1±6.7 mm. At stage Ia, the thickness of the M-echo was 11.5±3.7 mm, at stage Ib - 15.8±8.4 mm, at stage Ic - 17±3.4 mm, at stage II - 21±4.1 mm, at stage III - 27±2.0 mm, at stage IV - more than 30 mm. The stage of uterine cancer was determined according to the International Classification of Cancer (FIGO, 1988). In table 2, a comparison was made of a specific histotype of endometrial cancer with the stage of the disease.
table 2
. Comparison of histotype and stage of endometrial cancer.
| Tumor histotype | Stage | Total | |||||
| Ia | Ib | Ic | II | III | IV | ||
| Adenocarcinoma: | |||||||
| highly differentiated | 12 | 3 | 3 | 4 | 2 | 1 | 25 |
| moderately differentiated | 22 | 6 | 2 | 6 | 6 | 2 | 44 |
| low-grade | 5 | — | — | 1 | 3 | 1 | 10 |
| serous-papillary | 3 | — | — | 1 | 3 | 1 | 8 |
| clear cell | — | 1 | — | — | — | 1 | 2 |
| Glandular squamous cell carcinoma | 1 | 1 | — | 2 | 1 | — | 5 |
| Sarcoma | 2 | — | 1 | 1 | 3 | 2 | 9 |
| Acanthoma | 1 | 1 | — | — | — | — | 2 |
| Total | 46 | 12 | 6 | 15 | 18 | 8 | 105 |
As can be seen from table. 2, more than 60% of patients were diagnosed with stage I uterine cancer, with 46 patients having stage Ia. Patients with common forms of malignant diseases of the uterine body accounted for 23%. In most cases (89 patients, 85%), adenocarcinoma of varying degrees of differentiation was diagnosed.
In our study, the degree of tumor differentiation correlated with the stage of the disease: in highly differentiated adenocarcinoma, the process was mainly limited to the uterine body. Poorly differentiated, serous papillary and clear cell adenocarcinomas were noted at stages II, III and IV with tumor spread beyond the organ. Squamous cell carcinoma of stage I was diagnosed in 2 patients, stages II and III - in 3. A combination of adenocarcinoma and endometrial stromal sarcoma was detected in 9 patients, of which 5 were diagnosed with stages III and IV of the disease. The main ultrasound signs of endometrial cancer during transabdominal and transvaginal studies in B-scan mode can be considered an increase in M-echo, which is not typical for this patient, unevenness and heterogeneity of the endometrium, in addition, a higher echogenicity of its structure as a whole or the identified focal formation compared with unchanged myometrium, the presence of an uneven, external contour penetrating into the myometrium to varying depths. In cases of significant local spread of the tumor, visualization of a hypoechoic rim around the tumor or the absence of a border between the tumor focus and the myometrium is possible. In our study, we assessed the invasive growth index (IGI) - determining the ratio of the volume of the altered endometrium (AVI) to the volume of the uterine body. The obtained data are presented in table. 3. Calculation of these indicators was possible only for stage I endometrial cancer, when the border of the altered endometrium was defined quite clearly (Fig. 3).
Table 3
. Ultrasound parameters of the uterus and M-echo in endometrial cancer of different stages.
| Stage | Uterine volume, cm3 | Endometrial volume, cm3 | IIR |
| Ia | 50±15,1 | 4,2±2,2 | 11,9±4,2 |
| Ib | 62±10,4 | 8,3±4,6 | 7,5±5,4 |
| Ic | 67±4,1 | 15,4±5,3 | 4,3±2,9 |
| II | 76±14,7 | — | — |
| III | 80±10,1 | — | — |
| IV | 88±13,6 | — | — |
At stage Ia, the volume of the endometrium was 4.2±2.2 cm3, IIR - 11.9±4.2, at stage Ib AIE - 8.3±4.6 cm3, IIR - 7.5±5.4 cm3, at stage Ic, AIE is 15.4±5.3 cm3, IIR is 4.3±2.9. As shown in the table. 3 data, there is a clear increase in endometrial volume and a decrease in IRI values as the degree of tumor invasion in the myometrium increases. For the majority of patients with endometrial cancer, its localization was characteristic of the fundus of the uterus or one of the tubal angles. Tumor necrosis with deformation of the uterine cavity and the presence of fluid in it were determined at stages III and IV of the process.
Rice. 1.
TVUSI, B-mode. Stage Ib endometrial cancer. Determination of the endometrial invasion index.
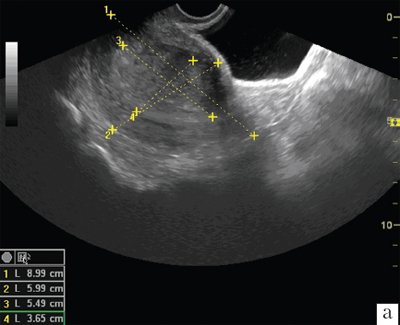
A)
Longitudinal scanning.
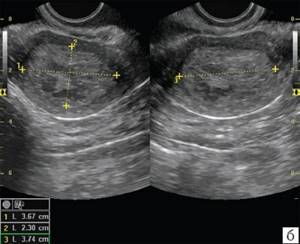
b)
Transverse scanning.
Based on literature data, we have identified three main types of growth of invasive endometrial cancer.
- Development of multiple highly differentiated tumor foci against the background of hyperplastic processes of the entire endometrium.
- Development of one highly differentiated tumor focus, surrounded by a hyperplastic mucous membrane over a short area.
- Development of one moderately or poorly differentiated tumor focus against the background of an atrophic mucous membrane.
The exophytic form of tumor growth was detected in 15% of cases. Exophytic tumor growth is characterized by the absence of deformation of the uterine cavity, clear boundaries of the endo- and myometrium, or the detection of a formation in the lumen of the uterine cavity. In 85% of cases, an endophytic form of growth with invasion into the myometrium was noted. Violation of the integrity of the hypoechoic rim in endometrial cancer is a specific sign of invasion into the myometrium. Endophytic tumor growth leads to asymmetry and deformation of the uterine cavity. With a deep infiltrative process, the 2nd option was noted in 30%, the 3rd option - in 70% of cases. Ultrasound made it possible to clearly determine the shape of tumor growth only in the initial stages of the disease. In stage Ia endometrial cancer, in the case of ultrasound in B-mode, a homogeneous hyperechoic structure of the median M-echo was determined, and in 69.5%, heterogeneity of the endometrial structure was revealed due to inclusions of a round shape, with smooth, in some cases unclear contours, increased echogenicity, the average size of which was 6.3±3.8 mm. The boundaries of the endometrium in all observations at stage I of the disease were determined to be clear and even.
Table 4
. Hemodynamic parameters in benign and malignant pathology of the endometrium.
| Index | Endometrial hyperplasia | Endometrial cancer |
| Uterine arteries | ||
| MSS, cm/s | 50±14,2 | 65,4±16,3 |
| IR | 0,82±0,07 | 0,79±0,07 |
| Intratumoral vessels | ||
| Hemodynamic parameters | No or peripheral blood flow | Intense blood flow - central and peripheral |
| MSS, cm/s | 9,3±1,3 | 10,2±4,1 |
| IR | 0,56±0,05 | 0,36±0,05* |
Note. * — p<0.05
In our observations, it was possible to differentiate the 1st and 2nd types of tumor development in the usual B-mode only in 10 patients. In other cases, due to significant local spread of the tumor, these differences were not determined. With a deep infiltrative process at stages III and IV of the disease, the thickness of the M-echo exceeded 27.0 mm. The boundaries between the tumor and myometrium in all cases were unclear, the contours were uneven, and in 61 (58.0%) patients the tumor boundaries were not defined up to the outer contour of the uterus. The structure of the M-echo in 30.3% of cases was homogeneous hyperechoic, in 20.1% - homogeneous hypoechoic, and in 50% - heterogeneous, predominantly hyperechoic. The echostructure of the tumor could also have different echogenicity: in 44.6% of cases it was homogeneous hyperechoic, in 10.4% - homogeneous hypoechoic, in 45.0% - mixed.
We assessed quantitative hemodynamic parameters using pulsed Doppler ultrasound in the uterine arteries and tumor vessels [14]. In table Table 4 shows a comparative description of hemodynamic parameters in benign and malignant endometrial pathologies.
As can be seen from the data presented, the hemodynamics of regional blood flow in endometrial cancer is accompanied by a tendency to increase the speed of blood flow in the vessels of the uterus and a statistically significant decrease in the index of peripheral resistance in tumor vessels, which can characterize the activity of intratumoral blood flow. MSS in the uterine arteries depended on the volume of the uterine body, which could be associated with the presence of fibroids, and the nature of tumor vascularization. The indicators of intratumoral blood flow and IR were not statistically dependent on the histotype of endometrial cancer.
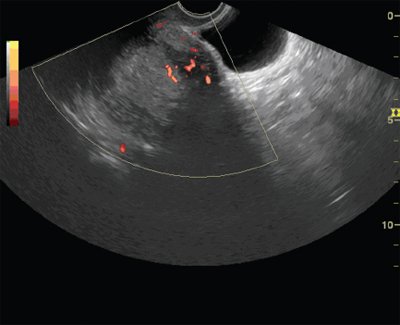
Rice. 4.
TVUS, energy mapping mode. Endometrial cancer stage Ia. A focus of hypervascularization is identified along the anterior wall of the uterus.
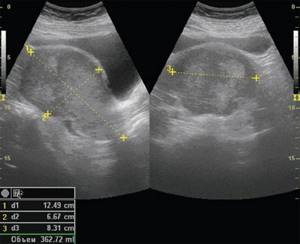
Rice. 5.
Ultrasound, B-mode, transabdominal scanning, stage IV endometrial cancer.
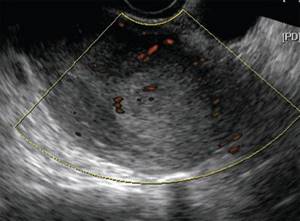
Rice. 6.
TVUS, Color Doppler, Longitudinal Scanning. Endometrial cancer stage Ia. Infiltrative formation of a hyperechoic structure in the area of the fundus of the uterine body with reduced vascularization.
When analyzing the nature and degree of vascularization of endometrial cancer, assessed using the CDC and EC modes, different options for intraendometrial blood flow were determined. Pathological vascularization of the endometrium occurred in 92 (87.6%) patients with endometrial cancer. In other cases, even in the presence of characteristic ultrasound signs of malignant lesions, intratumoral blood flow was not visualized using the techniques used. In case of a tumor of the uterine body, three main variants of blood supply were identified (A, B, C), and a certain dependence of the pattern of color circulation and EC with the stages and identified forms of tumor growth was observed. The intensity of blood flow in the endometrium and tumor node, determined in the CDC and EC modes, depended on the type of tumor growth and could be most clearly presented in the cine-loop mode. Zones of tumor blood flow are detected in endometrial cancer in more than 90% of cases (Fig. 4-8).
It was established that option A was characteristic of stage Ia: with infiltration of the myometrium to a depth of 5 mm, which was determined in 33.8% of cases and was characterized by an uneven increase in intraendometrial blood flow due to a local increase in the number of color spots with different color intensities, in the absence of color loci in the subendometrial zone. The same variant was characteristic of the exophytic form of growth with an intratumoral type of neovascularization.
Rice. 7.
TVUSI, CDC. Stage IV endometrial cancer. Hypervascularization of the formation of a heterogeneous structure in the area of the left uterine angle. Endometrial and intratumoral blood flow is determined.

Rice. 8.
TVUS, combination of B-mode and energy mapping mode. Stage IV endometrial cancer. A focus of hypervascularization along the posterior wall of the uterus with hypervascular endometrial blood flow.
Option B (47.6%) was characterized by a total increase in intraendometrial blood flow due to a large number of chaotically located color loci, with a simultaneous local increase in the number of color signals in the subendometrial zone. In 27.5% of cases, moderate vascularization of the tumor was determined, combined with rich vascularization of the myometrium. This variant was identified in 78.3% of patients with a mixed form of endometrial cancer.
Option C (19.6%) was characterized by a slight increase in intraendometrial blood flow with a significant total increase in the number of color signals in the subendometrial zone. This variant was characteristic of the endophytic growth form (92.5%) and was accompanied by intense intra- and peritumoral blood flow.
Although no direct correlation was established between the severity of tumor blood flow and the stage of the disease, as well as the degree of differentiation, the presence of a detectable zone of neovascularization corresponded to a higher stage of the process. Hypovascular and moderate blood flow in the endometrium was observed in patients with well-differentiated adenocarcinoma.
Color Dopplerography did not register neovascularization of the pathological process in 12.4% of cases. The reason for this could be the removal of a small tumor as a result of preliminary diagnostic curettage of the uterine cavity and in highly differentiated adenocarcinoma that arose against the background of endometrial atrophy.
Three-dimensional echography, due to the construction of frontal planes, made it possible to more accurately determine the state of the endometrium and establish its asymmetry. A disorganized vascular pattern, revealed by three-dimensional angiography in a volumetric block, when combining scanning modes, was an important additional sign of malignant endometrial lesions. The most accurate results in assessing the degree of invasion of endometrial carcinoma are achieved using three-dimensional reconstruction in ultrasound angiography mode (Fig. 9-11). An important sign of common invasive processes is the presence of zones of local increased vascularization in the myometrium adjacent to the tumor areas.
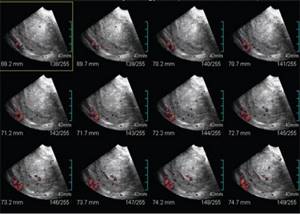
Rice. 9.
Ultrasound performed using Multi-slice view technology. Using layer-by-layer sections, it becomes possible to accurately determine the structure of the endometrium and its vascularization.
The capabilities of the ultrasound method in diagnosing endometrial cancer have their limitations due to the fact that hyperplastic processes and the initial stages of the disease do not have specific differential diagnostic features. Concomitant uterine bleeding with the formation of fibrin complicates the identification of areas of endometrial thickening. Certain difficulties arise in determining the depth of myometrial invasion in the initial stages of endometrial cancer within limits of up to 5 mm, as well as in cases of concomitant adenomyosis. Ultrasound does not accurately determine the volume of cancerous lesions in women with large and multiple submucosal myomatous nodes that deform the uterine cavity.
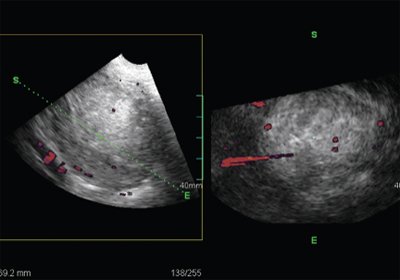
Rice. 10.
TVUS, energy mapping mode. Ultrasound performed using Oblique view technology. 3D volumetric data allows us to clarify the state of the endometrium and the nature of endometrial and subendometrial vascularization.
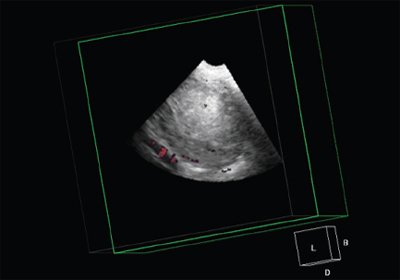
Rice. eleven.
Multi-plane reconstruction mode. Volume CT view. 3D data allows you to determine volumes as accurately as possible.
conclusions
Ultrasound examination using pulsed Doppler, color Doppler, energy mapping and three-dimensional image reconstruction is a highly informative method for non-invasive clarifying diagnosis of endometrial pathology. The results obtained indicate the high efficiency of the methods used in the differential diagnosis of benign and malignant processes. Ultrasound angiography and three-dimensional image reconstruction for endometrial cancer help obtain additional and very important information about the characteristics of the tumor process, the depth of tumor invasion into the myometrium, and the nature of the detected neovascularization makes it possible to predict the rate of tumor growth.
The use of modern ultrasound technologies makes it possible to solve the problems of intranosological diagnosis of endometrial cancer at a completely new qualitative and quantitative level, as well as to monitor patients in the process of specific treatment.
Literature
- Davydov M.I., Aksel E.M. Statistics of malignant neoplasms in Russia and the CIS countries in 2005 // Bulletin of the Russian Oncological Research Center named after. N.N. Blokhin RAMS. 2007. T. 18.
- Urmancheeva A.S., Tyulyandin S.A., Moiseenko V.M. Practical oncogynecology (Selected lectures) // M.: Publishing house. "MEDpress-inform". 2005. 264 p.
- Titova V.A., Kharchenko N.V., Stolyarova I.V. Automated radiation therapy of the female reproductive system // M.: Medicine. 2006. 160 p.
- Gruboeck K., Jurkovic D., Lawton F. et al. The diagnostic value of endometrial thickness and volume measurements by three-dimensional ultrasound in patients with postmenopausal bleeding // Ultrasound Obstet. Gynecol. 1996. No. 8. P. 272-276.
- Stolyarova I.V., Minko B.A., Lisyanskaya A.S. and others. Possibilities of modern ultrasound techniques in the clarifying diagnosis of endometrial cancer // International Congress Nevsky Radiological Forum “New Horizons” April 7-10, 2007 St. Petersburg, pp. 364-365.
- Chekalova M.A., Zuev V.M. Ultrasound diagnostics in gynecological oncology // M.: Publishing House. house "Russian doctor". 2004. 92 p.
- Teregulova A.E. Transvaginal echography using color Doppler mapping in patients with endometrial cancer // Ultrasound diagnostics. 1996. No. 4. pp. 21-23.
- Kurjak A., Shalan H., Sosic A. et al. Endometrial carcinoma in postmenopausal women: evaluation by transvaginal color Doppler ultrasonography // Am. J. Obstet. Gynecol. 1993. V. 169. P. 1597-1603.
Ultrasound scanner HS70
Accurate and confident diagnosis.
Multifunctional ultrasound system for conducting studies with expert diagnostic accuracy.
What is cervical cancer screening?
Cervical cancer is the third most common cancer among women. Therefore, its screening (mass) diagnosis has been introduced everywhere. The essence of such an examination is that it begins not after the onset of symptoms, but against the background of health. That is, when there are no signs of the disease yet. Any woman, 3 years after the start of sexual activity, should have her first smear test for cervical cancer. A year later, he is tested again, since it is not always possible to diagnose cervical cancer with a smear. The sensitivity of the test averages 85-90%. This means that in case of pathological changes in the epithelium, the smear will show normal results in 10-15% of cases.
Main reasons:
- Pathologically altered cells may not be included in the clinical sample
- The doctor may not cover the affected area
- If atypical cells are present on the spatula, they do not always fall from it onto the glass slide
- Evaluation of the cytological picture may be erroneous (human factor)
In old age, screening diagnostics are usually stopped. This is possible if the woman is over 70 years old and has had at least 3 negative oncocytology smears within the last 10 years.
Kidney tumors and causes of their development
A kidney tumor is a pathological process characterized by the proliferation of tissue consisting of qualitatively changed cells. Depending on the nature of growth, benign and malignant neoplasms are distinguished. The latter are more common and account for about 94–95% of all detected tumors. The average age of detection of kidney tumors is 70 years. According to statistics, tumors occur 2 times more often in men than in women. In children they are detected with a frequency independent of gender. Factors contributing to the development of tumors in the kidneys include:
- hereditary causes;
- bad habits (smoking, drinking alcohol);
- exposure to radiation or carcinogenic substances;
- disruptions in the immune system;
- the presence of chronic foci of infection in the body or kidneys.
Physical examination
If the laboratory test for cervical cancer is positive, confirmatory tests are required. After all, a smear on the date is only an approximate result. The next stage of cervical cancer screening is colposcopy. This is an examination of the mucous membrane using a special optical device that magnifies the image tens of times. Thanks to colposcopy, the doctor can detect not only cancer, but also background and precancerous diseases.
Extended colposcopy has the greatest diagnostic value. Its essence is that the cervix is treated with various substances. Most often it is acetic acid or iodine with glycerin, but there are other tests. All of them show what reaction certain substances cause in tissues. A biopsy is then taken from the suspicious area - this is the main way to detect cervical cancer.
Clinical examination also plays an important role in diagnosing the disease. Women often ask whether cervical cancer can be felt with a finger. Yes, you can find it. However, in this case we are not talking about early diagnosis. Only if the tumor is large is it accessible to palpation.
Send a request for treatment
Symptoms indicating the possible presence of a malignant neoplasm
Treatment of malignant tumors in the kidneys is most effective in the initial stages. But during this period, the neoplasm usually does not manifest itself in any way. A doctor may accidentally detect a kidney tumor on a routine ultrasound even in the complete absence of clinical signs of the disease. As the tumor grows, symptoms appear that indicate a deterioration in the patient’s general condition: nausea, weakness, loss of appetite, sudden weight loss. Blood in the urine, complaints of pain in the lumbar region, swelling in the sides of the abdomen, and renal colic are more likely to indicate that the kidney tumor has reached an advanced stage.
What tumor marker indicates cervical cancer?
Tumor markers are chemical compounds that are detected in the blood for various types of cancer. The main tumor marker for cervical cancer is SCC Ag (squamous cell carcinoma antigen). It is not used for screening diagnosis of the disease. Because it is inferior in sensitivity and specificity to a cytological examination of a smear from the cervix. Therefore, a tumor marker for cervical cancer is determined only for preclinical diagnosis of relapse or to assess the effectiveness of therapy.
SCC Ag is increased in any squamous cell carcinoma, regardless of its location. Therefore, an increase in its level may indicate an oncological neoplasm:
- Esophagus
- Lung
- Heads and necks
- Rectum, etc.
The tumor marker for cervical cancer can also increase in non-tumor diseases. These include tuberculosis, dermatological pathologies (psoriasis, eczema, lichen planus and others), kidney or liver failure. Even a positive result of a blood test for tumor markers for cervical cancer does not indicate the disease. Likewise, negative does not clearly indicate the absence of cancer pathology.
The data obtained during the study is assessed:
- Dynamics (a series of analyzes at certain intervals)
- In combination with other research methods
Thus, a blood test for cervical cancer is indicative, not confirmatory. It is not used for early diagnosis of the disease. At stage 1 cervical cancer, testing for squamous cell carcinoma antigen will give positive results in only 15% of cases. Only in late stages or when the tumor recurs is high sensitivity of the diagnostic test observed, which can reach 90-95%.

Types of stomach cancer
The overwhelming majority, about 90% of all clinical cases, are adenocarcinoma.
In addition to adenocarcinoma, there are other types of stomach tumors:
- Squamous cell carcinoma.
- Differentiated gastric cancer.
- Glandular squamous cell carcinoma, etc.
According to growth forms, they are distinguished:
- Fungal tumors. Such a tumor is prone to late metastasis, has exophytic growth, and is clearly demarcated from surrounding tissues.
- The tumor is ulcerated. It has a saucer shape with a recess in the center. Just like in the first case, it is clearly demarcated from the surrounding tissues and metastasizes late.
- Ulcerative-infiltrative tumor. It grows through the walls of the organ and has no clear boundaries.
- Diffuse infiltrative tumor. It is a mixed form. It has the appearance of numerous ulcerations and is prone to infiltrative growth.
Based on the location, there may be:
- Tumor of the fundus of the stomach.
- Front wall.
- Rear wall.
- Cardiac zone.
- Small curvature.
- Great curvature.
- Pyloric part.

What test should you take for cervical cancer?
The main test for cervical cancer is a cytological examination of a stained smear taken from the cervical canal. It has many advantages.
This study:
- Simple
- Inexpensive
- Fast - Once doctors test for cervical cancer, results can be obtained the same day or the next
- Painless - does not require either general or local anesthesia
- Does not harm health, and therefore can be performed with any frequency
- Has high sensitivity and specificity for a screening method
Tests for cervical cancer should be taken regularly. If they are all negative, it is enough to do research once every 3 years, starting from the age of 21. But if background and precancerous processes are detected, more frequent monitoring is required. The study will have to be completed annually. However, for most women this is not a problem. Considering how much a cervical cancer test costs, screening will not be financially burdensome.
The importance of a smear for oncocytology can hardly be overestimated. In developed countries, this test detects stage 0 or stage 1 cervical cancer in 70-80% of cases. That is, only 20-30% of women have the disease at stage 2 and above. In this case, the prognosis of the pathology is much worse. The likelihood of a complete cure is low.
Women often ask what blood test shows cervical cancer. There are several tests that help in diagnosis. For early detection of pathology, a blood test using PCR for oncogenic types of papillomavirus is used. If they are detected, the woman is monitored, since she is at risk for cervical cancer.
For patients who are already being treated for cancer, it is possible to take a test for cervical cancer to determine tumor markers in the blood. An increase in their concentration indicates the ineffectiveness of treatment or relapse of the tumor. A decrease in the amount of squamous cell carcinoma antigen indicates the success of therapy or ongoing remission of the cancer.
Prevention of stomach cancer
Prevention involves changing your diet. It should contain more plant foods. Do not overuse smoked, fried and fatty foods. They have carcinogenic properties. You should also not overeat. Nutritional causes account for about 35% of all cancer cases.
It is necessary to give up alcohol abuse and smoking. It is also important to promptly treat inflammatory diseases of the stomach, such as gastritis. Chronic inflammation is fertile ground for the development of stomach cancer.
Stomach cancer is a serious and extremely dangerous pathology. To treat it, it is necessary to make every effort, but this is not always justified. It is much easier to prevent a terrible disease. To do this, it is enough to follow these recommendations and undergo preventive examinations every year.
Can cervical cancer be seen on an ultrasound?
Ultrasound is one of the most commonly used diagnostic methods in gynecology. Using ultrasound, it is possible to visualize all internal genital organs. Therefore, patients often ask whether cervical cancer can be seen on an ultrasound. Yes, theoretically this is possible. But in practice, ultrasound is not used in the primary diagnosis of cervical cancer. The location of the tumor allows it to be seen without the use of imaging methods. After all, the cervix is not hidden from view by other tissues.
Can cervical cancer be detected by ultrasound? No you can not. Theoretically, if an ultrasound examination is performed, the doctor will only see a tumor-like formation. But whether it is cancer or not can only be determined with the help of a biopsy.
If cervical cancer is suspected, a woman undergoes a simple and extended colposcopy. Then a tissue sample is taken from the detected suspicious area of the mucous membrane, which is sent for histological examination.
Differentiation of neoplasms by ultrasound examination
Benign kidney tumors. Such neoplasms look like round echogenic space-occupying formations, usually small in size.
Malignant kidney tumors. A common sign indicating their presence is the detection of space-occupying formations with high echogenicity. Unlike cysts, they do not have a capsule, and their edges are always uneven. Sometimes it is possible to visualize a hypoechoic pseudocapsule formed by renal parenchyma compressed around the tumor. In some cases (10–20% of the total), calcifications are detected in neoplasms (in the form of extremely echogenic central or peripheral areas). Sometimes the tumor has necrotic areas or hemorrhages. They are visualized as hypoechoic areas on a hyperechoic background. As the tumor grows, its contours on ultrasound extend beyond the contour of the kidney.
Metastases. These malignant neoplasms are usually found in the cortex. Metastases can be found in one or both kidneys. Such tumors have the appearance of hypoechoic space-occupying formations of various sizes and shapes.
How is cervical cancer determined?
In the process of primary diagnosis, a cytological examination of a smear helps determine cervical cancer. However, this test is not confirmatory. To establish a final diagnosis, histological examination of the tissue must be performed. It differs from cytology in that it is not individual cells caught in the sample that are studied, but a fragment of tissue.
Cervical cancer can be detected using the following types of biopsy:
- Colposcopic biopsy - using special forceps, 2-3 mm of tissue is removed in the suspicious area.
- Endocervical curettage (curettage) - used if the suspicious area is not located in the endocervix. It is not accessible to the colposcope. In this case, curettage is performed using a curette, and the resulting material is sent for histological examination.
- A cone biopsy is a surgical procedure in which a cone-shaped area of the cervix is removed. It is both treatment and diagnosis. The method preserves a woman's fertility.
All these methods allow you to recognize cervical cancer. Thanks to them, a primary diagnosis is established. Then studies are required to assess the prevalence of the cancer process.
Indications for ultrasound
Ultrasound examination of the kidneys is recommended periodically for people of any age, even in the absence of signs of illness. It is also indicated for those who do not suffer from diseases of the urinary system. In addition, the procedure is recommended if symptoms such as:
- abnormalities in urine tests;
- palpation of a tumor in the kidney during a medical examination;
- regular aching or sharp pain in the lumbar region;
- frequent increases in blood pressure;
- renal colic;
- regular headaches (if their origin is not determined during the examination);
- severe swelling of the lower extremities or face;
- injuries or bruises in the kidney area;
- the presence of chronic and acute inflammatory diseases of nonspecific and specific types.
Instrumental diagnostics
There are many tests that can be used to determine the stage of the disease. These are ultrasound diagnostics, CT, MRI, radiography, endoscopic examinations. For example, ultrasound can detect cervical cancer if it has metastasized beyond the peritoneum. In addition, ultrasound is used to assess the patency of the ureters and the condition of the kidneys (renal failure is the leading cause of death in cervical cancer).
The most informative research methods allow you to assess the stage and detect which organs the tumor has grown or metastasized into:
- Endoscopic research methods - cystoscopy (insertion of a video camera into the bladder) or proctoscopy (examination of the rectum using video endoscopic equipment)
- Laparoscopy – allows you to examine the pelvic cavity
- Chest X-ray – to detect metastases in the lungs
- Computed tomography or MRI - allows you to detect metastases of any location ranging from a few millimeters in size
- Intravenous (excretory) urography - X-ray examination of the kidneys with contrast to assess their function and urodynamics (the movement of urine through the urinary tract)
- Positron emission tomography - injection of radioactive substances that accumulate in tumor cells, followed by their visualization
An experienced doctor knows what cervical cancer looks like on an ultrasound, CT or MRI. Correct determination of the stage of the oncological process allows you to choose the right treatment tactics.
Send a request for treatment
Preparing for an ultrasound
Ultrasound examination of the kidneys is a procedure that requires minimal preparation. The main recommendations for patients are as follows:
- For three days before the kidney examination, you should follow a diet: food should be well digestible and light. Foods that cause bloating or increased gas formation (brown bread, sauerkraut, carbonated drinks, fruit juices, raw fruits, whole milk, etc.) must be excluded;
- the last meal should be no later than 8 hours before the kidney examination;
- The procedure requires a full bladder, so it is recommended to drink several glasses of still water an hour before the ultrasound;
- Before an ultrasound examination of the kidneys, you should not take diuretics;
- 4 hours before the procedure, you must refrain from smoking: changes in the vascular system caused by nicotine can blur the picture and interfere with tumor detection and accurate diagnosis;
- If there are constant problems with the intestines that are not corrected by diet, the patient is recommended to take medications that reduce gas formation before the examination.
Organization of treatment in Germany
In Germany, modern methods of treating cervical cancer are used. ]Booking Health[/anchor] can arrange treatment for you in this country. We have direct contracts with all major German clinics.
You can receive effective treatment for cervical cancer at the Helios Clinic Berlin-Buch. The Helios Clinic Berlin-Buch is a maximum care medical center, which is an academic clinic of the best medical complex in Europe, the Charité. The Department of Gynecology, under the direction of Prof. Dr. med. Michael Untha, offers women extensive examinations to detect precancerous conditions and/or assess the stage of cancer. Based on the examination results, specialists determine the optimal treatment tactics, including all types of surgical interventions and systemic therapy. Every year, the department treats about 5,000 women, with more than 3,000 of them undergoing surgical treatment. Due to high treatment success rates, qualified doctors and excellent technical equipment, the department is certified by the German Cancer Society as a specialized Center for Gynecological Oncology. The head physician of the department is a member of the Working Group on Gynecological Oncology and the Berlin Cancer Society.
You can contact us to:
- Choose the best clinic where you will get the best possible therapeutic results
- Save on medical services up to 70%
- Receive a full package of services (document preparation, logistics, interpretation and translation, etc.)
- Get insurance that will cover unexpected medical expenses up to 200 thousand euros for 4 years
Fill out an application on our website. Our specialist will select the optimal therapeutic programs for you and call you within a few hours to agree on all issues.