- home
- Technologies
- Laparoscopic tubal surgery
Laparoscopic operations on the fallopian tubes for chronic salpingitis, infertility, ectopic pregnancy, for sterilization.
The first operation performed endoscopically was sterilization. Coagulation of the fallopian tubes with monopolar current was first reported by Palmer R. in 1962, and then by Steptoe PC in 1967. In 1973, Rioux JE and Cloutier D. created a bipolar coagulator to perform coagulation of the fallopian tubes. In the 70-80s, mechanical methods of laparoscopic sterilization using clips and rings, as well as various methods of transcervical occlusion of the fallopian tubes, were proposed. In 1973, Shapiro HI, Adler DLN for the first time removed the fallopian tube using laparoscopic access. A huge contribution to the development of minimally invasive surgery was made by K. Semm, who in 1975 published the first practical guide to operative laparoscopy, which presented the operations of separation of adhesions, terminal salpingostomy, removal of appendages, ovarian resection, etc. In 1977, Bruhat MA, Manhes H et al. reported on conservative interventions for ectopic pregnancy performed endoscopically. In 1981–1982 DeCherney AH described laparoscopic salpingostomy, and since then endoscopic treatment of tubal pregnancy has been widely developed.
Video of the operation using this technique by Prof. Puchkova you can see here
Surgeries on the fallopian tubes can be radical and reconstructive plastic. In radical operations, the tube is completely or partially removed due to an ectopic pregnancy or a purulent-inflammatory process. According to V.I. Kulakova, L.V. Adamyan, they make up approximately 14%. Reconstructive interventions (about 86%) are aimed at restoring the patency of the fallopian tubes and are closely related to the study of the problem of infertility.
Indications and contraindications for laparoscopic tubal surgery
Indications for laparoscopic operations on the fallopian tubes are:
- occlusion of the lumen of the fallopian tubes;
- the presence of peritubar adhesions;
- tubal pregnancy;
- salpingitis, sacto(pio)salpinx;
- sterilization.
Laparoscopic operations on the fallopian tubes (tuboplasty) are contraindicated if:
- inflammatory process in the lower genital tract;
- active inflammatory process of the pelvic organs (in less than 4-6 months);
- fallopian tube length less than 4 cm;
- the presence of a huge sactosalpinx, after removal of which the remainder of the tube will be less than 4 cm;
- obstruction in several parts of the fallopian tube, including in the isthmic section.
When performing laparoscopic operations in gynecological practice, the following instruments and equipment are used:
- endovideo system, including an optical system with a video camera, a light guide and a medical monitor;
- laparoscope;
- gas insufflator;
- aspirator-irrigator;
- electrosurgical unit;
- Veress needle;
- 5 mm trocars – 2;
- 10 mm trocar – 1;
- soft and hard 5 mm clamps, 5 mm dissector, 5 mm endhook;
- monopolar scissors;
- bipolar forceps;
- needle holder;
- suture material: “Polysorb” or “Vicryl” 4-0, 6-0;
- uterine retractor "Clermontferan" (Germany) or hysterograph, which ensures a change in the position of the uterus during the operation and the introduction of contrast.
Surgical correction of tubo-peritoneal infertility is carried out in phase 1 of the menstrual cycle in order to ensure optimal conditions for tissue regeneration and the possibility of carrying out rehabilitation measures.
In this case, you must be guided by the following provisions:
- all operations should be performed using 2-3 manipulators;
- all manipulations and displacement of organs should be performed only with the help of atraumatic instruments;
- tissue dissection in all cases is carried out after preliminary coagulation;
- all types of plastic surgery on the fallopian tubes should be performed after tightly filling them with methylene blue;
- At the end of the intervention, the pelvic cavity should be washed with sterile saline and anti-adhesion gel should be injected.
The tubes are inspected before the contrast is introduced (methylene blue solution), and then the movement of the latter through the tube and its outflow from the fimbrial region are traced.
Before attempting any surgical manipulation related to the fallopian tubes, it is advisable (if technical capabilities are available) to perform a tuboscopy to assess the condition of the endosalpinx and identify the degree of disruption of its folding, which has a very great prognostic value. Attempts to restore the patency of the fallopian tube when its mucosa is in poor condition do not give a positive effect; the method of choice for treating these patients is in vitro fertilization.
Through the umbilical access, a Veress needle is used to apply carboxyperitoneum in a volume of 3-4 liters to an intra-abdominal pressure of 12-15 mmHg. Interventions are performed from three approaches, using two 5-mm trocars and one 10-mm trocar for optics (Fig. 1). The fourth, 5-mm trocar, can be inserted as needed (in the case of severe adhesions in the pelvis). A uterine manipulator or hysterograph is inserted into the uterus, fixed on bullet forceps, which ensure a change in the position of the uterus during the operation, which makes it easier to manipulate the abdominal cavity and perform chromosalpingoscopy.
Fig. 1. Points of insertion of trocars during operations on the fallopian tubes (1 - 10 mm trocar, 2,3,4 - 5 mm trocars), the 4th trocar is placed extremely rarely
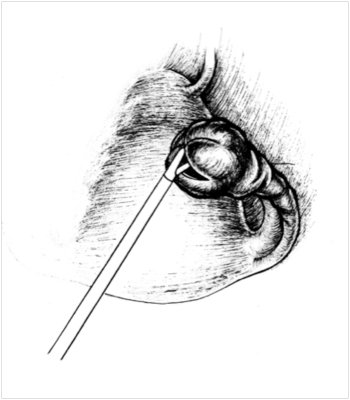
Rice. 2. Cross-shaped dissection of the ampullary section of the fallopian tube during salpingostomy (Puchkov et al, 2005)
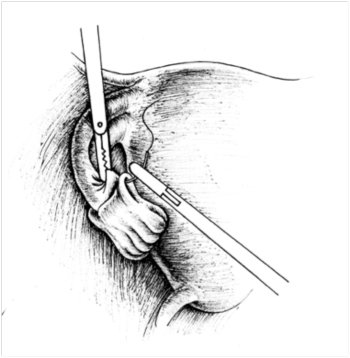
Rice. 3. Inversion of the petals and their fixation with sutures for salpingostomy (Puchkov et al, 2005)
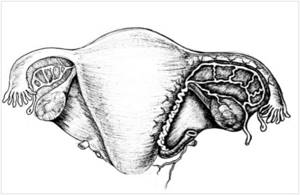
Figure 4. Location diagram of r.tubarius indicating areas of coagulation and intersection during salpingostomy (Puchkov et al, 2005)
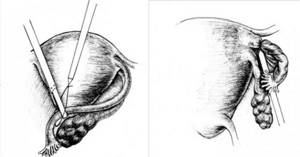
Figure 5. Performing salpingectomy using a loop ligature: a) applying a ligature to the fallopian tube; b) tightening the ligature (Puchkov et al., 2005 d) Fig.6. Force Triad LigaSure device with a set of tools
Preparing for surgery
The following types of diagnostics are required (results are valid for two weeks):
- coagulogram;
- general and biochemical blood tests;
- general urine analysis;
- blood tests for HIV, hepatitis, syphilis, group and Rh factor;
- vaginal and urethral smears for flora;
- Ultrasound of the pelvis;
- cytology of the cervical canal and cervix;
- fluorography;
- ECG.
In addition, you need to visit a therapist, anesthesiologist, and surgeon.
Shishkina Yulia Sergeevna
Obstetrician-gynecologist, gynecologist-endocrinologist, reproductive specialist, operating gynecologist
“Laparoscopy is widely in demand in gynecology. This technique allows you to diagnose and eliminate many diseases of the female reproductive system that are the causes of infertility. Laparoscopy is an extremely accurate, patient-friendly and effective method of treating fallopian tubes in gynecology.”
Laparoscopic surgery - salpingo-ovariolysis
The purpose of the operation is to restore normal topographic relationships by cutting the adhesions around the fallopian tube and ovary, isolating them from each other. Salpingo-ovariolysis is performed either as an independent intervention or as a preparatory step for surgery on the fallopian tubes. The fallopian tube (ovary) is picked up with atraumatic forceps and moved upward if possible. The adhesions are cut with endoscissors after their preliminary coagulation. Rough adhesions are excised and removed from the abdominal cavity. Special precautions are necessary when working near the intestines, ureters, and large vessels. The risk of their damage can be reduced by observing the following conditions: the operation is performed under general anesthesia with sufficient relaxation, the absence of defects in the insulating braid of the instruments, short-term switching on of the electrosurgical unit. After complete release of the fallopian tube from adhesions along its entire length, ovariolysis is performed. In this case, it is imperative to lift the ovary and inspect its surface facing the broad uterine ligament, since adhesions can often be localized there.
Causes of ectopic pregnancy
There are a number of reasons that can cause an ectopic pregnancy:
- inflammatory diseases of the uterus and appendages suffered previously;
- ovarian cysts and benign tumors that cause obstruction of the fallopian tube;
- uterine fibroids, localized at the junction of the uterus with the tubes;
- endometriosis in the fallopian tubes;
- adhesions surrounding the fallopian tubes;
- previous surgical interventions on the genital organs;
- previous abortions;
- the presence of intrauterine contraceptives.
Operation of salpingostomy (neostomy) and methods of laparoscopic fimbrioplasty
Fimbryolysis is performed for phimosis of the fimbrial part of the fallopian tube. While maintaining tight filling of the fallopian tube, endoscissors are used to gradually dissect along the radial scars and the center of the stellate scar, if any. After that, atraumatic forceps are inserted into the lumen of the tube in a closed state, the jaws are opened to a width of 2.5-3 cm and removed in this position. The procedure is performed 2-3 times.
Salpingostomy is performed when the tube is obstructed in the ampullary section. The ampullary section is fixed between two clamps against the background of tight filling with a methylene blue solution, which will allow you to correctly determine the location for the incisions. Endo-scissors are used to crosswise dissect the sealed ampullary section of the fallopian tube with two incisions 2-3 cm long along the scar changes so that they intersect at the pole of the hydrosalpinx (Fig. 2). Thus, 4 flaps (petals) are formed.
A soft clamp is inserted into the lumen of the fallopian tube and fixes its wall. Using a dissector, grasping the edge of the fimbrial section, the tube is turned out for 2-3 cm. To prevent it from returning to its previous position, the petals are fixed with 2-3 sutures with threads no thicker than 4-0 gauge, using the technique of intracorporeal knot tying (Fig. 3). If it is not possible to apply sutures, to maintain the tube in a passable state, you can use bipolar coagulation, which will “glue together” the serous cover of the peritoneum of the inverted section of the tube in the form of a duplicate. Hemostasis is achieved by point coagulation with a dissector. If possible, bleeding vessels of the mucous membrane are not coagulated to avoid damage.
There is a simpler salpingostomy technique - point endocoagulation (both mono- and bipolar coagulator) of the peritoneum of the fimbrial section dissected crosswise at a distance of 0.5-1.0 cm from the edge of the tube mouth along its perimeter. The endocoagulation areas should be separated from each other by a distance of 0.7-1.0 cm. As a result of endocoagulation, the outer layer of the pipe wall contracts and the edges of the stoma turn outward, which prevents them from gluing in the postoperative period. Salpingoneostomy involves the creation of a new artificial opening in the ampullary section of the fallopian tube. The operation is performed when it is impossible to open the tubal lumen in the fimbrial region. After filling the tube with methylene blue at the site of the intended dissection of the wall on the side opposite the mesosalpinx, linear coagulation is performed with a point coagulator for 2-3 cm along the ampullary section, followed by opening the lumen with an endo-hook. Inversion and fixation of the edges of the neostomy is carried out using one of the above methods.
Mechanical restoration of fallopian tube patency , assessed by laparoscopy, does not guarantee its normal functional activity. Tube function can be assessed by examining pregnancy rates. The final result depends on many factors: the duration of occlusion, the severity of the adhesive process in the pelvis, the degree of damage to the organ - the state of the mucous and muscular layers that ensure the transport of the egg to the uterus, the severity of the cilia and the smoothness of the endosalpinx folds, the presence of polyps of the mucous membrane, the degree of thickening of the tube wall, the presence of functionally complete fimbriae, the length of the tube, the size of the hydrosalpinx (more than 3 cm in diameter), as well as the surgical technique used. The simultaneous use of means to prevent postoperative adhesions (introduction of anti-adhesive gel, antibacterial and physiotherapeutic treatment) helps to improve the results of the intervention.
Is it possible to restore the pipe after removal?
It would seem that the possibilities of modern medicine are so wide that it should be possible to replace the fallopian tube with a new one. However, in reality this cannot be done. Why? The fact is that in order to perform its function, the organ needs to fully contract, and special villi must be located on the mucous membrane, which push the egg towards the uterus. This cannot be achieved with reconstructive surgery.
Recovery is possible if doctors removed only a specific segment of the fallopian tube. This operation is carried out according to certain indications (for example, if the tube is fused to the ovary in a small area).
Fallopian tube resection surgery - salpingectomy and salpingotomy
Salpingectomy is an operation to remove the fallopian tube from one or both sides, which is performed in the following cases:
- with a disturbed tubal pregnancy, accompanied by pronounced changes in the tubal wall;
- for chronic salpingitis that is not amenable to conservative treatment, especially in the presence of hydrosalpinx.
Removal of the fallopian tube, which has changed due to inflammatory processes and has no prospects for restoring its function, can be a preparatory step for subsequent in vitro fertilization.
A number of salpingectomy methods have been described in the literature.
Using an instrument inserted through the left lateral port, the fallopian tube is grasped and pulled up, creating exposure. Using an electrosurgical dissector in the mode of alternating monopolar coagulation and cutting, the fallopian tube is crossed at a distance of no more than 1 cm from the angle of the uterus and its mesentery in close proximity to the latter. Knowledge of the anatomical location of r.tubarius will help avoid damage to the vessels of the mesosalpinx and the occurrence of intraligamentary hematoma (Fig. 4).
Mobilization of the above-mentioned formations can also be performed by step-by-step coagulation with bipolar forceps followed by dissection with endoscissors. The third option for tubectomy is to apply a loop ligature with a 2-0 absorbable thread to the mesosalpinx and the uterine end of the tube, followed by cutting off the tube with endoscissors (Fig. 5 a, b). The proximal section of the tube is pre-coagulated as close to the uterus as possible in order to exclude the possibility of subsequent pregnancy developing in the stump of the removed tube. At the end of the operation, careful sanitation of the entire abdominal cavity is necessary, including the subdiaphragmatic space, lateral canals, and surgical field.
Recently, in operative gynecology, electrosurgical platforms of a completely new generation Force Triad “LigaSure” (Switzerland) have begun to be used for practical use. This device includes both monopolar and bipolar electrosurgical units, as well as an improved system of dosed ligation technology for vascularized tissue, which provides dosed energy supply depending on the properties of the coagulated tissue (tissue impedance). According to a number of foreign and Russian authors, dosed bipolar electrocoagulation makes it possible to stop bleeding and reliably close vessels with a diameter of up to 7 mm. When the device acts on the tissue, the liquid component is evaporated, collagen and elastin are dried and denatured until a dense homogeneous mass is formed that reliably closes the lumen of the blood vessels. Thus, the use of the LigaSure device for hemostasis during endosurgical mobilization of organs and closure of large vessels can serve as a universal way to stop bleeding. The use of this device when performing tubectomy reduces the operation time to 5 minutes and reduces the amount of blood loss to zero.
Performing salpingotomy with preservation of the fallopian tube during ectopic pregnancy is advisable:
- when the diameter of the fertilized egg is no more than 4 cm;
- in the presence of a developing pregnancy in the ampullary region;
- in the absence of tissue imbibition and arosion of the vessels of the pipe wall.
After dissecting the peritubar adhesions and fixing the tube with a soft clamp, the antimesenteric edge is opened longitudinally with a needle electrode or scissors above the proximal area of dilation, where the fertilized egg is usually located (the distal part of the dilation of the fallopian tube is filled with blood clots). The fertilized egg is easily removed by pressing from the side of the serosa or peeled off using hydraulic preparation. With the correct choice of incision site and precision surgical technique, it is possible to completely remove the fertilized egg and detach the chorion without bleeding. The lumen of the fallopian tube is thoroughly washed and hemostasis is controlled. If there are bleeding areas in the placental area, excessive coagulation should be avoided and carried out using microsurgical forceps. If it is not possible to identify individual vessels, then, according to V.I. Kulakov, L.V. Adamyan, a continuous suture or coagulation can be applied to the mesosalpinx in this area. The hole in the fallopian tube is usually not sutured. Both edges of the wound are usually well matched. Studies conducted by Tulandi T., Guralnick M., Nelson L. have proven that suturing during these operations worsens the effectiveness of surgical treatment, compared with sutureless surgery, due to deformation of the fallopian tube. In this regard, they believe that suturing the tubotomy incision is inappropriate. Complete healing of the wound with restoration of integrity and patency occurs in 3-6 months. At the final stage of the operation, chromosalpingoscopy is performed to determine the patency of the fallopian tube.
A specific postoperative complication of salpingotomy performed for tubal pregnancy is persistent ectopic pregnancy - the growth of trophoblast tissue after incomplete removal of the fertilized egg. This dictates the need to determine the beta-hCG titer over time after surgery. If it decreases, then you can stick to wait-and-see tactics. If the level of beta-hCG remains the same or increases, surgical intervention is indicated to remove the remaining part of the ectopia or the prescription of a short course or a single dose of methotrexate.
Consequences of the operation
Immediately after a tubectomy, many women report to the doctor that they have discomfort and a feeling of heaviness in the abdomen. Such sensations are due to the fact that carbon dioxide partially remained in the abdominal cavity, which was pumped there during surgery. The discomfort goes away after a few days.
Some patients, after some time, begin to notice symptoms indicating hormonal disorders:
- weight gain;
- engorgement of the mammary glands;
- diffuse enlargement of the thyroid gland, not accompanied by disruption of its activity;
- hypertrichosis (excessive hair growth on various parts of the body);
- emotional instability, headaches, increased sweating.
Menstrual irregularities develop in approximately 30% of women after unilateral and 40% after bilateral tubectomy. There may be delays in menstruation, as well as dysfunctional uterine bleeding (that is, those that are not associated with menstruation).
If one tube is removed, the chances of successful conception are reduced, but a natural pregnancy is still possible. After a bilateral tubectomy, the doctor diagnoses infertility. However, this is not a death sentence at all, since the IVF method makes it possible to achieve the birth of a child in the vast majority of cases (even if there are other pathologies of the reproductive system).
Experts note that after surgery, sclerotic changes often occur in the ovaries and cysts form, and these processes are most pronounced on the side of the removed tube. In the case of bilateral tubectomy, such changes are observed equally in both ovaries and develop faster.
Sterilization operation
Sterilization of the fallopian tubes, according to L.V. Adamyan (2000), PJ Taylor (1995), is one of the most common gynecological procedures. Indications for surgical sterilization:
- the couple's desire for complete fertility prevention;
- intolerance to other methods of contraception;
- medical indications - diseases of the cardiovascular, endocrine, musculoskeletal systems, mental disorders, hereditary diseases in which pregnancy and childbirth are absolutely contraindicated.
Before the operation, it is necessary to obtain the patient’s personal signature agreeing to sterilization. It is necessary to explain to her that restoration of patency of the fallopian tubes after any method of sterilization is not guaranteed.
With a normal menstrual cycle, surgery should be performed in the early proliferative phase. For women using an IUD, it is advisable to perform it 1 cycle after removal of the intrauterine contraceptive device and prophylactic antibacterial treatment. For patients taking oral contraceptives, sterilization can be performed at any time. The combination of artificial termination of pregnancy and sterilization, in our opinion, is inappropriate.
Currently, there are several options for tubal occlusion. Surgical intervention is performed through 2 approaches: a 5-mm trocar - paraumbilical, 5-mm - in the left (right) iliac region or in the midline above the pubic symphysis. If there is an adhesive process or other complicating issues, a third trocar is introduced.
After fixing the fallopian tube with a clamp, it is monopolarly coagulated over a length of 2 cm, 2-3 cm from the angle of the uterus, followed by dissection with endoscissors to the mesosalpinx, which significantly reduces the risk of recanalization. Coagulation can also be performed using a bipolar electrode in 2 or 3 places.
It is possible to excise a section of the fallopian tube 1-2 cm long after preliminary bi- or monopolar coagulation at a distance of 2 cm from the angle of the uterus.
Fimbriectomy involves coagulation and division of the distal portion of the mesosalpins near the infundibulopelvic ligament and the infundibulum of the fallopian tube.
According to the results of studies by Gomel V., Winston L., J. Hulka J., applying Hulka-Clemens clips to the isthmic part of the tube strictly in a perpendicular direction is a method that ensures the highest efficiency of the refertilization operation. In this regard, when deciding whether to perform sterilization, the patient's future need for a procedure to restore patency of the fallopian tubes should be taken into account.
Yun's ring method involves applying silicone rings using a special tool. The fallopian tube is captured by jaws at the junction of the isthmus and the ampulla, pulled into the lumen of the instrument, the ring is put on the loop of the tube and compresses it. Due to ischemic damage to the tube over a long distance, the likelihood of reversibility of this intervention is very low.
Benefits of laparoscopy
You should be aware of the advantages of laparoscopic intervention over abdominal surgery. Firstly, this is a short rehabilitation period. Recovery will take only 3 to 5 days (the woman will be in the hospital during this time). If you cut the abdominal wall with a scalpel, you will have to stay in the hospital for at least 10, maximum 15 or more days.
As for the type of stitches that remain after the operation, after laparoscopy there will be three small scars, each of which is a maximum of one and a half centimeters. They won't be noticeable.
Endoscopic operations give the surgeon the opportunity to fully control the process through the control of a video camera. It displays the image on the screen at 10x magnification. This operation is gentle because, due to video control, the doctor has no chance of damaging healthy tissue.









