Detailed description of the study
Upper respiratory tract infections (URTIs) are common among people of all ages. Infection with them is possible at any time, but the peak incidence usually occurs in the autumn-winter period. URTIs include rhinitis (inflammation of the nasal mucosa), pharyngitis (inflammation of the pharynx), tonsillitis (inflammation of the pharyngeal and palatine tonsils) and laryngitis (inflammation of the larynx).
The clinical picture of these diseases may vary depending on which organ is affected. Common manifestations of URTI include:
- Runny nose, nasal congestion
- Sore throat
- Sneezing
- Cough
- Headache
- Increased body temperature
- General malaise
- Muscle pain
Separately, one can distinguish inflammation of the epiglottis - epiglottitis, in which the following symptoms suddenly appear:
- Difficulty or pain when swallowing, sensation of a lump in the throat
- Asphyxia (suffocation caused by compression of the airways, closing their lumen)
- Salivation
- Hoarseness of voice
- Dry cough
- Increased body temperature
This condition is caused by infection with the bacterium Haemophilus influenzae type B (hemophilus influenzae) and is more common in children aged 1-5 years.
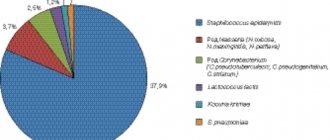
The causes of URI development can be both viruses and bacteria. The upper respiratory tract is inhabited by many bacteria, which normally contribute to the body's resistance to infections. Among them, opportunistic ones are distinguished, such as some types of streptococci, staphylococci, corynebacteria, etc.
Group A β-hemolytic streptococci play an important role in the development of tonsillitis and pharyngitis. They are the cause of the development of bacterial tonsillitis, in which, unlike viral tonsillitis, antibiotic therapy is necessary. Inflammation of the epiglottis caused by Haemophilus influenzae also requires antibiotics. Some people serve as asymptomatic carriers of these bacteria and a source of their spread.
Culture of discharge from the throat or nose is the standard for diagnosing URI, confirming or refuting the role of bacteria in the development of these diseases. Timely identification of the causative agent of URI allows you to prescribe the necessary treatment and prevent complications of the disease.
Throat swab: features of the procedure
Before taking a swab from the mucous membrane of the throat, the patient should be informed about special preparation. So, the procedure should be carried out on an empty stomach or no earlier than 3 hours after drinking or eating. Before performing it, you should also not rinse your mouth, brush your teeth, use oral sprays, or use antibiotics.
The analysis procedure is as follows:
- the patient opens his mouth wide;
- The ENT
examines the oral cavity, determines the place where the discharge is collected; - the doctor presses the tongue with a spatula and runs it along the back wall of the throat and the mucous membrane of the tonsils with a sterile swab;
- carefully removes the swab and lowers it into the test tube;
- records the time of taking the analysis.
Useful information on the topic:
- Pediatric ENT
- Diagnosis of ENT diseases
- Consultation with an ENT doctor
- Treatment of ENT diseases
- Examination by an ENT doctor
- Prevention of ENT diseases
- ENT doctor appointment
- EAR, throat, nose
- Otolaryngology
- Paid ENT
Scope of application of bacteriological culture
Bacteriological culture is used to make an accurate diagnosis in the following areas:
- ENT diseases;
- dermatology;
- urology;
- venereology;
- gynecology and other areas of medicine.
Bacteriological culture is equally effective against both non-acute and indolent, latent infections. Bacteriological culture is very often used to detect infections in the nasal cavity to diagnose rhinitis and sinusitis. It is also widely used for gynecological purposes.
However, many of these medical fields needlessly abuse this procedure. Often, the use of bacterial analysis depends on material interests and the reluctance or ignorance of doctors regarding methods for diagnosing syndromes.
Basically, this analysis is indicated for use in the presence of female pelvic inflammatory disease and recurrent vulvovaginitis, male prostatitis and chronic torpid urethritis, but it is also widely used for diseases of the nose and throat. Doctors insist on confirming the presence of various nasal infections in the following categories of citizens: girls, elderly women, conscripts and pregnant women.
Microscopic examination
The material to be examined is applied to a glass slide, fixed in a burner flame, Gram stained, and examined under an oil immersion microscope. Gram-negative or gram-positive rods, cocci or coccobacilli are detected in the smear, and their morphological and tinctorial properties are studied.
Microscopic signs of bacteria are an important diagnostic guide. If the smear contains gram-positive cocci, located in clusters resembling bunches of grapes, it is assumed that the causative agent of the pathology is staphylococcus. If the cocci stain positive for Gram and are located in the smear in chains or pairs, it may be streptococci; gram-negative cocci - Neisseria; gram-negative rods with rounded ends and a light capsule - Klebsiella, small gram-negative rods - Escherichia, Pseudomonas aeruginosa. Further microbiological examination is continued taking into account microscopic signs.
Indications
The doctor prescribes culture of mucus from the throat and nose for microflora and sensitivity to antibiotics to confirm the diagnosis of various infectious diseases in children and adults. A smear is taken:
- with sore throat;
- if you suspect whooping cough;
- to exclude diphtheria of the pharynx;
- for fungal diseases.
A swab is also taken for healthy people during medical examinations. The following categories of people should take a smear:
- pregnant women;
- persons who have been in contact with a patient with diphtheria or tonsillitis;
- persons entering work in the food industry, educational and preschool institutions, and medical institutions.
Each person has normal and conditionally pathogenic microflora in the nasal cavity and pharynx, its quantity does not exceed a certain indicator. Under normal conditions, flora does not cause any diseases in humans.
Culture for group A hemolytic streptococcus
Microbiological examination to detect infection with group A hemolytic streptococcus.
Synonyms Russian
Culture for group A beta-hemolytic streptococcus, culture for pyogenic streptococcus, culture for GABHS.
English synonyms
Group A streptococci culture, GAS culture, S. pyogenes culture, Beta hemolytic streptococcus culture.
Research method
Microbiological method.
What biomaterial can be used for research?
Oropharyngeal swab, nasopharyngeal swab, nasal swab.
How to properly prepare for research?
- 3-4 hours before taking swabs from the oropharynx (throat), do not eat, drink, brush your teeth, rinse your mouth/throat, chew gum, or smoke. 3-4 hours before taking nasal swabs, do not instill drops/sprays or rinse your nose. It is best to take smears in the morning, immediately after a night's sleep.
General information about the study
Streptococci are the most common causative agents of bacterial infections in humans. There are various serological groups of streptococci: A, B, C, D, F, G. The most pathogenic for humans are group A streptococci, or pyogenic streptococci.
Bacteria of this group have hemolytic properties (can destroy red blood cells), therefore they are also called hemolytic streptococci. They are the causative agents of various purulent and immunoinflammatory diseases, such as tonsillitis, pharyngitis, tonsillitis, scarlet fever, otitis, acute rheumatic fever and rheumatic heart disease, acute glomerulonephritis, myocarditis, endocarditis, erysipelas, streptoderma, osteomyelitis, otitis. Group A hemolytic streptococcus culture is performed to detect streptococcal infection and is the gold standard for diagnosing streptococcal pharyngitis.
What is the research used for?
- To confirm the diagnosis of streptococcal infection.
- For differential diagnosis (along with other studies) of diseases that occur with similar symptoms, such as pharyngitis and tonsillitis of various origins, localized form of pharynx diphtheria, peritonsillar abscess, infectious mononucleosis, leukemia, agranulocytosis, acute respiratory infections, oropharyngeal candidiasis, exacerbation of chronic tonsillitis.
- To evaluate the effectiveness of antibacterial therapy for streptococcal infections.
When is the study scheduled?
- When a patient has a sore throat or pharyngitis.
- If a streptococcal infection or bacterial carriage is suspected.
- For nosocomial infections.
- When carrying out antibacterial therapy for streptococcal infection.
- In some cases, for prophylactic purposes before hospitalization in a hospital.
What do the results mean?
Reference values: no growth.
Reasons for a positive result
- Acute streptococcal infection.
- Asymptomatic bacterial carriage.
Reasons for a negative result
- Absence of streptococcal infection (provided that no antibiotic treatment was carried out).
What can influence the result?
Antibacterial therapy.
Also recommended
- Streptococcus pyogenes, DNA [real-time PCR]
- Complete blood count (without leukocyte formula and ESR)
- General urine analysis with microscopy
- Creatine kinase MB
- Troponin I
- Culture for diphtheria (Corynebacterium diphtheriae)
Who orders the study?
Infectious disease specialist, therapist, general practitioner, pediatrician, ENT, rheumatologist.
Literature
- Bisno AL, Stevens DL Streptococcus pyogenes. In: Principles and practice of infectious disease / GL Mandell, Bennett JE, Dolin R (Eds) ; 6th ed. – Churchill Livingstone, Philadelphia, PA 2005. – 2701 p.
- Guide to infectious diseases / ed. Yu.V. Lobzina, S.S. Kozlova, A.N. Uskova. – St. Petersburg: Phoenix, 2001. – 932 p.
What reveals
A nasal swab allows you to determine the presence or absence of the following types of microorganisms:
- Corynobacter diphtheria;
- Staphylococcus aureus;
- streptococcus;
- hemophilus influenzae;
- mushrooms of the genus Candida;
- pneumococcus and much more.
It is important to note that for many organisms, counts below 104 CFU/ml do not warrant concern. High rates require determination of resistance to antibacterial drugs and phages necessary for timely treatment.
Procedure
Before the procedure, the patient will have to perform simple manipulations. A throat swab must be taken on an empty stomach. At least 2 hours before this, you should not gargle, drink or eat. It is also worth considering that taking antibacterial drugs can significantly affect test results.
A smear is taken as follows:
- The patient sits down on a chair.
- It is recommended to open your mouth wide so that the doctor or technician can access the desired area.
- The material is collected using a sterile cotton swab pre-wound on a handle.
- After taking the analysis, the swab is placed in a transport medium, which will be used to transfer the material to the laboratory for subsequent research. It is important to comply with short deadlines and all necessary conditions during transfer, as this affects the results of the analysis.
- When the smear is delivered to the laboratory, it is carefully examined under a microscope to determine the cellular composition of the mucous membrane. Sowing on nutrient media is also performed. This action is aimed at accurately determining the pathogenic microorganism and its sensitivity to certain groups of antibiotics. Due to this, it becomes possible to rationally influence the body without resorting to the use of unnecessary drugs.
Throat swab in Lipetsk
Treatment and diagnostic center No. 1 has everything necessary to conduct a comprehensive examination of the patient. Taking a smear from the throat is often one of the most informative research methods, so otolaryngologists prescribe it if there are contraindications to its conduct. The high accuracy of the results allows the specialist to prescribe the most effective treatment, eliminating the need to use unnecessary medications.
Contact our center if you need qualified assistance.
Sign up for ENT: +7, +7, +7, you can also sign up online