The chest contains many vital organs: the heart, lungs, esophagus... That is why diagnostic studies of the mediastinum must be as accurate as possible - after all, the timely detection of possible diseases depends on them.
One of the most informative and at the same time painless methods of studying the chest organs is magnetic resonance imaging (MRI). Most often it is prescribed for examining soft tissues: lungs, pleural cavities, etc.
Bronchi and lungs. Diagnosis of diseases of the lungs and bronchi
In most cases, to make a correct diagnosis, it is enough to follow three steps:
- See the structure of the lungs using an x-ray or x-ray computed tomography. Computed tomography is more informative than conventional radiography of the lungs. With conventional radiography, small details may not be visible: they can be “hidden” behind the overlay of projection shadows. A CT scan of the lungs can show tuberculosis, inflammation or traces of previous inflammation, inflammation of the pleura, fluid in the pleural cavity or heart sac. It is possible to determine the presence of tumors, rib fractures and vertebral fractures. It is important that CT scans can assess the condition of the thymus gland (thymus) and lymph nodes of the chest. Those. Almost the entire anatomy of the chest can be assessed in detail.
- Determine the function of the lungs and bronchi . It is easier to see the function of the lungs and bronchi using external respiration function or spirometry. This study is needed to assess the speed and volume of exhaled air flow, incl. for the diagnosis of bronchial asthma. Using the external respiration function, you can easily determine whether there are any obstacles to the flow of air or not, as well as see the vital capacity of the lungs. Pulmonary function can also be assessed based on the results of pulse oximetry, i.e. according to the degree of oxygen saturation of the blood. In case of breathing disorders during sleep, so-called sleep apnea due to snoring, overnight respiratory monitoring is carried out.
- Laboratory research . If there is sputum or any discharge from the respiratory tract, a laboratory test is performed to determine the presence of viruses, bacteria, fungi, as well as specific markers of diseases in the biomaterial. It is also advisable to take a blood test to check for increased white blood cells and accelerated ESR (signs of inflammation) and for the content of hemoglobin and red blood cells. If ventilation of the lungs is impaired, with oxygen deficiency, the level of hemoglobin and red blood cells increases to compensate for the oxygen starvation of the tissues. When blood hemoglobin decreases, on the contrary, the load on the lungs increases, which are forced to compensate for the lack of oxygen in the tissues (shortness of breath due to anemia - anemia). In addition, a high level of IgE can be seen in the blood - a marker of the allergic process, which increases with bronchial asthma. Sputum can also be examined for the presence of atypical (tumor) cells and markers of bronchial asthma.
Typically, these three steps provide complete information about the state of the respiratory system. To interpret the research results, we will offer you a consultation with a doctor of the appropriate specialty. As a rule, this is a general practitioner, or a pulmologist, an allergist, an immunologist.
| You can determine how the lungs and bronchi work using a study of respiratory function (pulmonary function) (spirometry) | |
Laboratory research . Inflammation of the bronchi is usually caused by viruses and bacteria, less often by pathogenic fungi. It is clear that the treatment in these different cases will also be different. Treatment without an accurate determination of the cause that caused the inflammation may work poorly; the inflammatory process in the bronchi and lungs can only weaken and, over time, become chronic. Here you can perform PCR diagnostics, microbiological and cytological examination (microscopy) of sputum and any other respiratory tract secretions. Examination of secretions from the lumen of the bronchi and pleural fluid for the presence of infections is also possible, but to obtain such biomaterial it is necessary to perform bronchoscopy and pleural puncture.
Assessment of external respiratory function (spirometry) . Spirometry is the “gold standard” in the diagnosis of chronic lung diseases such as bronchial asthma, bronchitis and other pathological conditions when breathing is impaired (difficulty in inhaling or exhaling, “weak” lungs, etc.). A spirometer measures the speed and volume of air inhaled and exhaled. If bronchial asthma, bronchospasm, or bronchial obstruction is suspected, a test with a bronchodilator drug is performed.
X-ray of the lungs . X-ray of the lungs is a routine examination of lung tissue and is included in examination standards for the diagnosis of many diseases. Using X-rays, we can examine the lung in two projections, which makes it possible to identify pathological changes in the lung tissue. Lung X-ray helps to differentiate between lung diseases, for example, between tuberculosis, simple bronchitis and bronchiectasis, and is the diagnostic method of first choice when diagnosing pneumonia.
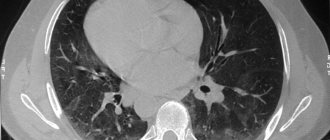
Computed tomography of the lungs . A computed tomogram (CT) of the lungs produces high-quality images of cross-sections of lung tissue. Using a CT scan of the lungs, you can identify foci of inflammation in the lung tissue, assess their size and interaction with nearby organs. Lung CT with contrast is mainly used in the diagnosis of tumors.
Magnetic resonance imaging (MRI) of the lungs If the doctor has questions when making a diagnosis, MRI of the lungs will help differentiate similar diseases, for example, distinguish a lung cyst from lung cancer. Magnetic resonance imaging (MRI) allows you to evaluate changes in blood vessels without the use of contrast agents.
Bronchoscopy . Bronchoscopy is an examination of the respiratory tract using an optical device - a bronchoscope. Bronchoscopy is highly informative in the diagnosis of bronchitis, bronchiectasis and in searching for the causes of cough of unknown etiology.
Ultrasound of the lungs. Using an ultrasound examination of the lungs, the doctor can identify the accumulation of fluid in the pleural cavity, which can form with pneumonia, tuberculosis and other lung diseases, assess the condition of the thoracic lymph nodes and find pulmonary tumors. Most often, due to its simplicity, lung ultrasound is used to diagnose pneumonia in children.
CT scan of the chest
Home – Chest – CT scan of the chest
Computed tomography of the chest, along with traditional radiography, is the leading method in the diagnosis of diseases of the lungs, mediastinum and chest wall
In what cases is a chest CT scan performed?
Indications for performing a breast CT scan:
- Differential diagnosis of pathological changes in the lungs and mediastinum, the nature of which cannot be determined on radiographs.
- Clarification of X-ray examination data of patients with an established diagnosis: a) prevalence and localization of pathological changes; b) identification of destruction cavities, enlarged lymph nodes and other changes not visible on radiographs.
- Detection of changes in the lungs and mediastinum in the absence of changes on radiographs and the presence of clinical signs of the disease: hemoptysis, rapidly progressing shortness of breath, chronic cough with large amounts of sputum, atypical cells or Mycobacterium tuberculosis in the sputum.
- Replacement of invasive diagnostic methods (bronchography, pneumomediastinography, diagnostic pneumothorax or pneumoperitoneum)
- Dynamic observation, assessment of the effectiveness of conservative and surgical treatment, identification of complications.
- Pathology of the sternum, ribs (tumors, osteomyelitis, perichondritis, etc.) and soft tissues of the chest wall.
- Diseases of the pleura (mesothelioma, prolonged pleurisy of unknown etiology, etc.).
Chest CT allows you to identify and differentiate various diseases of the lungs, mediastinum and chest wall, such as:
- Space-occupying formations (including primary tumors and metastases) of the lungs, mediastinum and chest wall. Given that CT can detect even very small lesions in the lungs, chest CT is especially effective for diagnosing lung cancer at an early, most treatable stage.
- Inflammatory changes in the lungs, mediastinum and chest wall, including those of a specific nature (pneumonia, tuberculosis, mediastinitis, osteomyelitis, etc.).
- Infectious destructive processes in the lungs (abscess, abscess pneumonia, septic embolism).
- Diffuse interstitial lung diseases (sarcoidosis, alveolitis, vasculitis, etc.)
- Parasitic diseases (echinococcus, alveococcus).
- Emphysema and obstructive pulmonary disease (COPD);
- Bronchial diseases (tumors, non-tumor stenoses, bronchiectasis; foreign bodies, cysts, atelectasis).
- Inflammatory or other diseases of the pleura (pleural effusion, pleural calcification, neoplasms, pneumothorax).
- Chest trauma (bruises of the lungs, hematomas of the lungs and mediastinum, hemothorax, including coagulated hemothorax, fractures of bone structures, etc.).
- Congenital anomalies.
When identifying space-occupying formations in the lungs and mediastinum, to clarify their prevalence and interaction with neighboring organs and structures, including vessels, it may be necessary to perform a CT scan with intravenous contrast, including CT angiography.
| STUDY | PLAN, rub. | URGENT, rub. |
Diaphragm study
The diaphragm is the muscle that separates the chest and abdominal cavities. Basically, a person needs a diaphragm for breathing. It can be compared to a piston in a car or bicycle pump - together with the pectoral muscles, it sucks air into the lungs, going down and expelling air, going up. In addition, the diaphragm is involved in the movement of food through the esophagus and in blood circulation (when the diaphragm lowers, pressure in the abdominal cavity increases and blood is “squeezed” out of the liver into the inferior vena cava, from where it enters the heart).
It so happens that there are practically no characteristic clinical signs of diseases and damage to the diaphragm. Sometimes patients may complain of pain in the middle of the chest or lower half of the chest, which radiates to the supraclavicular region, back or abdomen. Usually, the existence of an inflammatory process in the diaphragm is judged by the condition of nearby organs (stomach, liver, heart). The main instrumental method for studying the diaphragm is x-ray. The condition of the diaphragm is quite simple to examine by palpation and visually: by soreness in characteristic points, mobility of the ribs during breathing. The points of attachment of the diaphragm to the lumbar vertebrae are accessible to palpation, and often they are the source of difficult-to-diagnose chronic abdominal pain. In our clinic, diagnosis of diaphragm diseases takes place in several stages:
- Determination of the state of the diaphragm (its shape, surface, level of location, the presence of pathological shadows in the area of its location, determine the nature of the movement of the diaphragm);
- Determination of the position of the diaphragm relative to the thoracic and abdominal organs;
- Determination of the position and condition of nearby organs.
Determining the state of the diaphragm . The study of the diaphragm begins with a survey X-ray of the chest organs in several projections (direct, lateral and oblique). In case of diseases of the diaphragm or adjacent organs, a high or low position of the dome of the diaphragm, deformations and pathological darkening (tumors, cysts, abscesses) may be determined. In some diseases, the movements of the diaphragm may be impaired - from slight restriction to complete immobility. For a more detailed assessment of diaphragm movement disorders, your doctor may recommend that you perform x-ray kymography (video x-ray). The patient is not exposed to long-term irradiation, and interpretation of the video radiograph makes it possible to identify dynamic changes in the diaphragm, characteristic, for example, of a diaphragmatic hernia.

When examining the diaphragm, we may suggest that you perform an ultrasound of the abdominal organs to rule out associated inflammatory diseases.
Typical findings on X-ray examination:
- Hernias - diaphragmatic hernias can form due to a prolonged increase in intra-abdominal pressure (severe cough with bronchitis, obesity). The most common hiatal hernia is a hiatal hernia, which occurs when part of the stomach enters the chest cavity. This pathological condition may be accompanied by heartburn, pain in the epigastrium and along the esophagus. Sometimes the pain can be of a shingling nature, resembling pancreatitis. It is important to know that the part of the stomach that extends into the chest cavity, in some cases, can cause disturbances in the functioning of the heart (rapid heartbeat, extrasystoles) and patients can be treated unsuccessfully by a cardiologist for a long time. If necessary, we will offer you a consultation with a doctor in the required specialty.
- Subphrenic abscess - most often an abscess occurs due to inflammatory diseases of the abdominal organs, such as acute appendicitis, gastric and duodenal ulcers, liver and biliary tract diseases, pancreatitis, etc. Patients may complain of sweating, chills, high fever, a feeling of heaviness, and pain under the ribs. The pain may intensify when breathing, coughing, and radiate to the shoulder and shoulder blade. Hiccups, shortness of breath, and a painful dry cough appear. Sometimes the patient’s forced semi-sitting position is noticeable, in which it does not hurt so much.
- Paralysis or paresis of the diaphragm due to problems with the nerves supplying the diaphragm.
- Foreign bodies in the diaphragm - With blind gunshot wounds of the chest and abdomen, numerous fragments that have entered the thickness of the diaphragm may remain unrecognized. Clinically, such foreign bodies most often do not manifest themselves at all, but they may cause discomfort or vague pain in the chest, which intensifies with movement. When an infection occurs, the fragments can fester and form an abscess.
Determination of the position of the diaphragm and assessment of the condition of nearby organs. Due to the fact that most diseases of the diaphragm can be hidden or disguised as other diseases, if necessary, we can offer you an ultrasound and/or x-ray examination of the abdominal cavity in order to assess the condition of the internal organs adjacent to the diaphragm.
Modern diagnostic methods in pulmonology and ENT clinics
One of the urgent tasks of modern pulmonology is the creation of uniform standards for the diagnosis and treatment of various lung diseases. The diagnosis must be based on medical history, clinical, laboratory and other types of studies.
In the program of examining patients with various pathologies of the lungs and ENT organs, an important place is occupied by the integrated use of radiation diagnostic methods. Currently, X-ray images are obtained using direct analog, indirect analog and digital technologies.
The X-ray method remains one of the main research methods and includes general and special types of research. General types of research, in which there is no digital processing, involve the use of traditional standard radiography, fluoroscopy and linear longitudinal tomography. Radiography is a direct analogue technology and has the highest spatial resolution. This study is accessible, helps to identify a wide range of pathological changes, and provides information, in most cases, sufficient to make a diagnosis and determine treatment tactics. During dynamic monitoring of the patient, radiography makes it possible to make an accurate assessment of the course of the disease, allows you to track the formation of residual changes, and in the presence of complications, determine their nature.
The examination of the patient should begin with taking pictures in two mutually perpendicular projections, preferably on film measuring 35 x 43 cm on a Siregraph D-2M apparatus with an X-ray image intensifier (IIA) for 3 workstations, made by General Electric. Polyprojection radiography allows one to judge the localization and extent of the inflammatory process in the lungs, the condition of the lungs in general, the roots of the lungs, pleura, mediastinum and diaphragm. An image only in direct projection is allowed for patients in very serious condition.
Survey photographs of the chest are performed with the following technical data: from the focus of the X-ray tube to the film - 1.5 m (telephoto) using screening raster 12; voltage on the X-ray tube is 70–95 kV, anode current is 100–250 mA, exposure time is 0.1–0.3 s. However, chest images should be taken using the hard radiation technique (anode voltage - 120 kV, shutter speed - 0.02 s). On such images, the normal pulmonary pattern is traced to the periphery; pathological formations behind the shadow of the heart, diaphragm and small subpleural formations, which are not visible on ordinary images, are revealed. This makes it possible to interpret the interstitial structure. The effective dose load is no more than 1.0 mSv.
Currently, digital radiography is becoming increasingly widespread. Modern digital radiography systems include digital radiography from an electron-optical converter screen, digital fluorescence radiography, and digital selenium radiography. The fluorescent plate has a significantly greater exposure latitude than conventional film-screen combinations, thereby expanding the interval between under- and overexposure, which is important for obtaining a good quality image.
Digital radiography (Agfa Diagnostic, Villa Systemi, Amico, Medical Technologies, Electron) can detect areas of infiltration in the lung behind the shadow of the heart, in the paravertebral region. The dose load for this type of study is 0.03–0.6 mSv. An important feature of low-dose digital radiography is the ability to create electronic memory archives and transmit images over a distance. The creation of electronic image processing and transmission systems (PACS) is a new step towards the formation of x-ray departments of the future.
Fluoroscopy is a functional research method that allows you to examine the heart and respiratory organs during their movement and judge their function. To reduce radiation exposure to the patient, it is necessary to use X-ray diagnostic devices equipped with digital X-ray units. These include the FCMB fluorographic apparatus “Renex-Fluoro”, “Proscan-2000” and “Proscan-7000”, OKO FC. The method is used according to indications to identify symptoms of the presence of pleural fluid and its outcomes. An important method for the differential diagnosis of various lung diseases is linear tomography (a layer-by-layer type of study). Layer-by-layer examination eliminates the summation effect inherent in radiography. Tomography makes it possible to determine the nature, structure and extent of the pathological process localized in the lung parenchyma and pleura, to study the condition of the tracheobronchial “tree”, roots of the lungs, and mediastinum.
Linear tomography of the lungs (Philips, Siemens, Toshiba), depending on the task, is carried out: in direct, lateral and oblique projections; with longitudinal, oblique and transverse views of shadow smearing; with the patient in a vertical or horizontal position. The thickness of the separated layer during tomography depends on the angle of rotation of the X-ray tube. The larger it is, the smaller the thickness of the selected slice. With a transverse type of smearing, the released layer is thinner than with a longitudinal type. In this case, the contours and structure of the tomographed formation are better displayed. Isolation of a thick layer at an angle of rotation of the X-ray tube up to 12 is called zonography. The main attention in tomography is paid to the correct choice of section depth, which determines the diagnostic value of the resulting tomograms. To clarify the nature of the infiltrate in the lung parenchyma, tomography should be performed in two mutually perpendicular projections.
The larynx and trachea should be tomographed in two mutually perpendicular projections, the main and upper lobe bronchi - in direct and oblique projections. The optimal projection for the lower lobe bronchi of the lungs is lateral, for the middle lobe and lingular bronchi - oblique. The bronchi of the apical, posterior and anterior segments of both lungs are tomographed in frontal and lateral projections. The optimal projection for obtaining the lumens of the segmental bronchi of the middle lobe and lingular segments is an oblique projection with a patient rotation angle of 50–55° relative to the length of the body axis. To obtain the lumens of the apical segmental bronchi of the lower lobes, lateral tomography is used. Tomography of the basal segments is carried out in frontal and lateral projections. In these projections, the lumens of the basal bronchi of the lower lobe are displayed. Zonography is a thicker distinguishable layer. It is best used to clarify the nature of disseminated processes in the lungs, detailing the X-ray picture of fibrous and sclerotic changes, pulmonary pattern and roots of the lungs.
Among modern special methods of obtaining images in the diagnosis of diseases of the lungs and ENT organs, the method of choice is computed tomography (CT). Digital computed tomography, based on the high sensitivity of the method and the ability to quantify, has established itself as one of the most effective methods of medical imaging. Some of the most modern and reliable computed tomographs are spiral, X-ray computed tomographs “Aura” (Philips), “Aquilion” (Toshiba), “Pronto” (Hitachi Medical). A transverse image of the thoracic cavity allows one to study the topographic-anatomical relationship between normal and pathological changes in the lungs and establish the relationship with the pleura, roots of the lungs and bronchi. The sensitivity of high-resolution computed tomography for detecting lung disease is about 94%, compared with 80% for chest x-rays. With CT, X-ray morphological manifestations of inflammatory processes in the lungs can be detected at earlier stages of the disease. Spiral computed tomography (SCT) makes it possible to significantly reduce the examination time, reduce the patient’s radiation exposure, and identify small nodules and pathological foci in the lungs that are not always detected with conventional CT. In many cases, SCT can replace invasive research - angiography. Picker has developed a new system for SCT that allows the principle of “virtual endoscopy” to be implemented. This system is intended primarily to identify patients with obstructive processes in the upper respiratory tract, which allows for advance selection of the biopsy site. This technique can be used as an independent technique, and also serve as a link between tomographic and conventional endoscopic examination. The patient's radiation dose during computed tomography does not exceed that received during a conventional x-ray examination.
Alternative methods of medical introscopy used in the diagnosis of lung diseases are ultrasound (US) and magnetic resonance imaging (MRI) - tomography based on the effect of nuclear magnetic resonance.
Ultrasound scanning provides information about the condition of the pleura, pleural cavity, and subpleural zones of the lung tissue. If there is a need to clarify the presence of a small amount of effusion in the pleural cavity that is not detected by conventional x-ray examination, and to determine its nature, it is better to use ultrasound. A new method of imaging in ultrasound is undergoing clinical trials - a specialized computer processing method for synthesizing ultrasound images with a large field of view using conventional hand-held ultrasound sensors, allowing the doctor to more fully register the structures being studied.
Magnetic resonance imaging, a non-invasive diagnostic method, has not yet received widespread use and requires further study and clarification. The advantage of MRI (Hitachi Medical, Siemens) over other methods is the assessment of the vascular bed of the pulmonary circulation.
Radionuclide research methods are used to determine the degree of impairment of regional blood flow and regional ventilation. The method complements radiographic data. It is technically simple, has no contraindications, and the radiation exposure is insignificant.
Currently, it is impossible to imagine a clinic that does not have a facility for conducting endoscopic examinations. Endoscopic methods, which were initially used exclusively for diagnostics, very soon turned into therapeutic ones and often compete with abdominal operations.
Bronchoscopy (Pentax, Karl Storz, Lomo) is performed after a mandatory preliminary x-ray examination of the chest organs in direct and lateral projections, since during bronchoscopy it is possible to examine the bronchi up to orders V–VI inclusive and the peripheral parts of the lungs cannot be seen. Indications for bronchoscopy are central or peripheral, benign or malignant lung tumors identified by x-ray, chronic bronchitis, bronchiectasis, long-term pneumonia, cystic fibrosis, lung abscess, hemoptysis and pulmonary hemorrhage of unknown etiology, mediastinal tumors and pleural pathology, foreign bodies of the tracheobronchial “tree” ", suspected tuberculosis.
If the patient has hemoptysis or a long-term cough during treatment with negative radiological data, as well as if the nature of the cough in a smoker changes, the indications for bronchoscopy are absolute.
Absolute contraindications to planned endoscopic examinations are myocardial infarction in the acute stage, stroke in the acute stage, cardiovascular and cardiopulmonary failure of the 3rd degree, paroxysmal tachycardia and atrial fibrillation.
Despite the fact that endoscopic examinations are increasingly being introduced into clinical practice every year, many doctors, especially in the outpatient network, are little familiar with the capabilities of diagnostic and, especially, therapeutic bronchoscopy and tend to exaggerate its danger. Of course, when using instrumental research methods complications cannot but arise, but due to the improvement of endoscopic devices (reducing the diameter and increasing the flexibility of the device), their number is reduced to a minimum, and they are, as a rule, not caused by the negligence or low level of training of the endoscopist , but the patient’s main or concomitant diseases. Currently, most medical institutions are equipped with modern, expensive endoscopic equipment, and it is unacceptable not to use it.
In our country, the most popular fiber endoscopes and video endoscopes are Japanese, Pentax and Olympas, as they are reliable in operation, have a small outer diameter and a large diameter of the biopsy channel, which is very important when performing medical procedures. In modern video endoscopes, thanks to the use of highly efficient lenses and precise digital signal processing systems using megapixel CCD matrices, it is possible to obtain a clear, high-quality image, magnified approximately 100 times, without deteriorating color rendition. Video endoscopes are more reliable in operation, since they can be bent at any angle and even tied in a knot without fear of damaging the endoscope. The load on the endoscopist's eyes has been significantly reduced. Thanks to the use of video endoscopes, it is possible to detect the smallest changes in the mucous membrane of the esophagus, stomach, duodenum and colon, as well as the trachea and bronchi, which makes it possible to diagnose cancer of these organs at an early stage of development.
Diagnostic endoscopic examination makes it possible to make a diagnosis, verify it morphologically, assess the extent of the process and develop optimal treatment tactics. Thanks to the constant improvement of endoscopic equipment and auxiliary endoscopic instruments, as well as the development and implementation of new treatment methods, many diseases can be treated through an endoscope.
Among all endoscopic research methods, bronchoscopy has long occupied a special place. Today, this is not only one of the first diagnostic methods, but also the most important and effective method of treating patients with chronic inflammatory and suppurative diseases of the nasopharynx, larynx, trachea and lungs.
As our many years of experience have shown, single courses of therapeutic bronchoscopy are effective for pneumonia, abscess pneumonia or lung abscess, and for chronic bronchitis, cystic fibrosis, bronchiectasis it is necessary to conduct therapeutic bronchoscopy in courses. The main medicinal substances that doctors use during therapeutic bronchoscopy are antiseptics, antibiotics, mucolytics and immunomodulators. During therapeutic bronchoscopy, it is possible to restore the drainage function of the bronchi, removing purulent contents from the bronchial “tree”, carry out a targeted effect on the bronchial microflora and administer drugs that reduce the viscosity of the secretion. Sanitation bronchoscopy is performed every other day. In this case, treatment can be carried out on an outpatient basis. Depending on the intensity of the inflammatory process in the bronchi, from 5–6 to 8–10 sanitation bronchoscopy per course of treatment is performed.
Of the surgical treatment methods during bronchoscopy, the most common are removal of benign tumors and removal of foreign bodies. The problem of diagnosis and removal of foreign bodies is especially relevant for pediatrics.
The method of removing benign tumors of the nasopharynx, larynx, trachea and large bronchi using radio wave coagulation (Surgitron device) is safe, since a coagulation scab does not form at the site of the cut-off tumor, as with electrocoagulation, which can be rejected on the 3rd–7th day and cause bleeding.
In conclusion, it should be emphasized that to identify the disease at an early stage of development, it is necessary to conduct a comprehensive examination, including clinical, laboratory, radiation, endoscopic and morphological studies. The efforts of doctors of various specialties should ultimately be aimed at early diagnosis of malignant diseases of the nasopharynx, larynx, trachea, bronchi and lungs.
In Russia, lung cancer ranks first in the structure of the incidence of malignant neoplasms and is diagnosed annually in more than 66 thousand patients.
Unfortunately, at present, as in past years, central lung cancer is most often diagnosed on the basis of clinical symptoms, the presence of which already indicates the widespread nature of the tumor lesion, i.e., in the late stage of the disease.
The most favorable phases for cure are the very initial phases of lung cancer development, when there is no metastasis yet or its probability is low. Currently, new methods of organ-saving surgery are being developed for this category of patients. These include various options for endobronchial surgery and therapy, including: electrocoagulation, cryodestruction, Nd:YAG laser surgery, brachytherapy and photodynamic therapy.
The curtailment in many countries, including Russia, of preventive screening programs and clinical observation in risk groups has reduced the already low percentage of early diagnosis of lung cancer. The only source of active mass detection of the disease at an early stage of development remains X-ray and bronchoscopic examinations undertaken for various benign lung diseases.
Improving the quality of early diagnosis of lung cancer is associated with the use of new preventive screening programs based on the use of computer questionnaires, new molecular, genetic biomarkers and highly informative methods of clarifying diagnostics: fluorescent bronchoscopy, low-dose spiral tomography, cytological examination of sputum using cytometry and immunocytochemical studies.
Technical development and improvement of these diagnostic methods is aimed primarily at increasing their resolving capabilities and identifying early cancer of minimal size, down to intraepithelial microfoci.
N. E. Chernekhovskaya , Doctor of Medical Sciences, Professor G. G. Fedchenko , Candidate of Medical Sciences A. V. Povalyaev RMAPO, Moscow
Examination of the ribs and sternum
A chest x-ray is usually sufficient to examine the ribs. In more complex cases, we will offer you additional research methods and assistance from specialized specialists.
The examination of the ribs is usually carried out in two directions: studying the structure of the ribs and searching for the cause of the disease of the ribs and sternum.
Study of the structure of the ribs and chest cavity
- X-ray (x-ray) of the ribs and chest. Chest X-ray (chest x-ray) allows you to reliably determine the condition of the bone tissue of the ribs of the sternum, identify the presence of deformities, fractures, etc.
- Computed tomography, magnetic resonance imaging of the ribs and chest (CT, MRI of the ribs) . In the event that a chest X-ray does not reveal any violation of the integrity of the bones, but the ribs and sternum hurt, it is advisable to conduct magnetic resonance imaging or computed tomography. These studies will give us a clearer idea than a chest x-ray about the nature of changes not only in the bone structure, but also in the connective tissue.

CT scan of the chest bones with 3D reconstruction. This image shows foci of calcification of the sternocostal joints as a result of a long-term inflammatory process.
- Osteodensitometry . This test allows you to judge your bone density. Most often, bone density is impaired due to osteoporosis (as with a fracture, when the density decreases, the ribs usually hurt), therefore, if bone density decreases, we will offer you a series of laboratory tests and a consultation with an endocrinologist. When performing a chest x-ray, one can judge the integrity of the bones, but the density of the cat’s tissue can be discussed in more detail when performing osteodensitometry.
- Examination for oncological processes. The ribs are a typical region of metastasis in breast cancer, myeloma and some other tumors. Metastases are not always clearly visible on conventional x-rays, so computed tomography is preferable. A blood test for tumor markers, protein fractions, and a general blood test can also be informative.
Additional Research
- Consultation with a rheumatologist. If your ribs hurt, and instrumental methods have not shown any changes, perhaps we are talking about an autoimmune disease that has begun. Our task is to prevent its development.
- Research for rheumatic diseases. We will offer you rheumatic tests and diagnosis of autoimmune diseases. These studies will show the presence and degree of activity of rheumatic disease. Often it is not the ribs that hurt, but the sternocostal joint, damaged by the rheumatic process. It is possible to say reliably about the nature of the disease only after conducting a study for rheumatic diseases. More details…
- Consultation with a neurologist if there is suspected entrapment of the intercostal nerves (intercostal neuralgia).
- Immunological examination. Infections often act as provocateurs of various autoimmune diseases. Our task is to determine what kind of infection provoked the disease of the ribs and sternum. Read more…
Indications and contraindications for chest MRI
Magnetic resonance diagnostics is carried out by exposing the human body to magnetic fields. High-frequency response impulses from tissues exposed to electromagnetic radiation are converted by sensors into a layer-by-layer computer image, through which the doctor can examine the internal organs.
MRI of the chest and mediastinum may be recommended in the following cases:
- suspicion of tumors (including cancer) in the lungs;
- determination of the involvement of adjacent tissues in the pathological process (in the study of malignant tumors);
- assessment of the anatomical structure of the heart if pathology is suspected;
- assessment of myocardial blood flow after a heart attack or microinfarction, the dynamics of blood flow in the parts of the heart;
- diagnosis of inflammation of the lymph nodes;
- diagnosis of spinal diseases in the mediastinum, assessment of the condition of muscles and adipose tissue;
- assessment of the condition of the pericardium;
- clarifying diagnosis of diseases previously identified using other methods.
Doctors do not often prescribe MRI of the chest organs, mainly for differential diagnosis. To study blood vessels and arteries, MRI with a contrast agent is performed - magnetic resonance angiography.
Despite the non-invasiveness, painlessness and relative ease of the procedure, it is worth remembering that it also has contraindications. MRI cannot be performed on people with installed artificial heart valves, stents in blood vessels, pacemakers, insulin pumps or other implanted electronic devices. MRI is performed with caution (only as prescribed by a doctor) during pregnancy, lactation, mental disorders and claustrophobia.
This is important. A contraindication for magnetic resonance angiography is an allergy to the contrast agent.