What is bilirubin?
Just over half of newborns become noticeably icteric in the first week of life. This infantile jaundice usually goes away in 2-4 weeks. What causes jaundice in children? Jaundice is a yellowing of the skin and whites of the eyes caused by hyperbilirubinemia - that is, an increase in the concentration of bilirubin in the blood serum.
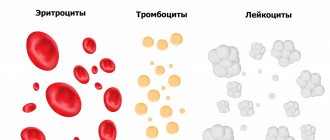
Bilirubin is a yellow-orange natural pigment that is released during the natural breakdown of red blood cells - erythrocytes: as a result of the breakdown of hemoglobin into unconjugated bilirubin. The liver clears the blood of excess bilirubin by filtering it out and converting it from the free form (unconjugated) to the bound form (conjugated with glucuronic acid), which enters the bile and digestive tract, exiting along with the stool, giving it its characteristic color.
What causes jaundice?
Jaundice occurs when there is too much bilirubin in the blood.
It can be elevated due to many factors: abnormalities in the liver, impaired flow of bile (bile itself contains bilirubin) from the gallbladder and bile ducts, blood disorders in which too many red blood cells containing bilirubin are broken down. Bilirubin is a yellow substance produced by the breakdown of red blood cells that carry oxygen throughout the body. When red blood cells die, the liver filters their breakdown products from the bloodstream. But with pathologies (diseases of the liver and bile ducts, increased destruction of red blood cells), the liver may not keep up with this process, bilirubin accumulates, and the skin, sclera of the eyes and mucous membranes become yellow.
Types of jaundice
There are several types of jaundice, and depending on this, the mechanism of damage differs.
There are three types of jaundice:
- Prehepatic (hemolytic) jaundice. Occurs when too many red blood cells break down. This process is called hemolysis. When too many red blood cells break down at once, large amounts of bilirubin are released that the liver cannot handle. This happens, for example, with hereditary types of anemia, when a person’s red blood cells (red blood cells) have a special shape and are prone to faster destruction.
- Hepatic (parenchymal) jaundice. This type is associated with liver damage, which affects the organ's filtering ability and causes too much bilirubin to enter the bloodstream. This is possible with liver infections, hepatitis, cirrhosis.
- Subhepatic (mechanical) jaundice. This type of jaundice occurs due to blockage of the bile ducts connecting the liver, gallbladder and intestines.
The bile ducts are a series of tubes that are similar to blood vessels but are responsible for carrying bile from the liver to the gallbladder. If an obstruction does not allow the liver to remove excess bilirubin, serious disruptions occur in its functioning, which in turn provoke jaundice. This happens due to gallstones, enlarged lymph nodes or tumors.
Causes of hyperbilirubinemia
Hyperbilirubinemia almost always indicates pathology. However, there are exceptions. For example, the cause of hyperbilirubinemia can be prolonged fasting (deficiency of albumin, cellular carrier proteins), the use of drugs that cause competitive inhibition of the uptake of bilirubin by hepatocytes (radiocontrast agents, drugs for the treatment of helminthiases).
In newborns, the cause of hyperbilirubinemia is physiological jaundice, which develops due to the immaturity of the enzyme systems of bilirubin metabolism. The causes of pathological hyperbilirubinemia are as follows (listed in order of frequency):
- Liver diseases
. The most common cause of hyperbilirubinemia. The destruction of hepatocyte membranes leads to the release of bilirubin and its entry into the bloodstream. This occurs with any infectious liver lesions (viral, bacterial, protozoal hepatitis), alcoholic, autoimmune hepatitis, cirrhosis. - Diseases of the biliary tract
. The second most common cause of hyperbilirubinemia. As a result of intrahepatic and extrahepatic cholestasis, which is observed with cholecystitis, cholelithiasis, cholangitis, the permeability of bile capillaries increases. Under the influence of high hydrostatic pressure, bilirubin diffuses into the blood vessels. - Hemolytic anemia (HA)
. With increased destruction of red blood cells (hemolysis), the amount of free bilirubin in the blood increases. This is typical for both congenital (hereditary microspherocytosis, sickle cell anemia, thalassemia) and acquired hemolytic anemia (paroxysmal nocturnal hemoglobinuria, autoimmune, drug-induced HA). - Hereditary enzymopathies
. Genetically determined defects in the enzymes of hepatic metabolism of bilirubin lead to disruption of its uptake by hepatocytes, conjugation with glucuronic acid, or secretion into bile. This group of diseases is called benign hyperbilirubinemia (Gilbert, Crigler-Nayar, Dabin-Jones syndrome). - Metabolic disorders
. These are rare hereditary diseases that affect the liver parenchyma, in which bound bilirubin enters the blood. These include hemochromatosis, Wilson-Konovalov disease, lysosomal storage diseases (Gaucher disease, Niemann-Pick disease). - Pathology of the upper gastrointestinal tract
. Some diseases of the digestive system (pseudotumorous pancreatitis, pancreatic tumor, stenosis of the major duodenal papilla) can create a mechanical obstacle to the outflow of bile due to compression of the bile ducts, thereby leading to their overflow, diffusion of bile pigment into the capillaries.
Symptoms of jaundice
From the name of the syndrome it is clear what the main symptom is.
With jaundice, the whites of the eyes, skin and other tissues of the human body turn yellow. Interestingly, the shade of yellow suggests the type of jaundice. With hemolytic jaundice, the skin becomes pale and acquires a light yellow, lemon tint. For liver diseases - orange. With mechanical jaundice, the skin darkens and becomes earthy, greenish in color. Jaundice caused by acute illness is usually accompanied by fever, chills, abdominal pain, flu-like symptoms, dark urine, and light-colored stools.
If jaundice develops as a result of chronic pathology, there may be symptoms such as weight loss or itchy skin. Jaundice caused by cancer of the pancreas or biliary tract may be accompanied by abdominal pain.
Jaundice in children
A common occurrence is jaundice in newborns.
As in adults, infantile jaundice is associated with increased levels of bilirubin in the blood, but in the vast majority of cases it does not pose a serious threat to life or health. Jaundice is one of the most common syndromes encountered by newborns. According to statistics, almost 60% of full-term babies and 80% of those born prematurely (before the 37th week of pregnancy) have varying degrees of jaundice at birth. Moreover, 60-70% of this number are faced with a physiological, rather than pathological form of jaundice. And only one in 20 babies has high bilirubin levels that require treatment.
Symptoms of neonatal jaundice usually develop 2–3 days after birth and disappear without treatment by 2 weeks. Most hospitals screen children for jaundice before discharge. Despite the fact that jaundice in newborns usually goes away without medical help, at the first symptoms it is necessary to show the baby to the doctor so that the specialist can determine the cause of the yellow sclera or yellow skin and give individual recommendations.
Jaundice is common in newborns because babies' red blood cells break down more quickly. In addition, a newborn's liver is not fully developed, so it does not remove bilirubin from the blood as efficiently as it does in an adult. Plus, the low content of bacteria in the intestines of newborns also affects the exchange of bilirubin, increasing its content in the blood. Usually, by the end of the second week of a baby’s life, his liver begins to cope with the amount of bilirubin, and the level returns to normal.
Treatment is usually only recommended if tests show very high levels of bilirubin in the baby's blood. In especially high quantities, bilirubin has a neurotoxic effect, meaning it can harm the baby’s brain. The extent of the damage depends on the duration of the jaundice and the degree to which bilirubin is elevated.
Phototherapy is often used to reduce a baby's bilirubin levels. Light from a special lamp shines on the skin and converts bilirubin into a form that is more easily broken down by the liver. In rare and severe cases, an exchange transfusion is used: the baby's blood is removed through a catheter and replaced with blood from a suitable donor. Most babies respond well to treatment and are discharged from the hospital within a few days.
Treatment of jaundice in newborns at home
The main treatment method for indirect hyperbilirubinemia (newborn jaundice) is phototherapy (phototherapy) - treatment with light from the blue spectrum of radiation. At the same time, under the influence of blue light, bilirubin is destroyed and eliminated naturally from the baby’s body.
For phototherapy of newborns, only special blue light lamps (photoirradiators) are used. Treatment takes several days, the duration of therapy is determined by a pediatrician. Photoisomerization of bilirubin occurs in the child’s skin, therefore, the larger the body area used for phototherapy, the more effective the treatment process. The lamp for the treatment of jaundice in newborns is a bath made of harmless plastic, in the base of which blue light lamps are mounted. During the procedure, the baby is placed in a removable hammock.
The total session lasts at least 14 hours, treatment must take place in the presence and under the supervision of parents. The child should not be left alone in the device without supervision.
Jaundice in adults
Jaundice is less common in adults than in children and can occur for many reasons, including:
- Hepatitis. This is an inflammatory disease of the liver, often caused by a virus. Hepatitis can be acute (completely curable) or chronic. Other causes of hepatitis: medications, drugs, alcohol, autoimmune diseases. Such liver damage eventually leads to jaundice.
- Blocked bile ducts. These thin tubes carry bile from the liver and gallbladder to the small intestine. Gallstones and tumors can block the ducts.
- Pancreatic cancer: It is the 10th most common cancer in men and the 9th most common cancer in women.
- Blood disorders that cause rapid breakdown of red blood cells.
How to do phototherapy at home correctly
The use of a UV lamp for the treatment of jaundice in a newborn is prescribed by a pediatrician. You should not self-medicate and make prescriptions yourself. You can rent a UV lamp and use it yourself; the physiotherapist or pediatrician who prescribed the treatment will explain to you in detail how to use the lamp, outline the number and duration of sessions, and tell you safety measures.
Practical recommendations for phototherapy:
- Phototherapy is carried out only with a special medical lamp for newborns!
- Any other lamps (for example, for photography, or for tanning, solarium lamps) can not only harm a child, they can be deadly for him.
- the room temperature must be at least 26 degrees.
- The child's genitals must be protected; to do this, simply put a diaper on the baby.
- Every 2 hours it is necessary to measure the child’s body temperature
- the daily volume of fluid that the child receives must be increased by 10–20%
- phototherapy can be discontinued if there are no signs of a pathological increase in bilirubin, and the concentration of total bilirubin in the blood serum has become below the values that served as the basis for starting phototherapy;
- 12 hours after the end of phototherapy, a control test of blood bilirubin is necessary
IMPORTANT TO KNOW: the photo lamp of our medical center has a special “pocket” where the mother places the newborn. In this case, the child’s body is irradiated, and the head and face are located outside, outside the irradiated surface. Our lamp is very easy to use, no special knowledge or skills are needed, just put on the baby's diaper (so that the genitals are not exposed to radiation), put the baby in the pocket, and carefully fasten the zipper.
Irradiation of the body by ultraviolet rays with light from the blue spectrum leads to photoisomerization (decomposition) of large molecules of bilirubin, converting it into water-soluble products that are easily and quickly excreted by the kidneys with urine or the liver into bile through the gastrointestinal tract.
Gilbert's syndrome
Separately, it is worth highlighting Gilbert's syndrome - a common hereditary disease, also known as constitutional liver dysfunction and familial non-hemolytic jaundice.
It does not require treatment, and many doctors do not consider it a disease and consider it as a variant of the norm and an individual feature. Gilbert's syndrome occurs in 1-5% of the population, depending on the region. It is associated with a defect in the gene that is responsible for the production of a liver enzyme. Thanks to this enzyme, indirect bilirubin binds. In a third of Gilbert's syndrome carriers, the pathology does not manifest itself throughout life. It is often asymptomatic and is detected only by a blood test for bilirubin. However, more pronounced symptoms are also possible: pain in the right hypochondrium, metallic taste in the mouth, flatulence, vomiting, general weakness and fatigue, loss of appetite, insomnia. Symptoms are varied, and often patients with Gilbert's syndrome experience low mood, irritability, and anxiety.
There is usually no specific treatment for Gilbert's syndrome. The patient needs to limit the amount of fatty foods in the diet, adhere to a healthy lifestyle and visit a gastroenterologist - he is the one who diagnoses and treats this disease.
Classification
Depending on which fraction of bile pigment is increased, there are:
- Indirect hyperbilirubinemia
. Unconjugated (unbound) bilirubin is increased. The cause is pathologies that cause suprahepatic jaundice - hemolytic anemia, benign hyperbilirubinemia. - Direct hyperbilirubinemia
. Accompanied by an increase in the level of conjugated (bound) bilirubin. The cause is diseases leading to hepatocellular and subhepatic jaundice. The most common of them are viral, alcoholic hepatitis, cholecystitis.
Bilirubin encephalopathy (kernicterus) is distinguished separately. It occurs in hemolytic disease of newborns, the cause of which is the incompatibility of erythrocyte antigens (Rh conflict) of the mother and fetus. This disease is very serious, it is characterized by damage to the subcortical nuclei and cerebral cortex and requires immediate treatment.
Diagnosis and treatment of jaundice
A preliminary diagnosis can be made based on skin color, but we repeat that jaundice is not a disease, but a syndrome.
Therefore, all further diagnostics after the initial examination will be aimed at identifying the cause of the symptoms. If the skin or sclera turns yellow, the following tests must be taken:
- general blood analysis;
- general urine analysis;
- biochemical blood test, including a blood test for total bilirubin and direct bilirubin;
- urine test for total bilirubin and direct bilirubin;
- blood for antibodies to viral hepatitis.
The next stage is hardware diagnostics.
Ultrasound of the liver and biliary tract is often required. If prescribed by a doctor, an MRI or tomography may also be performed. Treatment is selected individually, depending on the causes of jaundice, the condition of the internal organs and the results of the studies. Jaundice has many types and manifestations, and its treatment is also varied.
Different specialists deal with different types of jaundice: therapists, infectious disease specialists, hematologists, oncologists. Which specialist will become the primary attending physician will become clear as a result of the examination. It is right to start the examination by taking laboratory tests and contacting a therapist.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
What to do if there are signs of increased bilirubin
It will not be possible to normalize bilirubin levels without laboratory tests, because first of all you need to find out the reason for the change in the amount of pigment in the blood. This means that you need to check the level of ALT and AST enzymes, do an analysis for viral hepatitis and an ultrasound of the liver.
If the increase in bilirubin is caused, for example, by cholelithiasis, then cholecystectomy (removal of the gallbladder) or drug therapy with ursodeoxycholic acid is indicated. If viral hepatitis occurs, antiviral therapy is necessary. If a person has a parasitic disease, the helminths must be destroyed. Those. the scheme of action depends entirely on the condition that led to the increase in bilirubin.