Hysteroscopy is a procedure for examining the uterine cavity using a device that creates multiple magnification. There is a classic hysteroscopy - it is usually performed under anesthesia, requires large instrumental dilatation of the cervix and ends with curettage of the endometrium. And there is an “office” option - this is a mini-option, used only for diagnostic purposes, does not require pain relief, and is carried out in a antenatal clinic.
During office hysteroscopy, the endometrium is not removed, and therefore the procedure does not have any effect on the duration of the cycle. Even if in the process the doctor took a pinch - an endometrial biopsy. But the first option, with curettage, can disrupt the cycle and change the nature of menstruation.
Back to contents
When does your period come?
Hysteroscopy combined with RDV is routinely performed in the last days of the menstrual cycle, 26-27, but before bleeding begins. In this case, there is no double monthly bleeding (during and after the procedure and on those days when menstruation should begin according to its due date). After all, even if the doctor had not surgically removed the upper mucous layer of the uterus, it would normally begin to peel off in the coming days or even hours. In this case, the first menstruation (not to be confused with discharge after the procedure) begins in about a month. The day on which there was medical intervention should be considered the first day of the cycle.
Office diagnostic hysteroscopy is performed in the first half of the cycle in order to better examine the uterine cavity without the risk of the presence of a fertilized egg in it. If the procedure was performed on the 10th day of the cycle, then your period can be expected in about 18 days.
Back to contents
What should be your period after the procedure?
Changes in the characteristics of menstruation are no less important than the timing of when your period arrives. In most cases, the first discharge of blood is less abundant. Gynecologists consider the appearance of scanty periods after hysteroscopy to be a consequence of curettage: the main volume of menstrual flow is the rejected endometrium, which is almost absent after the procedure. The decrease in the volume of secretions continues until the endometrium is completely restored.
Much more often than scanty discharge, patients are bothered by very heavy periods. Sometimes they hide uterine bleeding that occurs against the background of an inflammatory process or perforation of the uterus. The following signs will help you understand that heavy periods are a pathology:
- dark or brown periods;
- unpleasant odor of discharge;
- release of large clots;
- increased body temperature;
- intense abdominal pain.
All these symptoms require immediate contact with a gynecologist. Consultation is also necessary in cases where heavy discharge continues for a long time without stopping. This process is fraught with a decrease in hemoglobin and a significant change in hormonal levels.
What to do if periods are painful
Often, painful periods become the reason for hysteroscopy. If she required curettage, pain may persist during the first cycle. In general, pain is a normal reaction to injury to the endometrium, so it should not cause concern. To reduce it, you can take an antispasmodic or NSAID.
The exception is when the symptom becomes painful and intensifies when walking, after eating and while visiting the toilet. In this case, the patient needs to consult a gynecologist.
How is hysteroscopy done: before or after menstruation?
On what day hysteroscopy is performed depends on the purpose of the procedure. For example, to identify tumors and polyps, the procedure is carried out in the first phase of the cycle, that is, immediately after menstruation. During this period, the endometrium lining the uterus is thinner, and tumors are better visible on it. Inflammatory processes are easier to detect when the endometrium is swollen, so diagnosis of suspected endometritis is carried out on the eve of menstruation in the second phase of the cycle.
Conducting a hysteroscopy the day before menstruation is less informative, since the endometrium becomes loose and may begin to bleed. However, the procedure can be performed for urgent reasons.

Can the procedure be performed during or before menstruation?
Doctors can perform hysteroscopy during menstruation only in emergency cases:
- with intense bleeding, in which tampons and pads become completely wet in 1-2 hours;
- if there is a suspicion of the presence of a dead fertilized egg in the uterine cavity;
- if you suspect the presence of foreign objects in the uterus;
- if you suspect uterine rupture.
Gynecologists recommend that patients remain in the hospital for further observation on the first day after hysteroscopy during menstruation.

If there is no menstruation
You need to make sure that pregnancy has not occurred. It is possible within 2-3 weeks. If conception is excluded, the pregnancy test is negative, and apart from the absence of menstrual periods, there are no complaints, we continue to wait. The fact is that the endometrium needs some time to recover, especially if the curettage (EDV) was rough, the upper layer of the uterus was completely removed.
Often after the procedure, doctors prescribe oral contraceptives (OCs) for several months, depending on the patient’s reproductive plans. Then there are usually no problems with the cycle. Withdrawal bleeding occurs within 7 days after finishing the drug package.
When OCs were not taken, and more than two months have passed since the RDV, it is time to do an ultrasound and visit a gynecologist. If ultrasound shows signs of progesterone deficiency, progesterone is prescribed (Duphaston or Utrozhestan). After finishing taking them, menstrual-like bleeding begins.
There are also more serious reasons for the absence of monthly bleeding after hysteroscopy - these are hormonal disorders, including those arising from the approaching menopause or problems with the ovaries (polycystic disease). But they usually do not occur all at once. If a woman has previously had delays in menstruation, then the cause should not be looked for in this diagnostic procedure.
Back to contents
Menstruation after hysteroscopy and its nature
The nature of menstruation after hysteroscopy depends on the woman’s reaction to the manipulations, treatment procedures, as well as her ability to recover. They can begin exactly on time, or with a slight delay or, conversely, earlier, become abundant or scanty, long-lasting or shortened - all these are variants of the norm.
If menstruation after hysteroscopy is so heavy that a woman has to change hygiene products very often (every 2 hours), then it is best to consult a doctor. If menstruation after hysteroscopy has an unpleasant odor, a brown color, and the patient has severe pain in the lower abdomen, then it is necessary to immediately consult a specialist, because these signs may indicate inflammation.
Normally, after the procedure, the patient may feel slight discomfort and discharge, which goes away on its own within 2-4 days. Sometimes a woman mistakes heavy bleeding for menstruation after hysteroscopy, so if it does not decrease in volume and lasts more than 4 days, she does not pay attention to it. But this should alert the patient, because this may be a symptom of a complication of the procedure and threaten life and her health.
Too scanty or short periods
If, during a mini-operation, a problem was removed that was causing heavy menstruation, for example, a polyp or submucosal uterine fibroid, then it is quite natural that monthly bleeding will become moderate or even scanty. Oral contraceptives and hormonal intrauterine device significantly reduce blood loss.
During menstruation, blood loss should not be less than 30 grams, and bleeding should end too early (last less than 3 days).
If there is only a dark, brown daub, and more than one month after gynecological intervention, there is a suspicion of the formation of intrauterine synechiae. These are films, adhesions that envelop the walls of the uterus or cervical canal. Their formation is not a mistake of the doctor curettaging the uterus, but a frequent complication of RDV. It’s not for nothing that they are now trying to prescribe it as rarely as possible to women of reproductive age, only for strict indications. This pathology is also called Asherman's syndrome.
Adhesions cause scanty, short and infrequent menstruation, as well as infertility. They are removed during repeated hysteroscopy.
If there is evidence of adhesions only in the lumen of the cervical canal, an easier and less traumatic procedure is performed - bougienage.
Important! On ultrasound, intrauterine synechiae are not clearly visible. They can only be suspected based on the clinical picture.
Diagnoses associated with Asherman syndrome:
- endometrial hypoplasia;
- endometrial atrophy.
After cutting the adhesions, a relapse may occur again, so women planning pregnancy should not postpone it for a long time after treatment.
Back to contents
Possible consequences of the procedure
Despite the safety of this examination, a woman may experience some health complications, many of which will only be temporary. For example, pain after hysteroscopy is considered commonplace, because this is a natural reaction of the human body to instrumental intervention. Such uncomfortable sensations pass quite quickly, but due to differences in the pain threshold they can be tolerated differently. To get rid of this effect of the procedure, you can consult a doctor for a prescription for a pain reliever. Also, do not forget about precautions that will prevent pain after hysteroscopy from lasting longer than usual, and will help avoid various complications. These include temporarily refusing to use sanitary tampons, douching, physical activity and sexual activity. However, it is best to check the restrictions with the doctor who performed the procedure. You should also contact him if the pain does not go away within a week.
Heavy, prolonged and painful menstruation
Hysteroscopy itself does not cause dysmenorrhea and menorrhagia. And the problem usually manifests itself even before it occurs. Possible reasons:
- coagulopathy
is an inherited problem with blood clotting; - adenomyosis
(internal endometriosis); - hormonal disorders
that provoke excessive growth of the endometrium - hyperplasia; - endometrial cancer
; - Uterine fibroids
are a benign neoplasm located outside the uterus or inside its wall, which does not allow its removal with a hysteroresectoscope, that is, from the inside, laparoscopy or abdominal surgery is required.
Heavy menstruation should be considered blood loss of more than 80 grams on all days.
Treatment is prescribed depending on the cause - surgical or conservative (taking hormonal or hemostatic pills, installing the Mirena intrauterine system), otherwise in the case of a non-gynecological disease.
If the second period comes too early, 1-2 weeks after the first, it comes heavily and is scarlet in color, then this should be regarded as uterine bleeding. He needs to be stopped. Usually, hormonal pills according to a certain scheme and hemostatic drugs are used for this.
Back to contents
The effect of hysteroscopy on the menstrual cycle
Normally, menstruation after hysteroscopy should begin at the patient’s usual time. However, everything will depend on the goals of hysteroscopy and the technique of its implementation. After a routine diagnostic examination, a cycle failure is unlikely, since the mucous membrane is not affected or is only slightly injured.
Things are somewhat different when combining diagnosis and treatment. For example, after resectoscopy of tumors, including removal of a polyp from the uterine cavity, or hysteroresectoscopy of fibroids, hormonal levels are often disrupted, so changes in the menstrual cycle occur frequently. Until the body restores the integrity of the uterine mucous membranes after hysteroresectoscopy, you should not expect regular periods.
A similar situation is created when diagnosing with curettage in classical or separate (RDV) formats; extensive trauma to the endometrium occurs, so the recovery period may be longer than during a regular examination.
Important! Significant cycle disruption after hysteroscopy is observed in approximately 5% of patients. In most cases, this is due to the unsatisfactory general condition of the body and the presence of serious pathologies.
When will your period start after hysteroscopy?
Experts expect the start of the first menstruation after hysteroscopy at the usual time for the patient. The period when they should begin is calculated in advance. However, your first period may come a few days earlier or later than your normal cycle. On average, the onset of bleeding may vary by several days or even a week, up or down.
It is possible to predict with an accuracy of up to a day when your period will begin after hysteroscopy only on the basis of a pre-existing calendar of regular bleeding. For patients who underwent the procedure in the first phase of the cycle, they will return no earlier than in 2-4 weeks. For those who had hysteroscopy in the second or third phase of the cycle, menstruation usually begins within 3-7 days.
Could there be a delay and for how long?
Gynecologists say that a delay after hysteroscopy is normal, since the body needs time to recover. It usually takes about 4 weeks for endometrial tissue to regenerate, so menstruation may begin 1-2 weeks later. In rare cases, disruptions occur over several cycles, for example, bleeding appears later for three months in a row.
Doctors call an alarming symptom a long delay, in which there are no periods at all for 7 weeks after hysteroscopy, and discomfort appears in the lower abdomen, lower back and perineum. This may indicate a spasm of the cervix, as a result of which blood and exfoliated endometrium cannot leave the organ cavity. Such a delay in menstruation is fraught with dangerous complications and requires immediate medical intervention.
What if your period started early?
Many women think that after hysteroscopy, periods begin without interruption, especially if polyps or other tumors were excised during the intervention. In fact, this is not so: the period when menstruation begins in the classical sense remains the same, but in practice postoperative bleeding occurs. However, cases when critical days came earlier or immediately after the intervention are not uncommon.
Sometimes it is difficult for patients to understand whether their bleeding is normal or abnormal. Gynecologists advise paying close attention to the nature and intensity of the discharge if it occurs earlier than expected. Heavy bleeding with clots may indicate a serious problem that requires medical attention.

How many days does your period last after the procedure?
The duration of menstruation after hysteroscopy usually does not change. The exception is cases when the onset of menstruation after hysteroscopy with curettage, which is always accompanied by bleeding, occurs 3-5 days after the intervention. In this case, the total duration of bleeding will be longer. The next period will last as usual.
When to see a doctor
In most situations, the doctor warns the woman about the possible consequences, prescribing preventive treatment in the first 3 to 5 days after the manipulation. The gynecologist also explains whether after hysteroscopy menstruation can begin immediately in this situation, or wait until after a month.
As a rule, antibacterial drugs, antispasmodics and other painkillers, hemostatic agents, herbal medicine, and, if necessary, hormones are prescribed.
But not everything can always be foreseen. In the following situations, you should seek medical help unscheduled:
- with painful menstruation uncharacteristic for a woman;
- when an unpleasant odor appears along with discharge from the genital tract, possibly of a purulent or putrefactive nature;
- if bleeding continues for more than 7 - 10 days immediately after hysteroscopy;
- in the case when the onset of menstruation is excessively heavy, with clots, more than 50 ml/day;
- long periods after hysteroscopy in the first cycle - more than 7 days;
- when severe abdominal pain occurs;
- in case of a temperature rise of more than 38 degrees, not associated with a cold, etc.
Self-medication in such situations is life-threatening; if assistance is not provided in a timely manner, there is a high risk of developing even more serious complications.
Briefly about the purpose of the procedure
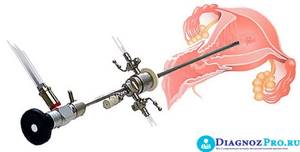
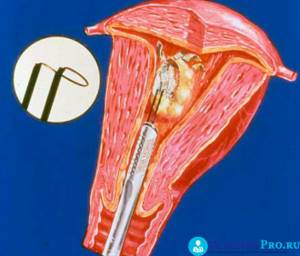
Hysteroscopy is an endoscopic research method. During the procedure, a special probe is inserted into the uterine cavity, which contains a light guide and a conductor for the camera. In this way, the resulting image can be displayed on the monitor screen, and it is easier to monitor it, and can also be recorded on a medium and then compared during the treatment process. A hysteroscope involves the possibility of removing pathological formations (polyps, submucous nodes, septum in the uterine cavity, etc.), performing a biopsy and other manipulations.
The procedure can be carried out for diagnostic purposes to clarify the prevalence of the pathological process and identify the cause of the disease. It is also performed as a therapeutic technique.
Hysteroscopy is often combined with curettage of the uterine cavity and cervical canal, followed by histological examination of the material.
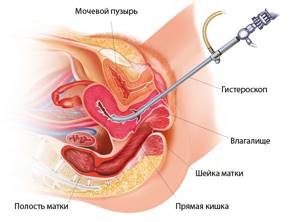
Carrying out hysteroscopy
Indications for hysteroscopy:
- Acyclic uterine bleeding. Conventional curettage only results in complete removal of the endometrium in 40-45% of cases and often does not involve pathological areas.
- Bloody discharge during menopause. The fact is that the pathological process, including endometrial cancer, can be very small. With normal scraping, you may not touch it, which leads to a false result.
- Menstrual irregularities of unspecified cause.
- To remove the intrauterine device when it grows in due to prolonged exposure or when the antennae break.
- If there is a suspicion of remnants of the fertilized egg or placenta, hysteroscopy is also an advantage.
- To control treatment, including hormonal.
- Hysteroscopy can effectively remove polyps, small submucous myomatous nodes, septum or adhesions in the uterine cavity.
- For some pathology of the fallopian tubes (narrowing of the mouths), the procedure is indicated.
- As a therapeutic tactic for endometrial hyperplasia, especially in recurrent forms.
Watch the video about the procedure:








