In what cases is blood transfusion performed?
Whole blood cannot be transfused; it is possible to use only its components, such as fresh frozen red blood cells and platelet concentrate. One of the main indications for blood transfusion is a hemoglobin level of less than 70 g/l and a decrease in saturation (oxygen saturation of the blood) to 80%. The procedure is necessary for the disintegration of massive tumors; the disintegration process is accompanied by chronic blood loss. Usually these are tumors of the uterus, vagina, and cervix. And such an oncological problem as melanoma has a depressing effect on the red blood cell, in this case, in order to carry out chemotherapy, it is necessary to restore the normal level of red blood cells and hemoglobin, so a blood transfusion is performed.
The need for a transfusion of fresh frozen plasma is due to profuse edema and the presence of a state of suppressed hematopoiesis; this transfusion is also carried out to prevent the development of disseminated intravascular coagulation syndrome with a sharp inhibition of blood clotting.
When to Transfuse Patients with MI and Anemia: The REALITY Study
Relevance
It is well known that anemia is a factor that increases the poor prognosis of patients with myocardial infarction. On the one hand, in order to improve the blood supply to the myocardium with oxygen, early correction of anemia seems logical, but on the other hand, red blood cell transfusion increases the risk of stent thrombosis and infections. Therefore, the purpose of the REALITY study was to compare two approaches to transfusion of red blood cells in patients with myocardial infarction: when hemoglobin decreases ≤80 g/l with a goal of 80-100 g/l and when hemoglobin decreases ≤100 g/l with a goal of >110 g /l.
Methods
The randomized study included patients with myocardial infarction and anemia, whose hemoglobin level was in the range of 70-100 g/l.
Patients with cardiogenic shock, myocardial infarction caused by percutaneous coronary intervention or coronary artery bypass grafting, blood transfusion in the previous 30 days, known hematologic disease, and major bleeding were excluded.
Patients were randomized into two groups: red blood cell transfusion when hemoglobin decreased ≤80 g/L with target values of 80-100 g/L and red blood cell transfusion when hemoglobin decreased ≤100 g/L with target values >110 g/L.
Follow-up was 30 days, and the primary endpoint included all-cause death, reinfarction, stroke, and emergency revascularization.
results
- The study included 666 patients, with a mean age of 77 years and 43% women.
- 35.7% of the ≤80 g/L group and 99.4% of the ≤110 g/L group received at least 1 dose of packed red blood cells (p<0.0001). However, the incidence of the primary endpoint was not significantly different between the two groups: 11% versus 14% (hazard ratio 0.77; 95% confidence interval 0.5-1.18; p<0.05 for noninferiority analysis).
- The incidence of deaths was also comparable (5.6% vs. 7.7% p>0.05), but the incidence of infections and acute lung injury was statistically significantly higher in the ≤100 g/d group.
Conclusion
Thus, the results of this study convincingly demonstrated that there is no need for red blood cell transfusion only when hemoglobin decreases ≤100 g/L in patients with myocardial infarction and anemia.
Source:
acc.org/latest-in-cardiology/clinical-trials/2020/08/29/13/09/reality?fbclid=IwAR1r6lyMA-EUpkF7Si6m82dYPDdA6S29Er7rxW5iaIR5KFC1MXNmYGQQ8ek
Blood transfusion procedure
Upon admission to the hospital, each patient's blood group according to the ABO system and antigens are checked. If a patient has a negative KO (Kell system), then he is allowed to use only blood with similar characteristics for transfusion. If this rule is not followed, hemolysis will occur and the red blood cells will be destroyed by the patient's own antibodies.
Also, before each blood transfusion procedure, the blood group according to the ABO system and the Rh factor, a compatibility test between the patient and the donor, and a biological test must be carried out (20-25 ml of blood is administered and the patient is monitored for 15 minutes). If the Rh factors, blood group match, the compatibility test is positive and there are no abnormalities in the biological test, further blood transfusion is carried out.
It is possible to individually select various blood components for patients with existing Rh conflict, hemolytic anemia and multiple previous transfusions. For such patients, a gel test is performed in a specially equipped blood bank laboratory.
Contraindications to blood transfusion
Absolute contraindications to transfusion are an acute state of cardiovascular failure, cardiopulmonary failure accompanied by pulmonary edema, myocardial infarction.
Important! The doctor may perform a transfusion even if there are contraindications if the procedure can save the patient's life.
Relative contraindications for blood transfusion:
- thrombosis and embolism;
- severe cerebrovascular accidents;
- septic endocarditis;
- heart defects;
- myocarditis and myocardiosclerosis with circulatory failure;
- stage III hypertension;
- severe functional disorders of the liver and kidneys;
- bronchial asthma, polyvalent allergy;
- tuberculosis;
- rheumatism, especially with rheumatic purpura.
Blood transfusion is a complex procedure with many contraindications, causing possible complications in some cases. A transfusion is prescribed if the hemoglobin level falls below 65 g/L. Blood transfusion can save a person’s life in a critical situation, therefore, despite all the possible disadvantages of the procedure, it is still used for adults and children. To prevent complications, it is necessary to strictly observe all stages of preparation for transfusion, especially individual compatibility and Rh compatibility.
What does transfusion help with?
Solid tumors lead to significant changes in the hematopoietic system. Under their influence, anemia and abnormalities in the blood clotting system can develop.
The disintegration of tumors leads to depletion of the bloodstream and blood reserve of the body. Surgical treatment also leads to massive bleeding. All of the above factors lead to the fact that the body’s own reserve is depleted and it requires a blood transfusion from a donor. Due to insufficient blood volume, treatment may be delayed because In case of anemia and thrombocytopenia, chemotherapy cannot be administered.
Chemotherapy drugs can have side effects on blood germs and worsen thrombocytopenia. That is why constant monitoring of red and white blood indicators and coagulation properties is necessary. If any deviations from the norm are noted, blood transfusion is prescribed according to all rules.
Indications for blood transfusion
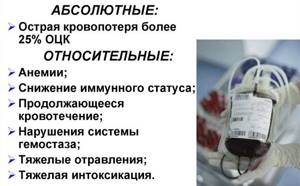
Indications can be absolute and relative. Absolute indications include extensive blood loss, traumatic shock, and major tissue damage during severe operations. The rest of the readings are relative. Among them are anemia, severe intoxication, bleeding, blood clotting disorders, decreased immunity, inflammatory processes with poor tissue regeneration, poisoning, including toxic substances. If the hemoglobin level in the blood drops below 65 g/l, this is considered a severe stage and an indication for blood transfusion (blood transfusion).
Important! If blood loss exceeds 1 liter during childbirth, a blood transfusion is also performed.
Reasons for hemoglobin falling below 65g/l:
- large loss of blood due to injuries, during operations, during childbirth, bleeding in gynecology and for other reasons;
- oncology;
- infectious diseases of a chronic type in different organs;
- hematological diseases in which red blood cells are quickly destroyed;
- predisposition associated with genetics.
How long does the effect last after a blood transfusion?
Everyone knows that blood transfusion is a medical procedure that saves the life of many patients in extreme and difficult situations and prolongs it for cancer patients. But the blood transfusion system is not at all simple. At the first stage, 250-300 ml of red blood cells are administered and the vital signs of the body are monitored. If red blood cells and hemoglobin have returned to normal, the next blood transfusion is carried out no earlier than 18-30 days later, provided that the red blood cell has not recovered during this period of time.
In a situation where, due to the constant destruction of pathological tissues of the neoplasm, daily blood loss occurs, transfusion is performed in the amount of 2-3 doses of red blood cells every 5-7 days. This situation is typical for cervical or vaginal cancer. The procedure will be repeated until conditions are created that are suitable for embolization of the vessels feeding the tumor, or for surgical treatment or chemotherapy.
Consequences of blood transfusion to raise hemoglobin
The main positive side of the procedure is the patient’s rapid recovery from intoxication, recovery from anemia and poisoning, and an increase in hemoglobin levels. The negative consequences of transfusion are the possible occurrence of complications. It is very difficult to foresee all complications during transfusion, because Each person’s body can react completely unpredictably to blood transfusion. Conventionally, possible complications are usually divided into three groups: mechanical, reactive conditions and complications associated with infectious diseases.
Mechanical complications include:
- improper too rapid introduction of foreign media into the body, causing expansion of the heart;
- entry of air particles into the blood transfusion system, causing embolism;
- blockage of blood vessels due to blood clots entering them;
- improper functioning of organs as a result of a blood clot entering them.
Reactive consequences of blood transfusion:
- hemolytic types of shock can occur if blood is used that is poorly compatible with antigens;
- post-transfusion shock condition caused by poor quality donor material, i.e. with toxins, microorganisms, destroyed cells, etc.;
- anaphylactic shock as a result of the development of allergic reactions;
- citrate shock when using blood with preservatives;
- increase in body temperature after blood transfusion.
How are donors' blood tested?
For oncology, you can do a blood transfusion that has undergone a thorough examination for infections, group membership, and Rh factor. If necessary, additional testing is carried out for other group antigens. To completely protect patients from infections, the following measures are taken:
- Before donating blood, the donor answers a questionnaire. He is obliged to talk about possible cases of infection recently. If there is the slightest suspicion of infection in a donor, he is not allowed to donate;
- the donor is examined by doctors and undergoes tests. People who have abnormal test results (abnormal bilirubin, increased white blood cells, high liver enzymes, etc.) are excluded from taking the test;
- After collection, the blood is examined for parenteral infections. If they are absent, she is divided into factions and sent to a six-month quarantine to check the donor again. He could have had infections that were not detected by laboratory methods because they were at an early stage of development.