This information explains what to expect before, during, and after your blood transfusion procedure. A blood transfusion is a procedure in which blood or blood cells are given into your body. You may need a blood transfusion if cancer or cancer treatment affects your blood in any way.
Some people may not want to have a blood transfusion for religious or other reasons. You always have the right to refuse treatment. Your healthcare provider may only recommend a blood transfusion if they think it is necessary. You may lose a lot of blood during some operations. If you don't replace this blood, you could die.
to come back to the beginning
About blood
Blood consists of plasma, red blood cells (erythrocytes), platelets and white blood cells (leukocytes).
- Plasma is the liquid part of blood. It contains all blood cells. You may need a plasma transfusion if your blood doesn't clot well.
- Red blood cells carry oxygen throughout the body. You may need a red blood cell transfusion if you have low red blood cell counts (anemia). This may help relieve dizziness, shortness of breath, or weakness (feeling unusually tired or tired).
- Platelets help form clots and stop bleeding. You may need a platelet transfusion if you have low platelet counts (thrombocytopenia). This may help stop bleeding or prevent too much bleeding during surgery or a procedure.
- White blood cells fight infections. White blood cell transfusion is a rare procedure that is performed in exceptional situations.
to come back to the beginning
What blood products are used for blood transfusion?
Donor blood in its pure form is rarely transfused, only in military field conditions. The most commonly used blood components, as well as preparations prepared from them:
- erythrocyte mass, as well as erythrocyte suspension, “washed” erythrocytes;
- platelet mass;
- leukocyte mass, leukocyte suspension;
- plasma immunoglobulin preparations
The first two types are usually used for massive bleeding, as well as for chronic anemia, and for tumors with extensive tissue destruction.
Donor leukocytes help fight immunodeficiency conditions, in which the risk of very severe concomitant infection is extremely high. Leukocyte mass is currently used quite rarely.
Plasma is used for the prevention and treatment of the consequences of massive bleeding such as disseminated intravascular coagulation syndrome, as well as in the complex treatment of blood clotting disorders.
Immunoglobulin preparations are used for primary immunodeficiencies, such as HIV, and for secondary ones against the background of long-term chemotherapy with inhibition of the hematopoietic function of the bone marrow.
In addition, blood transfusions are part of the patient's active preparation for major surgical interventions, carried out in order to reduce the risks of severe complications during surgery.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
About donated blood
There are currently no substitutes for blood. The blood or blood cells you receive during a transfusion are usually donated by someone else.
Sometimes you can donate your own blood, which can be stored and given to you if necessary. This is called autodonation. For more information, check out How to Become Your Own Blood Donor.
After donating blood, it is checked to determine whether it belongs to a certain group. It is also checked for:
- syphilis;
- hepatitis B and C;
- HIV;
- a virus associated with a very rare type of leukemia;
- West Nile virus;
- Trypanosome cruzi (the parasite that causes Chagas disease);
- Zika virus;
- bacteria (platelet only).
If the test results reveal any of these infections, the blood is discarded.
Targeted donation
Purposeful donation means someone donates blood or blood cells specifically for you. Blood received as part of a targeted donation is tested in the same ways as any other. If any of the viruses listed above are detected in the blood, the donor will be notified privately.
Red blood cells donated as part of a targeted donation are stored for 25 days. Platelets donated as part of a targeted donation are stored for 4 days. After this period has expired, they can be given to someone else. The blood will also be given to someone else if the donor's blood type does not match yours.
to come back to the beginning
Features of the blood transfusion procedure at the International Clinic Medica24 for cancer patients?
The lion's share of our patients are patients with cancer who receive multiple chemotherapy treatments and, in most cases, have undergone multiple operations, so for them there is a special procedure for routine blood transfusion. We do not allow violations of this order.
To avoid the risks of hemolysis or intravascular coagulation, we make sure to individually select the dose of erythromass and platelet concentrate using gel tests in a blood bank. To do this, the patient comes to us the day before, 1-2 days in advance, and we do rapid blood tests in the presence of the patient.
The results of rapid tests make it possible to clarify the presence or absence of indications for blood transfusion and a preliminary assessment of the required number of doses of drugs. In addition, after collecting blood from the patient, and having received an advance payment for blood products, we send blood samples for gel tests, as well as for checking hemostasis (clotting system) indicators of the blood, and infectious safety (tests for syphilis, HIV, hepatitis).
Upon receipt of individually selected blood products, within 3-24 hours from the moment of receiving the results of rapid tests, we conduct a test for the biological compatibility of each individual blood product and each individual dose with the patient’s blood. Tests are carried out both in vitro (in a special plate) and by administering a small, usually 2-5 ml, microdose of blood to the patient. In the absence of a pyretic or allergic reaction, we administer the first dose. Subsequent doses of blood are administered at intervals, from 20 to 40 minutes, to avoid complications.
After completing the blood transfusion procedure, we take blood for a control examination in order to assess the effectiveness of blood transfusion and blood components. The patient must be examined by a hemotransfusiologist before, during and after blood transfusion. All observation data are entered into the blood transfusion card.
Another secret of our clinic when transfusing blood to cancer patients is the active use of steroid hormones to “cover up” possible side effects of blood transfusion, as well as the use of colony-stimulating factors - drugs that help the body produce red and white blood cells on its own.
Before blood transfusion
Before the transfusion procedure, we will determine your blood type using a test called blood type and Rh factor. It may take 2 to 4 hours for the blood bank to process the test. If you have unexpected indicators, it may take longer. Based on the results of your blood type and Rh factor test, your health care provider can make sure that the blood or blood cells received during the transfusion are safe for you.
Your healthcare provider will also discuss the risks of blood transfusions with you. The likelihood of an allergic reaction during or after the transfusion procedure is very low. The most common adverse reactions include fever of 100.4°F (38°C), chills, and rash. They can be eliminated with medication. Reactions to blood transfusions are rarely life-threatening.
to come back to the beginning
Shamray Vladimir Stepanovich
Doctor of the highest qualification category, head of the hematology department.
More details / Reviews

BLOOD TRANSFUSION IN SURGERY. PRACTICAL GUIDE. B.V.PETROVSKY. PRACTITIONER'S LIBRARY. MEDGIZ. 1954
Errors in determining blood groups, incorrect technique, non-compliance with blood conservation rules, underestimation of contraindications for transfusion - all these errors can cause a number of post-transfusion complications.
Statistics on complications observed after blood transfusion are not usually reported in the press, but mortality associated with blood transfusions has been published in a number of countries.
This decrease in fatal post-transfusion complications in the USSR is explained by the progress in the organization of blood transfusion, the improvement of preservation techniques, and the improvement of the general qualifications of doctors and nurses.
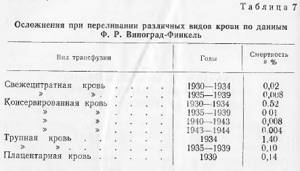
Interesting data on the percentage of fatal post-transfusion complications observed during transfusion of freshly citrated, canned, cadaveric and placental blood.
Below is a table by F.R. Winograd-Finkel about complications during transfusion of various types of blood (Table 7).
DANGERS AND COMPLICATIONS DURING BLOOD TRANSFUSION. POST-TRANSFUSION REACTIONS
Table 7
This table indicates an increased percentage of complications after transfusions of cadaveric and placental blood, which is partly explained by the complexity of organizing transfusions of this type of blood. The safest method is a canned blood transfusion.
However, some complications still occur with this method. Knowledge of their causes, clinical picture and outcomes, methods of prevention and treatment is absolutely necessary for every practicing physician.
The classification of post-transfusion complications can be presented as follows:
1) blood transfusion shock associated with transfusion of incompatible blood;
2) post-transfusion shock due to transfusion of group-compatible blood;
3) complications as a result of errors in blood transfusion techniques;
4) transmission of infection along with the donor’s blood.
Post-transfusion reactions should be classified as a special group and should be considered as complications only in selected severe cases.
Then they are included in the second group.
Hemotransfusion shock as a consequence of transfusion of group-incompatible blood is a serious and very dangerous complication.
Currently, thanks to the proper organization of blood transfusion, the risk of transfusion shock has been almost completely eliminated. However, when deviating from the rules for determining blood compatibility, which can occur especially in institutions where blood transfusions are rarely performed, such disasters are still observed. According to the severity of clinical symptoms, transfusion shock can be severe, moderate or mild.
The severity of transfusion shock depends on a number of reasons, of which the amount of incompatible blood transfused and the speed of its administration seem to be of decisive importance. For example, amounts of foreign blood not exceeding 20-30 ml may not produce any special consequences other than severe chills and fever. However, these doses of incompatible blood can be fatal if the liver or kidneys are damaged (A. N. Filatov).
Indications for blood transfusion, as well as the transfusion technique, play a role in the development of transfusion shock. For example, it is known that transfusion of incompatible blood during an operation performed under deep anesthesia may initially not cause symptoms of incompatibility and only later manifests itself as signs of dysfunction kidneys and other parenchymal organs. This was shown experimentally by V.P. Berezkin and T. Zaltsman in the laboratory headed by V.S. Galkin. Experiments with the transfusion of foreign blood into dogs under anesthesia (intravenous administration of 2-5% novocaine solution), performed by I. I. Fedorov, also showed the absence of the animals’ reaction to the administration of large doses of heterogeneous blood.
N.I. Blinov (1949) cites his observation of the erroneous transfusion of 300 ml of blood of a different group to a patient who was under pentothal anesthesia.
Transfusion was performed during surgery. The patient, who had blood of group 0 (I), was injected with blood of group A (II). There was no reaction to this transfusion. Soon after the error was determined, the patient was transfused with 300 ml of group 0(1) blood and 300 ml of anti-shock fluid containing 10% alcohol. During the second transfusion, the patient's face became covered with red spots and he woke up. He did not make any complaints, but within 24 hours hemoglobinuria and the presence of protein in the urine were noted.
We observed a similar case in 1943, when 200 ml of incompatible blood administered during hip amputation under anesthesia did not have any negative effect on the patient. After the operation, the presence of protein in the urine was noted for 3 days. The patient, in good condition, was evacuated to the rear 2 weeks later.
In another patient whom we consulted, after a transfusion of 250 ml of incompatible blood under anesthesia, a severe reaction was observed, resulting in severe signs of transfusion shock.
Thus, based on clinical and experimental observations, we can conclude that anesthesia, by causing inhibition processes in the cerebral cortex and sharply reducing the reflex activity of the body, prevents the manifestation of signs of transfusion shock. However, this is observed only with very deep anesthesia (I.I. Fedorov) and, in addition, despite the absence of reflex manifestations of shock, after transfusions of incompatible blood under anesthesia, severe intoxication, hemoglobinuria, damage to parenchymal organs develops, i.e. a severe picture of protein shock (N.I. Blinov).
The slow, drip rate of transfusion of foreign, incompatible blood also slows down the development of transfusion shock and significantly reduces the severity of its symptoms.
Thus, according to N.I. Blinov (1952), after the rapid administration of blood of a different group, symptoms of a clinical hemolytic reaction appear in the recipient within 2-3 minutes.
The same conclusions follow from the works of N. I. Blinov (1943) and I. R. Petrov (1951), which indicate that the clinical picture of transfusion shock manifests itself in cases where blood of a different group is administered at a rate of 2-3 ml per minute. Slow transfusion of incompatible blood does not cause a clinically significant reaction. However, as soon as the rate of administration of this blood increases to 2-3 ml per minute, dizziness, difficulty breathing and other symptoms of a hemolytic reaction appear. They stop again 2-3 minutes after stopping the infusion.
All these facts largely confirm the main role of neuro-reflex mechanisms in the development of transfusion shock. This is also evidenced by clinical observations of blood transfusion shock and the effects of therapeutic measures against it.
Transfusion shock is now extremely rare;
anyone who has seen the clinical manifestations of severe post-transfusion shock will never forget its terrible symptoms. Usually, after the administration of 30-50 ml of blood of a different group, a number of subjective and objective symptoms are immediately noted. The patient feels awkwardness in the lumbar region, tightness in the chest, and ringing in the ears. Headaches, abdominal pain and, most importantly, rapidly increasing pain in the lower back appear. These pains can be extremely intense - the patient screams and sometimes loses consciousness.
Objectively, one can first register sharp redness and then pallor of the face, cyanosis of the lips, acrocyanosis, shortness of breath, anxiety of the patient, increased heart rate to 100-120 or more beats per minute, as well as a decrease in maximum blood pressure to 70-80 mm. Some authors (A.N. Filatov) attach great importance to this particular sign, which appears at the very beginning of the introduction of incompatible blood.
In case of severe shock, soon after the transfusion, after 20-30 minutes, and sometimes during the transfusion, the patient loses consciousness, involuntary defecation and urination appear.
In rare cases of fulminant forms of shock, death can occur 10-20 minutes after transfusion. More often than not, the pain subsides, consciousness returns, cardiac activity improves, and blood pressure slightly increases. In this second period of shock, there is an increase in temperature to 40° and above, leukopenia, followed by leukocytosis, hemoglobinemia (intravascular hemolysis), and jaundice appears (not always). Characteristic of this period of shock is progressive impairment of renal function. Oliguria quickly gives way to anuria and then, if measures are not taken in a timely manner, the patient dies within 1-2 days with symptoms of uremia,
The second period of shock in these cases is characterized by slowly onset oliguria, with pronounced changes in urine (increased specific gravity, the presence of protein, red blood cells, casts).
Jaundice is mild and sometimes absent. If active treatment is not carried out, the state of renal function and parenchymal organs gradually worsens, oliguria progresses, and after 3-5 days the patient dies due to symptoms of uremia. Some of the patients, despite pronounced signs of hemolytic shock, endure this severe complication.
In this case, the patient received only 100 ml of incompatible blood, which, apparently, determined the favorable outcome of this serious complication.
The mild degree of post-transfusion shock differs from the first two degrees in its slower course and relatively late onset of symptoms.
For example, the following case history can be given.
Patient K. was operated on in one of the Budapest hospitals in November 1950. A caesarean section was performed under ether anesthesia. At the end of the operation, 300 ml of blood of group AB (IV) was transfused. The patient tolerated the operation well. The next day after surgery, the temperature increased to 38 C, and vomiting was noted. 3 days after the operation, oliguria appeared (500 ml of urine, protein in the urine, casts).
A day later, the amount of urine decreased to 200 ml per day, symptoms of uremia appeared, and residual blood nitrogen sharply increased. On the 6th day after surgery, the patient was prescribed treatment: (massive drip infusion of isotonic glucose solution, bilateral repeated lumbar novocaine blockade according to Bishnevsky). The amount of urine gradually began to increase, the symptoms of uremia disappeared and the patient recovered.
A similar mild picture of transfusion shock
or rather post-transfusion uremia, because there was no shock as such (probably due to anesthesia), it occurs relatively rarely before other forms of complications. However, even in these cases (if a blood transfusion is not performed during anesthesia), it is still possible to note the first signs of a catastrophe, which are registered as an unusually strong reaction causing chills, awkwardness or pain in the lumbar region, fever, tachycardia. Subsequently, renal dysfunction is observed, expressed to a greater or lesser extent, as well as associated uremic phenomena. Sometimes such degrees of shock can go unnoticed, as there are reports in the press.
Everything that has been said about transfusion shock after the introduction of incompatible blood indicates that its cause is usually a medical error in determining the blood group and in the transfusion technique.
A A Bagdasarov and M. S. Dultsin (1952) note that in some patients with diseases of the hematopoietic organs, incompatibility of their plasma with red blood cells of the same blood group of the donor is sometimes detected. In such cases, it can be difficult to separate false agglutination from true one, and therefore such patients need to be injected with the blood of a universal donor by drip or replace the blood transfusion with plasma or serum.
The question of the presence of “individual incompatibility of plasma proteins of the donor and recipient”
to which A, A, Bogomolets attached great importance, is currently being resolved negatively. Most complications during blood transfusion do not depend on the hypothetical “individual protein incompatibility”, but on real reasons: incompatibility of blood groups, the production of antibodies when reintroducing Rh-positive red blood cells from a donor to a recipient with Rh-negative blood, transfusion of poor-quality, infected blood, etc.
Thus, at present, the possibility of so-called reverse agglutination by donor serum of recipient erythrocytes is practically denied.
Recent works by domestic and foreign scientists confirm the importance of the Rh factor in the origin of post-transfusion complications.
Repeated repeated injections of Rh-positive red blood cells into patients with Rh-negative blood sometimes lead to the formation of Rh antibodies in the recipient's blood, which can cause agglutination of the transfused Rh-positive red blood cells. The production of antibodies in the recipient's body occurs slowly and does not depend on the dosage of the transfusion. Long periods of time between transfusions increase the phenomena of sensitization.
Many severe reactions have been described in modern literature,
associated with repeated transfusion of Rh-incompatible blood. They resemble hemotransfusion shock caused by the introduction of a foreign blood group, but differ from it in the late manifestation and erasure of symptoms. Thus, according to F.R. Vinograd-Finkel, out of 10 severe reactions of this type, shock was recorded in only 4 patients. Symptoms of incompatibility in these cases usually do not occur immediately, but after 30-40 minutes, sometimes after 2-3 hours and even 12 hours after transfusion.
In women with Rh-negative blood, pregnancy with an Rh-positive fetus can also lead to the formation of antibodies. Transfusion of Rh-positive blood to such a woman sometimes causes transfusion shock.
Potter published (1944) comprehensive statistics of complications after the introduction of Rh-incompatible blood. Of the 71 cases of severe reactions, 60 were female recipients and only 11 were male recipients. 10 patients died from blood transfusion shock.
Currently, prevention of transfusion shock should consist of the following.
First of all, it is necessary that every doctor perfectly knows all the details of determining blood groups and blood transfusion techniques, and personally determines (twice using two series of standard sera) the blood group of the donor and recipient, even when transfusing canned blood. In this case, it is necessary to strictly follow the rules for determining blood compatibility: a) the method for determining blood groups with three standard sera, with the addition of saline, b) an individual compatibility test and c) a triple oiological test.
It must be emphasized that the individual compatibility test and the biological test are control measures. The biological triple sample is especially reliable in this sense. To illustrate its meaning, consider the following example.
In April 1950, patient B. underwent a transfusion of A (II) blood group of the same name in order to prepare him for surgery for a stomach tumor. The first 2 portions of blood, 20 ml each, did not cause any consequences. After the third portion of blood (another 20 ml), chills, shortness of breath, slight cyanosis, and a feeling of tightness in the chest appeared. The transfusion was stopped, and the blood groups of the donor and recipient were checked. It turned out that the doctor who determined the blood group made a mistake and mistook pseudoagglutination for true.
At the first sign of an unusual reaction occurring during or after a biological test, the blood transfusion should be interrupted and the blood type of the donor and recipient should be checked again.
In order to be able to identify an error, it is always necessary to leave and store several milliliters of transfused blood in the glacier during the day.
To prevent complications associated with transfusion of Rh-incompatible blood, it is recommended that all patients carefully collect information about their previous blood transfusions and how these transfusions proceeded. If there is a history of reactions and complications associated with blood transfusion, the Rh factor in the recipient’s blood should be determined and the Rh-negative patient should be given only Rh-negative blood.
Particular care should be taken when transfusing blood to women who have given birth and who have a history of sensitization to the Rh factor.
In order to eliminate complications that depend on transfusions of Rh-negative blood, it is necessary to have Rh-negative preserved blood in the glacier where the blood supply is stored. If this is not available, plasma or serum from any donor can be used for transfusion.
If blood incompatibility is established soon after transfusion, it is necessary to take emergency vigorous measures, which were developed in the USSR by A. N. Filatov and A. V. Vishnevsky.
First of all, you should immediately perform a venipuncture and remove 300-400 ml of the patient’s blood while simultaneously transfusing him, preferably with fresh or freshly preserved blood of the same group in the same quantity (A. N. Filatov’s method). It should be taken into account that venipuncture may be unsuccessful due to the collapse of the veins and increased blood clotting. In these cases, it is recommended to quickly perform a venesection.
Now, after this event, it is necessary to perform a bilateral perirenal novocaine blockade according to Vishnevsky.
The patient is turned on his side. After skin anesthesia, a long needle is inserted perpendicularly into the area of the angle formed by the XII rib and the long back muscles, which is advanced 5-6 cm to the perinephric tissue. As the needle advances, a solution of novocaine is constantly injected through it. The correct position of the needle end is achieved if novocaine flows out of it (the solution is distributed in the loose perirenal tissue). In this way, 100 ml of 0.25% novocaine solution is injected into the right and left perinephric areas (Fig. 74).
In addition, the patient is prescribed intravenous drip infusions of 4.5% glucose solution in the amount of 2-2.5 liters per day, as well as injections of morphine, camphor, and atropine.
In case of late detection of blood incompatibility after transfusion (on the second or more days), bloodletting in the amount of 200 ml should be performed, but instead of whole blood it is better to administer serum or plasma (200-300 ml). Novocaine lumbar blockade is fully indicated here. A careful drip infusion of glucose (1.5 liters per day) is also recommended.
Usually all these measures are effective. Before this technique, developed by Soviet authors, post-transfusion shock, according to world literature, ended fatally in 50-60% of patients. Currently, there are rare cases of shock that are still observed
Recently, domestic surgeons and pathophysiologists have been elucidating the positive qualities of intravenous infusion of novocaine solution for these complications.
In late cases, especially in weakened patients with impaired liver and kidney function, the prognosis may be unfavorable.
Post-transfusion shock due to compatibility of donor and recipient blood groups has been the subject of discussion at a number of conferences and congresses. A. A. Bogomolets put forward the original theory of colloidoclatic shock, according to which protein incompatibility between the plasma of the donor and the recipient exists with every transfusion. Each transfusion of blood that is completely compatible in group terms is always accompanied by colloidoclasia. However, colloidoclasis shock, as already mentioned, rarely occurs - only in cases of significantly pronounced colloidoclasia, accompanied by sudden changes in the blood and vital organs (A. A. Bogomolets).
The opinion of A. N. Filatov that the so-called protein incompatibility of blood practically occurs only in the presence of a number of changes in the transfused blood (infection, overheating, denaturation) is correct. Only this point of view equips the doctor with the necessary information about the clinical picture of post-transfusion shock, its prevention and treatment.
The causes of post-transfusion shock in the presence of compatibility of the blood groups of the donor and recipient are most often associated with infection of the preserved blood. This type of shock does not usually occur with freshly citrated blood transfusions or direct transfusions. An inexperienced doctor may make a mistake when determining the suitability of canned blood, and this is most often the cause of the disaster (A. N. Filatov).
A. N. Filatov was able to prove the growth of non-pathogenic microbes during a bacteriological study of crops,
taken from the remainder of the transfused blood and from the blood of a patient who developed post-transfusion shock. The second reason for this type of shock may be overheating of the blood (above 40°) or reheating of canned or freshly citrated blood—even within the limits of 38°, determined by the instructions. The destruction of the protein fraction of the blood in these cases is always pronounced, which causes a strong reaction or even shock.
The third cause of post-transfusion shock may be a change in blood plasma as a result of insufficient stabilization or due to improper blood collection, which promotes blood clotting (I. R. Petrov and G. Kasumov).
Thus, it should be emphasized that all these factors, especially infection, dramatically impair the quality of blood and lead to severe reactions and complications.
Having thousands of observations of the effect of transfused blood, we could be convinced that the extensive experience of blood transfusion of the team of a medical institution leads to a sharp reduction in the number of reactions and timely elimination of post-transfusion complications.
The clinical symptoms of post-transfusion shock of this type differ in some features. When transfused with infected, low-quality blood, shock is even more severe than with incompatibility of blood groups. Usually, the first symptoms do not appear immediately after the transfusion, but after 20-30 minutes or later, although in some cases they can be noted during a triple biological test. The first sign of shock is severe chills, pronounced cyanosis, tachycardia with a drop in blood pressure and an increase in temperature to 40-41°. Loss of vision is often noted. The patient usually loses consciousness, rushes about, vomits, and involuntary separation of urine and feces is noted. Pain in the lumbar region in these patients is less common than in transfusion shock after the administration of incompatible blood.
Most often, severe symptoms of intoxication, anuria and uremia lead to the death of these patients in a short time (after 10-20 hours).
Less commonly observed is the torpid course of protein shock. The condition of the cardiovascular system improves, consciousness returns, the temperature decreases somewhat, and the patient calms down. However, the next day the temperature rises again to 40°, which is accompanied by tremendous chills. The patient is in a serious, as if septic condition, the color of the skin becomes gray-yellow, the amount of urine sharply decreases, the number of leukocytes increases to 30,000-40,000, the leukocyte formula acquires a sharp shift to the left, young forms of leukocytes appear, their toxic granularity. Gradually, if no decisive measures are taken, anuria and uremia sets in, from which the patient usually dies within 2-5 days.
When transfusing blood that is not infected, but denatured by overheating and other factors, all of these symptoms are less pronounced.
Measures to prevent post-transfusion shock are described in the chapters on transfusion techniques. First of all, “these include the strictest adherence to the rules for collecting and preserving blood, as well as storing preserved blood and its transportation. Each transfusion physician should then pay particular attention to the signs of suitability of the preserved blood when collecting it before transfusion. The doctor himself must personally examine the blood before transfusion and, if there is the slightest doubt, consult with the senior surgeon whether to postpone the transfusion and not transfuse doubtful blood.
Under no circumstances should reheating of blood be allowed, and in general, blood that was taken out of the glacier and kept in a warm room for many hours will not be suitable for transfusion. The expiration dates of canned blood should be strictly adhered to, especially in institutions where there is not much experience in transfusion of this type of blood.
You need to be careful when handling blood that contains a large number of clots.
A small amount of clots does not prevent transfusion (after filtering the blood), but this blood should be transfused slowly, carefully monitoring the patient's response.
Finally, it should be emphasized the harm of diluting the blood with various liquids, which should be avoided due to the danger of hemolysis.
If the first symptoms of post-transfusion shock are present, after determining the blood groups of the donor and recipient and establishing their compatibility, it is necessary to immediately take a culture from the blood of the donor and recipient, as well as carry out general clinical studies of the patient.
Urgent measures in these cases are: bloodletting (200-300 ml of blood), drip intravenous infusion of isotonic glucose solution (2.5-3 liters per day), novocaine lumbar blockade according to Vishnevsky and massive injection of penicillin (up to 1,000,000 units intramuscularly per day). day).
In the future, depending on the development of clinical symptoms, antibiotics, diet, and restorative measures are prescribed.
Recently, intravenous and intra-arterial administration of novocaine has been widely used in clinical and experimental surgery.
Based on the data obtained by many authors when introducing novocaine into the venous bed (V.S. Galkin, M.A. Bubnov, I.R. Petrov, etc.), it can be assumed that novocaine injected into a vein temporarily reduces or even turns off the reflex excitability of the vascular wall. This method can be used in the future for the prevention and treatment of post-transfusion shock.
The prognosis of post-transfusion shock due to transfusion of compatible blood, untimeliness and low activity of therapeutic measures is usually poor. Using active treatment, it is possible to save the lives of the most severe, seemingly hopeless patients.
Allergic reactions due to blood transfusions are relatively rare. They are observed not only after repeated transfusions, but also after the first transfusion as a result of sensitization by various proteins (A. A. Bogomolets). Apparently, the state of the patient’s nervous system before the transfusion, the donor’s diet (Stuart), the administration of various serums to the patient, which was not clear from the anamnesis, etc., play a role.
Several cases of death due to post-transfusion anaphylactic shock were published in the literature before 1940. Observations by Soviet authors do not indicate a particular danger of post-transfusion anaphylaxis.
Typically, an anaphylactic reaction after a blood transfusion is expressed in severe chills, an increase in temperature to 38-39°, an allergic rash on the skin (urticaria), itching and a feeling of general malaise. On the blood side, leukocytosis (10,000–12,000) and an increased number of eosinophils (5–8) are noted.
During a blood transfusion
When everything is ready, the nurse will have access to one of your veins.
- If you have a central venous catheter (CVC), such as a tunneled chest catheter or a peripherally inserted central catheter (PICC), your nurse uses it to give the blood transfusion. This is a painless procedure.
- If you have an implantable port, such as a MediPort®, your nurse will use it to give blood transfusions. In this case, the same type of needle used for chemotherapy will be used.
- If an implanted port or CVC is not in place, the nurse will place an IV in one of the veins.
After gaining access to your vein, the nurse will begin the transfusion. This procedure is painless.
The procedure for transfusion of one dose of red blood cells usually takes 2-4 hours. The transfusion procedure for one dose of platelets takes 30–60 minutes. Your nurse will monitor you closely throughout the blood transfusion procedure.
to come back to the beginning
When should you contact your healthcare provider?
Call your healthcare provider if you have:
- temperature 100.4°F (38°C) or higher;
- chills;
- redness of the face and a feeling that the face is “burning”;
- rash or severe itching;
- difficulty breathing or shortness of breath;
- lower back pain;
- nausea (feeling of vomiting) or vomiting;
- weakness or faintness;
- dark colored urine.
If you have chest pain, call 911 right away.
Return to top