Hemoglobin is a protein that contains iron and carries oxygen from the lungs to the organs. A pathology in which the hemoglobin level falls below normal is called anemia
Anemia is accompanied by weakness, headaches, tinnitus, decreased appetite and sleep disturbances. The most vulnerable category of patients with anemia are children of early and school age. Schoolchildren get tired quickly, learn more slowly and remember less information, do not get enough sleep and become irritable. With severe anemia, dystrophic changes occur in the heart muscle - this leads to disruption of the heart and circulatory failure.
Hemoglobin levels can be raised with medications and foods. However, the choice of treatment depends on the type of anemia and its cause. In this article we will answer the questions: what is the norm for hemoglobin in children, why does it decrease, what foods does it contain, and how to prevent anemia in children.
Hemoglobin - what is the norm for a child
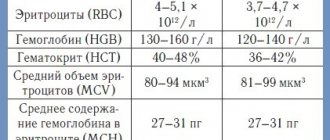
Each blood indicator has a norm, including hemoglobin. The World Health Organization gives the following hemoglobin standards for children:
- newborns up to 2 weeks of life - not lower than 150 g/l;
- children from 2 to 4 weeks of life - 120 g/l and above;
- children aged 6 to 59 months - 110-140 g/l;
- children aged 5 to 11 years - 115-140 g/l;
- children aged 12 to 14 years - 120-150 g/l;
- children and adults over 15 years old - 130-160 g/l.
Anything below is considered mild (below normal, but above 90 g/l), moderate (70-90 g/l) or severe (below 70 g/l) anemia. Each of the three degrees of severity has its own symptoms and treatment tactics.
How to increase hemoglobin in a baby who has already been introduced to complementary foods
If the child has already been introduced to complete complementary feeding (preferably no earlier than six months), then hemoglobin can be increased by adding the iron-containing products listed above to his diet. If your baby is introduced to complementary foods before six months, the absorption of iron from breast milk will become worse. It has also been noted that anemia is common in children who are fed cow's and goat's milk. This is due to the fact that these products do not contain enough microelements necessary for hematopoiesis. In addition, the baby’s body is often unable to break down cow protein.
Be sure to include berries in your child’s diet (even frozen or dried, if it’s winter): blueberries, strawberries, black currants, cranberries.
Why does a child have low hemoglobin?
Reasons for decreased hemoglobin levels in children: blood loss, insufficient blood production in the bone marrow and increased destruction of red blood cells.
Causes of low hemoglobin levels:
- malignant (cancerous) tumors;
- anemia due to vitamin deficiency;
- Iron-deficiency anemia;
- aplastic anemia;
- cirrhosis of the liver;
- Hodgkin's lymphoma;
- hypothyroidism;
- chronic kidney disease.
The first reason is blood loss. It can be acute and chronic. Typically, hemoglobin levels decrease several hours after the onset of blood loss. Chronic blood loss leads to anemia when the body does not have enough iron to produce new red blood cells. Examples of blood loss: gastrointestinal bleeding from an ulcer, bowel or kidney cancer, bone fractures, recent surgery, heavy menstruation in teenage girls.
The second reason is low blood production (erythropoiesis deficiency). In this case, a decrease in hemoglobin levels is caused by infections, hereditary pathologies, kidney diseases, copper and folic acid deficiency, vitamin B1 deficiency and malabsorption.
In addition, insufficiency of erythropoiesis occurs in myelofibrosis and osteomyelosclerosis. Myelofibrosis is a pathology in which fibrous tissue gradually replaces hematopoietic tissue in the bone marrow. Osteomyelosclerosis is the replacement of connective tissue with hematopoietic tissue. These disorders usually occur in cancers: lymphoma, multiple myeloma, chronic myelogenous leukemia.
The third reason is increased destruction of red blood cells. Occurs with pathological enlargement of the spleen, taking certain medications (quinine, quinidine, penicillin, ticlopidine), hemolytic-uremic syndrome, Epstein-Barr viral infection (human herpes virus type 4), malaria, botulism, tetanus, congenital heart valve defects, spider bites , insufficient levels of phosphates in the blood.
Other reasons for low hemoglobin levels in the blood:
- inflammatory diseases of the small and large intestine;
- insufficient intake of iron into the child’s body;
- chronic kidney disease;
- prematurity of the child;
- late or early umbilical cord ligation;
- Giardiasis is a parasitic intestinal disease;
- Helicobacter pylori infection and atrophic gastritis.
There are groups and risk factors that can lead to low hemoglobin levels and the most common type of anemia, iron deficiency:
- if the child was born with low body weight;
- children born from multiple pregnancies;
- children who did not receive enough iron through breastfeeding and formula milk;
- children who often suffer from infectious diseases;
- children with allergies;
- malnutrition, poverty.
A decrease in hemoglobin levels is not always regarded as a pathology. Children, especially teenagers, need a lot of iron for their body development. Due to the rapid growth of the microelement, there may be a temporary lack of microelement, so the level of hemoglobin in the blood decreases. This is especially true for children and adolescents who are actively involved in sports. They may develop "athlete's anemia." By eating foods high in iron, the deficiency is eliminated.
Correction of iron deficiency in children
The goal of therapy for iron deficiency anemia (IDA) is to eliminate iron deficiency and restore its reserves in the body. This can only be achieved by eliminating the cause underlying IDA in the body.
The basic principles of treatment of IDA were formulated by L. I. Idelson in 1981:
- It is impossible to compensate for iron deficiency without medicinal iron-containing drugs.
- IDA therapy should be carried out primarily with oral iron preparations.
- IDA therapy should not be stopped after normalization of hemoglobin levels.
- Blood transfusions for IDA should be carried out only strictly for health reasons.
Previously, it was believed that iron deficiency could be eliminated by prescribing a diet containing apples, buckwheat, pomegranates and other plant foods containing iron. However, in the 60s. 20th century researchers have proven that iron contained in foods in the form of heme (meat, liver, fish) is better absorbed in the body than from other compounds. About 90% of iron is absorbed in the duodenum, the rest in the upper jejunum. In iron deficiency conditions, the absorption surface of the small intestine increases. Iron is absorbed in 2 forms:
- heme (10%), the sources of which are hemoglobin and myoglobin, which are part of products of animal origin (meat, fish, poultry, liver) (Table 1);
- non-heme (90%), the sources of which are products of plant origin (vegetables, fruits, cereals) (Table 2).
The amount of iron received during the day from food contains about 10–12 mg of iron (heme + non-heme), but only 1–1.2 mg of this trace element is absorbed. It has been established that the bioavailability of heme iron in food products is higher than that of non-heme compounds and amounts to 25–30%.
Most dietary iron is in the non-heme form. The bioavailability of iron from cereals, legumes, tubers, vegetables and fruits is significantly lower than from heme compounds, and largely depends on the predominance of factors in the diet that inhibit or potentiate intestinal ferroabsorption (Table 3).
Despite the high iron content in some products of plant origin, they are not able to provide the child’s body with it. Substances present in food products of plant origin (tannins, phytins, phosphates) form insoluble compounds with Fe (III) and are excreted in feces. There is also information about the adverse effect of dietary fiber, which is rich in cereals, fresh vegetables, and fruits, on the absorption of iron. In the intestines, dietary fiber is practically not digested; iron is fixed on their surface and excreted in feces. On the contrary, ascorbic acid and animal protein (meat, fish) increase the bioavailability of iron, which increase the absorption of the microelement. It should also be noted that products made from meat, liver, and fish, in turn, increase the absorption of iron from vegetables and fruits when used simultaneously.
A diet that is complete and balanced in terms of its main ingredients can only “cover” the body’s physiological need for iron, but does not eliminate its deficiency.
The natural prevention of IDA in children in the first months of life is exclusive breastfeeding for up to 4–6 months. It is known that the concentration of iron in human milk is only 0.2–0.4 mg/l, but the absorption of iron from it reaches 50%, which meets the baby’s needs for the first 4–6 months. By the time a child’s body weight doubles (5–6 months), antenatal iron reserves in his body are depleted.
In order to prevent IDA during artificial feeding, it is advisable to use iron-enriched formulas in children at risk for developing IDA. They are prescribed to full-term children at risk (from twins, triplets, with a large increase in weight), starting from 3-5 months of life, and to premature babies - from 1.5-2 months. The iron content in formulas for artificial feeding of children in the first half of life is 3–5–8 mg/l of the mixture, and for children in the second half of life – 10–14 mg/l.
The inclusion of iron-fortified complementary foods (fruit juices, fruit and vegetable purees, instant cereals) in children's diets significantly increases the amount of iron entering the child's body with food.
For children aged 4–6 months who are breastfed, and infants after 6 months of life who do not receive iron-fortified nutrition, it is advisable to prescribe iron supplements in a prophylactic dose of 1–2 mg/kg/day until 12–18 months of life.
IDA in young children is associated with early consumption of cow's or goat's milk, which contains high levels of protein. It should be noted that the development of IDA in these children is associated not only with low levels of iron in cow's milk and poor absorption, but also with the loss of iron due to microdiapedetic intestinal bleeding. Numerous studies have noted the relationship between the amount of non-adapted product consumed (milk, kefir) and the severity of microdiapedetic intestinal blood loss in infants. It was noted that sensitivity to unadapted products decreases with age and after 2 years of life, microdiapedetic intestinal bleeding is not observed when taking cow's milk. The mechanism underlying the increased excretion of hemoglobin in feces due to the intake of unadapted dairy products in young children is not precisely known. Some authors associate microdiapedetic intestinal bleeding with intolerance to cow's milk proteins.
The choice of drug for the correction of IDA is given special importance, since the duration of treatment can range from several weeks to several months. In this case, not only effectiveness is important, but also the absence of side effects and complications, adherence to the therapy, especially in pediatric practice.
Currently, all iron preparations are divided into two groups (Table 4):
- ionic iron-containing preparations (salts, polysaccharide iron compounds);
- nonionic compounds, which include drugs represented by the hydroxide-polymaltose complex (HPC) of ferric iron.
Therapy for iron deficiency conditions should be aimed at eliminating the cause and simultaneously replenishing iron deficiency with medicinal Fe-containing drugs.
Treatment of iron deficiency conditions should be carried out primarily with iron preparations for oral administration.
Oral administration of Fe preparations:
- increases hemoglobin levels only 2–4 days later than with parenteral administration;
- unlike parenteral, it extremely rarely leads to serious side effects;
- even if the diagnosis is incorrect, it does not lead to the development of hemosiderosis.
Parenteral administration of iron supplements is indicated only for special indications (poor intestinal absorption syndrome, condition after extensive resection of the small intestine).
Requirements for oral iron preparations used in pediatric practice:
- good bioavailability;
- high security;
- pleasant organoleptic properties;
- various dosage forms convenient for patients of all ages;
- compliance.
For young children, it is preferable to prescribe iron-containing drugs, available in the form of drops or syrup. Actiferrin (drops, syrup), Maltofer (drops, syrup), Ferrum Lek (syrup), Hemofer (drops) are good for children of this age group (Table 5).
For adolescent children, it is best to prescribe iron preparations such as Ferrum Leka (chewable tablets) or Tardiferon and Ferrogradument, which are slowly absorbed, ensuring prolonged and uniform absorption of medicinal iron in the intestines. As a rule, these drugs are well tolerated by patients.
After choosing an iron-containing drug and the method of its use, it is necessary to determine the daily daily dose of the drug and the frequency of administration (Table 6).
Recommended doses of ferrous iron are based on data showing that only 10-15% of the iron supplied to the body is absorbed.
Iron (III) preparations - GPC are used in children with IDA of different ages in a therapeutic dose of 5 mg/kg/day.
For latent iron deficiency, all iron preparations are used at half the therapeutic dose.
Preventive doses of iron supplements:
- for children under 3 years old – 1–1.5 mg/kg/day;
- for children over 3 years old – 1/2 the daily therapeutic dose.
It is known that treatment with salt preparations may be accompanied by stool disorders, and therefore therapy with ferrous iron preparations must be started with a dose equal to 1/4–1/2 of the calculated therapeutic dose, followed by gradual achievement of the full dose over 7–14 days. The rate of “gradual increase” of the dose to the therapeutic dose depends both on the severity of iron deficiency, and on the state of the gastrointestinal tract and individual tolerance of the drug. This technique allows you to select an individual dose depending on tolerability and reduce the risk of side effects of therapy with iron salt preparations.
It is well known that iron salt preparations in the intestinal lumen interact with food components and medications, complicating the absorption of iron. In this regard, iron salt preparations are recommended to be prescribed 1 hour before meals. The administration of Fe(III) preparations - GPC does not require the use of a gradual dose increase technique. Drugs in this group are prescribed immediately in full dose, regardless of food, since food does not affect their absorption.
The therapeutic effect of oral iron intake appears gradually. Initially, clinical improvement is noted and only after some time does hemoglobin normalize. The first positive clinical sign that appears during treatment with iron supplements is the disappearance or reduction of muscle weakness. The latter is due to the fact that iron is part of the enzymes involved in the contraction of myofibrils. On days 10–12 from the start of treatment, the content of reticulocytes in the peripheral blood increases. The increase in hemoglobin can be gradual or abrupt. Most often, the onset of an increase in hemoglobin levels occurs 3–4 weeks after the start of therapy. As numerous studies have shown, the disappearance of clinical manifestations of the disease is observed after 1–2 months of therapy, and the disappearance of tissue sideropenia occurs after 3–6 months of treatment. The daily dose of elemental iron after normalization of hemoglobin levels should correspond to 1/2 of the therapeutic dose (Table 7). Early cessation of treatment with iron preparations usually leads to relapses of IDA. The duration of the main course of treatment with iron supplements is 6–10 weeks, depending on the severity of the identified iron deficiency anemia. The duration of a preventive course of iron supplements in order to create an iron depot in the body is:
- for mild anemia – 1.5–2 months;
- for moderate anemia – 2 months;
- for severe anemia – 2.5–3 months.
Criteria for the effectiveness of treatment with iron supplements:
- the appearance of reticulocyte crisis on days 7–10 of treatment;
- increase in hemoglobin level – 10 g/l per week;
- complete normalization of clinical and laboratory parameters by the end of the course of treatment.
The refractoriness of iron deficiency anemia is due to the inadequacy of the prescribed therapy or anemia not associated with iron deficiency!
Parenteral drugs in the treatment of iron deficiency anemia should be used only according to strict indications!
Indications for parenteral administration of iron supplements:
- Short small bowel syndrome.
- Malabsorption syndrome.
- Nonspecific ulcerative colitis.
- Chronic enterocolitis.
It is better to use parenteral drugs not daily, but at intervals of 1–2 days. In this case, for the first 1–3 administrations, you can use half the dose.
Considering the duration of ferrotherapy, the choice of drugs for the correction of IDA in young children requires special attention. Both iron salt preparations and Fe(III)-HPA polymaltose complex preparations are effective in the treatment of VSD. Side effects and adverse events during oral ferrotherapy of IDA are mainly associated with exceeding recommended doses and are more often manifested by dyspepsia. Adverse reactions and undesirable effects that may develop during ferrotherapy in children are summarized in Table 8.
Parenteral iron supplements should be used only strictly for specific indications.
Blood or red blood cell transfusions for IDA are carried out extremely rarely and strictly for health reasons. The criteria for blood transfusion are a decrease in hemoglobin below a critical level in combination with signs of impaired central hemodynamics, hemorrhagic shock, anemic precoma, hypoxic syndrome (Table 9). Blood transfusion can also be carried out when hemoglobin and hematocrit values are higher than critical, if there is massive acute blood loss.
The effect of blood transfusions for IDA is short-term. A negative effect of blood transfusions on erythropoiesis was noted. In addition, there remains a high risk of transfusion infection of the recipient. If there are vital indications for replacement blood transfusion, preference is given to red blood cells or washed red blood cells at the rate of 10–15 ml/kg. Older children are usually transfused from 150 to 250 ml. Whole blood has not been used in pediatric practice in recent years.
Prevention of IDA in children includes:
1. Antenatal prevention:
- For all women in the second half of pregnancy, it is advisable to prescribe oral ferrotherapy or multivitamins fortified with iron.
2. Postnatal prevention:
- natural feeding with timely introduction of complementary foods (meat puree from 6–7 months);
- for children who are bottle-fed, from 2–3 months the introduction of formulas enriched with iron (12 mg/l);
- For premature babies, children from multiple pregnancies, those born with a large body weight, with rapid rates of weight and height gain, from the 3rd month to the end of the first half of the year, it is recommended to take prophylactic iron supplements in a dose equal to 1/3–1/2 of the daily therapeutic dose of elemental iron. iron (1.0–1.5 mg/kg/day).
Vaccination of children with IDA is carried out after normalization of hemoglobin levels.
Removal from dispensary registration is carried out after a year.
I. N. Zakharova , Doctor of Medical Sciences, Professor N. A. Korovina , Doctor of Medical Sciences, Professor A. L. Zaplatnikov , Doctor of Medical Sciences, Professor N. E. Malova , Candidate of Medical Sciences RMAPO , Moscow
How does low hemoglobin manifest?
Signs of low hemoglobin levels manifest themselves in different ways. They can be divided into groups of symptoms: asthenic, epithelial, cardiovascular, muscular and secondary immunodeficiency syndrome.
Asthenic symptoms are manifested by increased fatigue, irritability, emotional instability, lethargy, and absent-mindedness. Children sleep poorly, eat little or do not want to eat at all. Children may complain of tinnitus, dizziness and headaches.
Epithelial symptoms: children have a pale face, areas of the legs and nails, pale ears and oral mucosa. The skin is dry and often flakes. Hair becomes brittle and may fall out. “Sticks” appear in the corners of the mouth. The child may complain of a burning tongue and dry mouth, difficulty swallowing and nausea.
Cardiovascular symptoms: increased heart rate, rarely shortness of breath. Sometimes the child complains of pain in the heart area.
Muscle symptoms: muscles weaken, the child quickly gets tired of simple activities, and may involuntarily defecate day and night due to weakness of the sphincter muscle.
Secondary immunodeficiency syndrome is manifested by the fact that the child often suffers from colds. He often experiences otitis media, pneumonia and intestinal infections. Rare symptoms of low hemoglobin levels are an increase in body temperature to 38 0C, red-tinged urine, swelling on the face.
Low hemoglobin - what to do
If you notice any of the symptoms described above in your child, contact your pediatrician. He will examine the child, listen to heart sounds, and give a referral for a general and biochemical blood test, which can confirm a reduced hemoglobin level. After the doctor has diagnosed anemia and identified its cause, the child is prescribed treatment and diet.
Depending on the cause of anemia, the doctor prescribes different treatments. For example, in case of deficiency anemia (when the body does not receive enough nutrients), medications are prescribed to compensate for the deficiency: B vitamins or iron supplements. For B12-deficiency anemia, the doctor prescribes vitamin B12 (cyanocobalamin), and in severe cases, a transfusion of red blood cells is indicated. For anemia of a chronic disease, iron supplements and recombinant erythropoietin are prescribed.
Often, anemic syndrome manifests itself in other diseases, for example, with kidney pathology, infections or disorders of the gastrointestinal tract. In this case, the doctor prescribes treatment for the underlying disease, which will restore the level of hemoglobin in the blood.
How else can you increase hemoglobin in an infant?
An important factor in the treatment of anemia in infants is the normalization of the daily routine. Provide your baby with adequate sleep, long walks in the fresh air (1.5–2 hours a day), the opportunity to move a lot, and strengthen him. These factors also play a significant role in increasing hemoglobin.
Among some naturopaths there is still an opinion that the child’s hemoglobin is influenced by the emotional state of the mother. According to this theory, if a mother is full of fears, then these fears block the flow of life (which is equivalent to the flow of blood) both through her channels and through the channels of the child. If there is no place for joy and a smile in her life, but there is a lot of anger and resentment, then changing her diet will most likely not change anything. If you find a resource of inner joy in yourself, stop “spoiling” your blood, stop sorting things out with your family, then this is how you can increase your baby’s hemoglobin.

Foods that increase hemoglobin
Food can increase hemoglobin levels in iron deficiency anemia. For other types (dyshematopoietic, posthemorrhagic, hemolytic, B12-deficiency anemia), specific treatment with drugs, blood transfusions or surgery is required.
List of products that increase hemoglobin:
- tahini halva contains more than 50 mg of iron per 100 g of product. Halva also contains vitamins E, B, phosphorus, zinc and calcium. Some of these substances improve the absorption of iron in the digestive tract;
- meat products: beef, liver, tongue, rabbit, veal. The iron content in these products ranges from 5 to 30 mg per 100 g of product;
- dried mushrooms: they contain up to 30 mg of iron per 100 g of finished product;
- seafood: squid, shrimp, clams, caviar, scallops. They contain up to 30 mg of iron per 100 g of product;
- wheat bran contains up to 15 mg of iron per 100 g of product;
- seaweed contains up to 12 mg of iron per 100 g of product;
- beets - 30 mg of microelement per 100 g of product;
- pomegranate - up to 30 mg of iron per 100 g of product.
It is recommended to add foods enriched with cobalt and manganese to your daily diet: squid, tuna, cod, catfish, flounder, pike, oat bran, rice flour. These products help the absorption of iron and accelerate the production of hemoglobin. It is also recommended to add medicinal herbs to food: stinging nettle, tripartite string, infusion of rose hips, strawberries, rowan tea, black currants.
Folk remedies to increase hemoglobin
If HGB is reduced slightly (not lower than 100 g/l), there are no severe symptoms, then anemia can be treated with folk remedies.
At home, you can prepare decoctions, infusions from plants containing folic acid, iron, vitamin B12, as well as dietary dishes.
Basic recipes:
- Nettle decoction. Prepared from the tops of young shoots. Add one glass of herbs to 1 liter of boiling water, cook for about 5 minutes and filter. Drink 1-2 glasses daily.
- Potato juice. The drink stimulates hematopoiesis. Drink 100 ml before meals 2-3 times a day for 2-3 weeks.
- Rowan infusion. Pour two teaspoons of ripe berries into one glass of boiling water and leave for at least 1.5 hours. Take 100 ml 2-3 times.
- Infusion of rosehip berries. A handful of dried fruits are poured into 500 ml of boiling water, left in a thermos overnight and drunk 100 ml before meals several times a day.
- Carrot and sour cream salad. For breakfast, eat 100-150 g of carrots, this stimulates the production of red blood cells and hemoglobin.
For low HGB, freshly squeezed juices from pomegranate, carrots, beets, as well as grapefruits, oranges, kiwis, blueberries, black currants, raspberries, and persimmons are useful.
The disadvantages of traditional methods are the duration of treatment, side effects such as diarrhea, flatulence, and exacerbation of gastritis.
If your hemoglobin level continues to decrease during treatment, malabsorption or bone marrow disease may be suspected. Additional examination is required.