What it is?
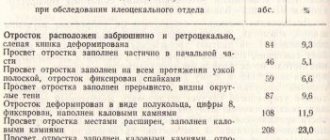
Appendicitis is an acute inflammation of the cecum, also known as the appendix (Figure 1).
Figure 1. The appendix (a), a pouch-shaped extension of the cecum about 7-9 cm long, is located in the lower right quadrant of the abdomen. When the appendix becomes inflamed (b), appendicitis develops. Source: CC0 Public Domain
Appendicitis always manifests itself unexpectedly. This is not the case when acute manifestations of the disease are preceded by a so-called prodromal period. If the appendix hurts, the patient may need emergency care.
Among acute surgical diseases of the abdominal cavity, appendicitis takes an honorable first place - 89% of the total. Most often it occurs in young people aged 15-30 years, and women are more susceptible to this pathology. However, this does not mean that adults and older people do not suffer from this disease - it can occur at 50 or even 70 years of age. Although such cases are rare, they still occur, and the danger to health is much higher, because the older a person is, the more concomitant diseases he has that slow down the recovery process.
Causes
Today, experts cannot say with complete confidence what exactly is the trigger for inflammation of the appendix.
It is generally accepted that the main cause of inflammation of the appendix is blockage of its lumen, resulting in the accumulation of mucus and its subsequent infection.
The role of hereditary predisposition to appendicitis has not yet been studied well. However, already now some domestic and foreign experts, based on their clinical observations, are suggesting that genetic factors can still contribute to the development of appendicitis. In addition, there are congenital features such as bending or narrowing of the appendix - they can cause congestion and inflammatory processes.
There are also less popular, but still accepted for consideration in wide scientific circles, theories affecting the possible causes of appendicitis:
- Vascular. There is an assumption that systemic vasculitis and other vascular diseases leading to disruption of the blood supply to the cecum can cause inflammation of the appendix.
- Endocrine. The mucous membrane of the large intestine contains the so-called. enterochromaffin cells, which secrete substances that promote inflammatory processes. It is in the appendix that there are a lot of such cells, so the theory is considered viable.
- Infectious. Many scientists believe that infectious diseases (for example, amoebiasis or typhoid fever) can cause inflammation of the appendix. True, so far no one can clearly explain which bacteria can be classified as specific causative agents of appendicitis.
Types of disease
Most often, appendicitis has an acute course. Some scientists insist on the possibility of developing chronic appendicitis in patients who have not previously suffered an acute form of the disease, but this statement is still the subject of controversy in scientific circles.
Thus, the clinical classification includes the following types of appendicitis:
- Acute uncomplicated.
- Acute complicated (read about complications in the next section of the article).
- Chronic.
Acute appendicitis, in turn, is usually classified according to the nature of pathological changes in tissues determined by histological examination.
This classification is called clinical-morphological and divides the acute form of appendicitis into the following types:
- Catarrhal. The most common and at the same time the least dangerous type of appendicitis, in which only the mucous membrane of the appendix becomes inflamed. The attack begins with diffuse pain in the upper abdomen, which after a few hours moves to the right iliac region. The abdomen is not tense and takes part in breathing movements. The temperature may be normal, but more often there is an increase to approximately 37.5°C.
- Purulent (phlegmonous). Foci of purulent inflammation cover the entire appendix, while it increases significantly in size, and swelling of the intestinal walls is noted. Inflammation of the peritoneum (peritonitis) may occur. The main symptom is pain in the right iliac region with constantly increasing intensity. The tongue is coated, vomiting is noted (sometimes multiple times). The abdominal muscles are moderately tense.
- Gangrenous. There is extensive necrosis of the walls of the appendix, and its color becomes black-green. The clinical picture resembles phlegmonous appendicitis, but the intensity of the pain is usually less, since many of the nerve endings in the appendix have died by this time. The pulse is weak, chills are often observed.
- Perforated. A perforated hole is formed in the wall of the appendix, which is fraught with the entry of purulent contents into the abdominal cavity. Intense pain subsides after a few hours, but soon returns, throughout the entire abdomen. There is fever and nausea, but the patient himself has almost no complaints. This is explained by euphoria against the background of severe general intoxication. The abdominal muscles are tense and do not take part in breathing movements.
Features of chronic appendicitis
The chronic form of pathology is represented by several types of diseases, differing in symptoms, frequency of attacks, and possible complications. Residual or residual appendicitis develops after an acute form of the disease that ends in spontaneous recovery. Residual appendicitis is characterized by periodic dull pain in the iliac region on the right side and the formation of adhesions.
Recurrent appendicitis is characterized by the occurrence of attacks against the background of a previously suffered acute form of the disease. After exacerbations, the health status returns to normal. Chronic appendicitis in its primary form develops independently, without previous acute attacks.
What is dangerous about appendicitis: complications
Lack of timely medical care can lead to perforation (rupture of the wall) of the appendix and the development of life-threatening complications:
- peritonitis (inflammation of the peritoneum),
- purulent inflammation of tissues - abscesses (subphrenic, interintestinal, retroperitoneal, periapendicular, hepatic),
- pylephlebitis (inflammation and thrombosis of the portal vein),
- sepsis (spread of infection throughout the body).
All of the above conditions are accompanied by a severe clinical picture: unbearable abdominal pain, high fever, vomiting, confusion. In the absence of emergency medical care, death occurs.
Features of the acute form in children
Primary diagnosis of appendicitis in children over 7 years of age is complicated. Although the disease at this age develops almost like in adults, children experience great fear of doctors, hospitalization, and surgery. Therefore, they can say that the pain has gone away and their health has returned to normal.
As a rule, the first signs of appendicitis appear suddenly in children: at home, at school, or while out for a walk. If we are talking about children under 3 years of age who are unable to clearly describe their feelings, then parents should recognize the following alarming symptoms:
- refusal to eat;
- cry;
- sleep disturbance;
- decreased activity;
- screaming when touching the stomach in the navel area;
- nausea;
- vomit;
- diarrhea with mucus in the stool;
- stool retention (rare);
- painful urination;
- elevated temperature (up to 40°), for infants – up to 37.5°;
- crying when squatting, pulling the right leg towards you in this position. Source: A.Yu. Razumovsky, A.F. Dronov, A.N. Smirnov, M.A. Golovanev Acute appendicitis in children // Russian Bulletin, 2013, vol. III, no. 4, pp. 125-132
If the child complains of pain or is naughty, try placing him on his left side. In this position, the pain will decrease, and you will immediately notice positive changes in the baby’s behavior. This factor is a reason to immediately consult a doctor for further treatment.
The first symptoms of appendicitis in children:
- abdominal pain (3-4 cm above the navel);
- lethargy, weakness, nausea, fever;
- impatience of belly touching.
Symptoms of appendicitis
Acute appendicitis is characterized by an acute onset. Symptoms usually appear at night or early in the morning, and the clinical picture develops rapidly. The first sign is the appearance of diffuse nagging pain in the upper abdomen (epigastric region). As the pain intensifies, it becomes sharp and throbbing, moving to the lower right side of the abdomen. General symptoms of an “acute abdomen” include (Fig. 2):
- increase in temperature (usually up to 37.5 C, but in complicated forms there is an increase to 40 C),
- nausea and vomiting,
- dry mouth,
- lack of appetite,
- stool disorders (both constipation and diarrhea are possible),
- cardiopalmus,
- grayish coating on the tongue,
- bloating and flatulence.
Figure 2. Classic symptoms of an “acute abdomen” that often accompany acute appendicitis.
Source: Adobe Stock Appendicitis has several specific symptoms that help distinguish it from other diseases:
- Bartomier-Michelson's symptom - pain on palpation of the cecum intensifies if the patient lies on his left side,
- Voskresensky's symptom - the doctor uses his fingertips to make a quick and light sliding movement from top to bottom towards the right iliac region, while the pain intensifies at the end point of the movement,
- Dolinov's symptom - increased pain in the right lower abdomen when it is retracted,
- Volkovich-Kocher symptom - first the pain occurs in the upper abdomen, and after a few hours it moves to the right iliac region,
- Krymov-Dumbadze symptom – increased pain on palpation of the umbilical ring,
- Razdolsky's (Mendel-Razdolsky) symptom - percussion of the abdominal wall is accompanied by increased pain in the right iliac region,
- Sitkovsky's symptom - the occurrence or intensification of pain in the right lower abdomen if the patient lies on his left side,
- Rovsing's symptom is the occurrence or increase in intensity of pain in the right lower abdomen with compression of the sigmoid colon and push-like pressure on the descending colon.
A rare cause of appendix pain is a tumor. Appendiceal cancer usually does not cause any symptoms until the disease reaches an advanced stage. A large tumor can cause bloating. Pain may occur if the cancer spreads to abdominal tissue.
A malignant tumor can develop simultaneously with acute appendicitis. It is usually discovered after the appendix is removed. Cancer can also be found by chance during a routine examination or diagnostic procedures aimed at identifying other pathologies. Diagnosis of cancer includes biopsy, ultrasound and MRI.
Risk factors for developing appendix cancer include:
- smoking,
- the presence of gastritis and some other gastrointestinal diseases,
- cases of appendix cancer in relatives,
- age (the risk of developing cancer increases with age).
Which side does it hurt on?
As a rule, pain with appendicitis is localized in the lower right part of the abdomen, since that is where the appendix is located - between the navel and the right ilium (Fig. 3).
Figure 3. Pain from appendicitis is usually worst at the site of inflammation - in the lower abdomen on the right side. Source: CC0 Public Domain
However, in rare cases, pain is noted on the left side. There are several reasons for this phenomenon:
- Excessive mobility of the colon.
- Irradiation. Appendicitis is known for the fact that when pressing on the abdomen, the pain can radiate to any part of the abdomen (including to the left).
- Mirror arrangement of internal organs (that is, organs that should normally be on the right are located on the left side, and vice versa).
Nature of pain
At the beginning, the pain of appendicitis can be diffuse and nagging. Later, as the disease progresses, it becomes sharp and pulsating. In rare cases, the pain appears suddenly, simultaneously with bouts of unrelieved vomiting and temperature fluctuations.
How to distinguish it from other diseases?
Pain caused by inflammation of the appendix usually becomes worse when coughing and sneezing, moving and breathing. There is also a phenomenon characteristic of appendicitis, which is called “Obraztsov’s symptom” - increased pain when the patient raises his right leg in a standing position.
A characteristic feature of appendicitis, which makes it possible to distinguish it from other diseases of the abdominal cavity, is that the pain subsides if you take a position lying on your side with your knees pulled up to your stomach.
Leukocytosis in complications of appendicitis
With the catarrhal form of appendicitis and initial destructive changes, leukocytosis is most often moderate, in the range of 12-14 x109 /l. If during this period there is no adequate treatment of the disease, that is, surgery, then in most cases complications develop.
The most common of these is perforation of the organ and release of purulent mass into the abdominal cavity. Perforation with subsequent development of peritonitis can also be determined by the clinical picture of the disease and according to instrumental examinations.
- Peritonitis is characterized by pain throughout the abdomen, noticeable bloating, lack of stool, and general symptoms of intoxication. As this complication develops, the pulse becomes thread-like and frequent, and can reach up to 140 beats per minute. If you do a blood test at this time, it will reveal pronounced leukocytosis, increased compared to the norm of ESR. If leukopenia is detected, that is, a decrease in the number of leukocytes in the peripheral blood, then this indicates a severe pathology.
- Moderate leukocytosis can also occur in humans with the development of appendiceal infiltrate. This term refers to a condition in which inflammation from the appendix spreads to the intestinal organs and a welded conglomerate is formed. In addition to an increase in the number of leukocytes, this complication reveals a shift in neutrophils. A patient with appendiceal infiltrate is treated in the first weeks without surgery; he is prescribed antibacterial therapy, under the influence of which the inflammation is relieved and blood tests return to normal.
- Appendiceal abscesses develop 8-12 days from the onset of the disease. Ulcers can be located anywhere in the abdominal cavity. This complication can be suspected by a deterioration in the patient’s general well-being, an increase in temperature, chills, and an increase in pulse. Leukocytosis increases in the blood, and a shift to the left of the leukocyte formula is determined.
- Pylephlebitis is one of the most serious complications of appendicitis. This term refers to purulent thrombophlebitis of the portal vein of the liver. The general condition of the patient is very serious, the most constant symptom is stunning chills, rapid pulse and temperature up to 40 degrees. There is high leukocytosis and ESR in the blood.
When making a diagnosis of appendicitis and identifying its complications, all blood parameters are taken into account, they are carried out repeatedly throughout the day, identifying all changes. The decision to choose a treatment method is made taking into account the patient’s condition.
Diagnostics
Diagnostic measures begin with palpation. When pressing on the abdomen on the right and sharply removing the hand, the pain intensifies - this is called the Shchetkin-Blumberg symptom.
Laboratory diagnostics:
- Blood test (the presence of appendicitis is indicated by an increased content of leukocytes and immature neutrophils).
- Urinalysis (done to make sure that the cause of pain is not a disease of the urinary system).
Instrumental diagnostics:
- Ultrasound examination of the abdominal cavity.
- CT scan.
- Radiography.
In doubtful cases, the doctor may prescribe diagnostic laparoscopy: an endoscope is inserted through an incision in the abdominal wall, with the help of which a direct examination of the appendix is performed. This procedure is classified as a diagnostic operation, but the accuracy of the study tends to be 100%.
How to determine a disease in a child?
As soon as you notice strange behavior associated with the symptoms listed above, you need to check your child for acute appendicitis. To do this, feel your stomach and determine the source of pain. This must be done carefully so as not to cause harm. If the pain is localized on the right, lightly press on the abdomen - you will probably find a lump. Moreover, if you suddenly remove your hand from the place of pressure, the pain will most likely intensify. This indicates the presence of acute appendicitis, and parents urgently need to call an ambulance. If you hesitate in this case, there may be peritonitis and/or rupture of the appendix.
Treatment
As a rule, appendicitis is treated surgically—if the diagnosis is confirmed, the appendix is removed.
Urgent Care
If all the symptoms point to appendicitis, there is no need to make independent attempts to alleviate the condition; the only correct solution is to call an ambulance. Thermal procedures are strictly contraindicated (that is, you cannot apply a heating pad).
Important! If you suspect acute appendicitis, you should urgently call an ambulance at 103. If the attack began far from the city, you can call the single rescue service at 112.
Before the ambulance arrives, you should not take painkillers. The patient will have to be patient, since pain relief may change the clinical picture and make diagnosis difficult. It is forbidden to eat (in rare cases, appendicitis may increase appetite), and even drinking is not recommended. If you are very thirsty, you can take a couple of small sips of water, but no more.
Important! The patient should not move independently - any physical activity can provoke a rupture of the appendix.
How is the operation performed?
A standard operation to remove the appendix is performed under general anesthesia and lasts on average 40-50 minutes. With a classic appendectomy, a 6-8 cm incision is made in the right iliac region, and the tissue is pulled apart using special instruments. The surgeon removes part of the cecum and removes the appendix, after which the vessels and tissues are sutured.
During laparoscopic removal of the appendix, punctures are made in the abdominal wall. The doctor inserts an endoscope into one hole, which helps him monitor the progress of the operation. Surgical instruments are inserted into the other two holes (Fig. 4).
Figure 4. Laparoscopic removal of the appendix causes the least amount of tissue trauma. Source: CC0 Public Domain
In case of rupture of the appendix and the development of peritonitis, a more complex operation is required - a median laparotomy (incision length is approximately 10 cm) with sanitation of the abdominal cavity, carried out using drainage devices. In the postoperative period, the patient must undergo a course of broad-spectrum antibiotics.
Drug therapy
Domestic experts consider drug treatment of appendicitis to be ineffective. In Europe, the approach is somewhat different: when appendicitis worsens, the doctor first prescribes a course of antibiotics, and only if it does not help, the patient is sent for surgery. Russian surgeons consider this approach to be unjustifiably risky, since delay in surgical removal of the appendix can lead to complications and even death.
Leukocytosis after appendectomy for appendicitis
You should not assume that after the operation all blood counts immediately return to normal. Moderate leukocytosis will be detected for several days after appendectomy and this is considered normal. This is due to the fact that the inflammatory reaction does not go away immediately after removal of the appendix from the body and with the healing of the postoperative wound.
Most patients after an appendectomy are prescribed antibiotics for several days; they help cope with inflammation and are also prescribed for prophylactic purposes to reduce the risk of developing all kinds of postoperative complications.
The operated patient is discharged home only after the blood counts return to normal. If leukocytosis does not decrease, then this is an indicator of the presence of an inflammatory reaction in the body. This in turn is considered the main contraindication to discharge.
To understand what causes an increase in the number of white blood cells in the blood after surgery, the surgeon must carefully examine the patient. Most often, the cause of moderate leukocytosis is the failure of the postoperative suture. Suppuration, suture dehiscence, fistulas - all this causes inflammation.
To prevent further changes, the doctor prescribes dressings with antiseptic agents, an additional antibiotic is selected, and physiotherapy is used. Usually, after several days of such treatment, everything returns to normal and the patient is discharged home.
More dangerous for the operated person are intra-abdominal complications, which also lead to leukocytosis, high ESR and other changes in blood parameters. Repeated surgery is often required to eliminate these complications.
With appendicitis, a person’s rapid recovery depends largely on how quickly he seeks medical help. Early surgery shortens the recovery period and reduces the risk of developing severe and sometimes life-threatening complications by tens of times. Therefore, at the first symptoms reminiscent of appendicitis, it is necessary to contact a medical facility in the first hours of illness.
Prevention
To reduce the likelihood of acute appendicitis, you should adhere to the following rules:
- include a sufficient amount of fiber in the diet to prevent constipation and putrefactive processes in the intestines,
- avoid uncontrolled use of antibiotics to prevent the development of dysbiosis,
- increase immunity: lead an active lifestyle, avoid bad habits, regularly take vitamin complexes,
Previously, preventive appendectomy was practiced abroad - American doctors removed children's appendixes with the same zeal as Soviet doctors cut out children's tonsils at the slightest sign of a cold. However, this practice has now been abandoned because after prophylactic appendectomy, children suffered from regular digestive disorders and were prone to frequent colds due to weakened immunity.
Causes of appendicitis in children
There is no consensus or 100% certainty among doctors about why inflammation occurs. However, doctors are sure of one thing: for the disease to develop, there must be bacteria in the intestines, and the lumen of the appendix must be blocked (the reasons include eating seeds, pits, etc.).
Other reasons:
- diseases that provoke a decrease in immunity (ARVI, otitis media, sinusitis, etc.);
- decreased immunity;
- helminths in the intestines;
- foreign objects in the intestines (berry seeds, fish bones, sunflower seeds, peeled pumpkins, etc.).