Features of the manifestation of appendicitis
Appendicitis is inflammation of the appendix, the most common pathology among all diseases of the digestive system. According to statistics, the disease occurs in 7–10% of the population of all countries of the world. Medical specialists cannot predict the likelihood of developing a pathological process in patients based on diagnostic data. Acute appendicitis can suddenly appear in adults, adolescents and preschool children, with the exception of children under one year old. The most vulnerable age category is from 5 to 40 years, and before 20 years of age, acute appendicitis is more common in men, after 20 years - in women. The insidiousness of the disease lies in its rapid development and frequent complications that can be life-threatening. When the first warning symptoms appear, you should immediately call a doctor or emergency help.
Appendix and immunity
For a long time it was believed that the appendix is a vestigial organ that has lost 100% of its functionality. At the beginning of the 20th century, the appendage was even removed in infants to prevent the development of appendicitis in later life. Observations of patients without an appendix led to the conclusion that these people have reduced immunity and are more susceptible to infectious diseases. Modern scientists are of the opinion that the appendix is a necessary and useful organ that helps maintain an optimal balance of the intestinal environment, provides protection against pathogenic microorganisms and infectious agents, and helps recover from poisoning and stress imbalance of microflora.
Treatment of acute appendicitis is almost always surgical. Removing the appendix does not necessarily mean that the patient will have health problems, but the immune and digestive systems may become less functional. To avoid an imbalance of the intestinal flora after surgery, special dietary supplements containing probiotics and prebiotics are introduced into the diet.
Forms of the disease
Depending on the nature of the disease, acute and chronic appendicitis are distinguished. Acute appendicitis begins suddenly and develops rapidly. It is extremely rare that symptoms go away on their own and a cure occurs.
Chronic appendicitis is a rarer form of pathology. In most cases, this is a consequence of acute appendicitis that was not removed. The symptoms are less pronounced, a period of relative calm is replaced by a sharp exacerbation. In the chronic course of the disease, there is a deterioration in health, the appearance of weakness and malaise. According to the medical classification, the chronic form of the disease can be complicated or uncomplicated.
Uncomplicated forms of appendicitis include:
- catarrhal (inflammation of the mucous membrane of the appendix);
- destructive (accompanied by tissue destruction with the formation of phlegmon, or gangrenous type).
Complications of appendicitis include pathological processes such as rupture of the organ wall (perforation), formation of infiltrate around the appendix, peritonitis (inflammation of the peritoneum), blood poisoning (sepsis), purulent inflammation with portal vein thrombosis (pylephlebitis).
Features of chronic appendicitis
The chronic form of pathology is represented by several types of diseases, differing in symptoms, frequency of attacks, and possible complications. Residual or residual appendicitis develops after an acute form of the disease that ends in spontaneous recovery. Residual appendicitis is characterized by periodic dull pain in the iliac region on the right side and the formation of adhesions.
Recurrent appendicitis is characterized by the occurrence of attacks against the background of a previously suffered acute form of the disease. After exacerbations, the health status returns to normal. Chronic appendicitis in its primary form develops independently, without previous acute attacks.
Chronic appendicitis clinic and diagnosis
The leading symptom of chronic appendicitis is moderate stabbing, aching or pressing pain in the right iliac region, aggravated by walking, running, physical activity and poor diet. The pain most often radiates to the right leg. The localization and irradiation of pain varies depending on the position of the cecum and the appendix.
In patients with recurrent and residual chronic appendicitis, the symptoms of the disease appear after previous attacks of acute appendicitis, and in cases of primary chronic appendicitis, they develop gradually, without noticeable reasons. Not excluded. the possibility that the cause of primary chronic appendicitis is diseases of other digestive organs, diseases of the genital area in women and asymptomatic acute inflammation of the mucous membrane of the appendix.
The pain periodically intensifies, attracts the attention of patients, interferes with their normal life and work, depresses them with the possible occurrence of an acute attack and the need for emergency surgery, which often leads to neurasthenic conditions and emaciation.
In many patients, pain is accompanied by nausea, rarely by vomiting. Almost all patients have constipation, which causes intoxication and worsens the course of appendicitis. Sometimes patients with chronic appendicitis complain of decreased appetite, heartburn, belching, bloating, rumbling, and increased pain after eating rough food. With a pronounced clinical picture, the performance of patients decreases.
The general condition of the patients is satisfactory; they often look quite healthy. The tongue is covered with a whitish coating, and sometimes there is an unpleasant odor from the mouth. With prolonged suffering, some laxity of the abdominal wall in the right ilioinguinal region may be detected. Performing active movements is accompanied by slight pain in the right iliac region or in another place, according to the location of the appendix. In the same area, mild percussion pain is detected, and sometimes an increase in percussion sound (the cecum is swollen).
Palpation gives pain in the right iliac region, increasing with deep palpation. In many patients, a swollen, compacted and painful cecum is palpable. In thin people, and... In children, you can palpate the appendix and determine its length and thickness. Palpation of the appendix must be carried out carefully. Wullstein, Wilms (1913) in their book report an observation when, after persistent palpation of the appendix, a “hematoma the size of a walnut” formed in the latter. Auscultation in the diagnosis of chronic appendicitis is of little importance. Examination through the rectum and through the vagina in women is necessary for differential diagnosis and may be valuable in the pelvic position of the appendix.
In chronic appendicitis, there are weakly positive symptoms of Sitkovsky, Obraztsov, Bartomier-Mikhelson, Rovzing. Prolonged suffering with repeated attacks of acute appendicitis can lead to atrophic changes in the muscles in the right iliac region, and then Ivanov’s second symptom becomes positive - an increase in the distance between the navel and the upper spine of the right iliac bone. In some patients, after a recent exacerbation (intensification) of pain, which did not give a picture of acute appendicitis (the patient suffered an exacerbation on the legs without consulting a doctor), there may be subtle (very weak) Voskresensky and Shchetkin-Blumberg symptoms.
Diagnosis should be based on a detailed study of complaints, anamnesis, objective and additional research methods. If the diagnosis of chronic appendicitis is beyond doubt, surgery is indicated, and there is no need to expand additional research methods—of course, if there are no other indications for this (for example, suspected gastric ulcer). If you doubt the diagnosis or lack confidence, you should examine the gastric juice, do fluoroscopy of the stomach and intestines, irrigoscopy, and conduct a special study of the liver, gallbladder or genitourinary organs. In the diagnosis of chronic appendicitis, great importance is attached to x-ray examination of the cecum and appendix. The X-ray method for studying chronic appendicitis is highly appreciated by A.A. Rusanov (1960), G.M. Shchekotov, S.G. Zhukova (1970). I.X. Gevorkyan (1970) writes that the X-ray diagnosis of chronic appendicitis is confirmed by morphological examination in 99.5% of patients. E.S. Drachinskaya and A.L. Polyakov (1969), A.M. Erukhimovich (1967) consider x-ray examination to be leading in the diagnosis of chronic appendicitis. Radiological signs of chronic appendicitis include pain in the area of the cecum under the screen, stasis in the appendix and cecum, pain and limited mobility of the appendix, limited mobility of the cecum, non-filling of the appendix with contrast mass, deformation of the appendix. Relative signs of chronic appendicitis include spasm of the pylorus, spasm of the bauhinium valve, and dilatation of the terminal ileum. Of great interest are the data of G.M. Shchekotova and S.G. Zhukova, reflecting radiological changes in the appendix in chronic appendicitis (Table 5).
Chronic appendicitis clinic and diagnosis 1
The scope of the study is determined by the difficulty of diagnosis. If it is impossible to resolve the issue of the presence of chronic appendicitis (such cases do occur), it is necessary to move on to solving the issue of the patient’s need for surgery. At the same time, along with many factors, the course of the disease (progresses or regresses) and the effectiveness of conservative treatment are taken into account.
A thorough analysis of diagnostic and tactical errors in chronic appendicitis shows that they are mainly associated with violation of the basic rules of examining the patient. Neglecting these rules and haste in work is a source of mistakes. One should never make exceptions when examining a patient; one should not omit a single element from the medical history, no matter how good the patient’s condition may seem and the diagnosis undoubted.
An experienced resident with extensive work experience examined patient K., 57 years old, who was admitted to the clinic on 27/VIII-71 with a diagnosis of chronic appendicitis. The diagnosis did not raise any doubt; there was a history of two attacks of appendicitis, a typical clinical picture, and expressive symptoms. The patient's condition is good. “The boundaries of the heart are normal, the apical impulse is in the fifth intercostal space on the left, the pulse is 74 beats per minute, rhythmic, with good filling and tension.” As it later turned out, the doctor made this recording without examining the cardiovascular system and made his first serious mistake.
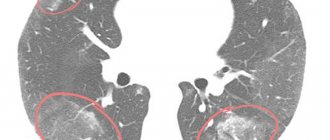
Not paying attention to the accelerated ROE (31), a shift in the white blood count (second error) and not considering it necessary to refer the patient for mandatory fluoroscopy of the lungs (third error), the doctor prescribed the patient for surgery, confidently reporting at a clinical conference about the typical clinical picture of chronic appendicitis and obvious indications for surgery (fourth error1 - the doctor did not report changes in the blood and unperformed fluoroscopy at the conference).
On 30/VIII-71, the attending physician, under local anesthesia, opened the abdominal cavity in the right iliac region, found the sigmoid colon instead of the cecum and called the professor into the operating room. The cecum with the appendix was located in the left iliac region. An appendectomy was performed. The anesthesiologist discovered that the patient's heart was in the right side of the chest.
In the postoperative period, mistakes began to be corrected. They did an X-ray of the chest and stomach. The diagnosis of complete inversion of the internal organs (situs viscerum inversus) was confirmed, and a large polyp in the pyloric region and cancer in the cardiac region were discovered in the stomach. After appropriate preparation, the patient soon underwent a gastrectomy, which he tolerated well.
A morphological study confirmed all three diagnoses: chronic appendicitis, cancer and gastric polyp.
If the doctor had not made four serious mistakes one after another, then, of course, the patient would have been operated on for a malignant tumor of the stomach with simultaneous removal of the vermiform appendix, which was currently bothering the patient more than the asymptomatic cancer process. The diagnosis would have been made accurately if the doctor had not betrayed his soul and listened to the heart of a healthy-looking person. Having discovered the heart on the right, he, of course, would order fluoroscopy of the stomach and intestines (to determine their position) and would receive the main diagnosis, concomitant disease and a clear plan of action.
The given example not only illustrates the erroneous diagnosis of chronic appendicitis (there are many such examples in the literature), but reveals the mechanism of diagnostic and tactical errors caused by a violation of a seemingly completely insignificant point in the study of a patient with chronic appendicitis.
Causes of the disease
Despite the enormous prevalence of the pathology, representatives of official medicine cannot compile a systematic list of the reasons leading to the development of the disease. At the same time, there are several theories about the origin and development of appendicitis. These include:
- Hypothesis about the infectious nature of the disease. According to the theory, the development of acute appendicitis is caused by a disruption of the microflora inside the organ, which leads to the activation of opportunistic bacteria and their transformation into a pathogenic environment. The theory, first published in 1908 by the German scientist Aschof, is supported by many modern scientists.
- Neuropsychic disorders (angioneurotic theory). Many scientists believe that as a result of neuroses and mental disorders, vascular spasm occurs in the tissues of the appendix, as a result of which their supply of nutrients deteriorates. As a result of this process, some tissue fragments die and gradually become foci for the spread of various infections.
- Stagnation phenomena (the theory of stagnation). Proponents of this theory believe that appendicitis develops due to intestinal hypotension, which leads to stagnation of feces and their entry into the appendage of the colon.
Thus, there is no single mechanism for the development of the disease, but risk factors cannot be denied, which include:
- narrowing or blockage of the lumen of the appendix by a foreign body, including tumors, helminths, fecal deposits;
- the presence of infectious pathogens, bacteria and viruses that cause inflammation of intestinal tissue;
- external injuries (blows to the abdomen), as a result of which the appendix is displaced or blocked;
- systemic vascular inflammation (vasculitis);
- metabolic disease;
- disturbance of intestinal motility;
- unbalanced diet.
The walls of the appendix become more vulnerable to the effects of all of these negative factors as the functionality of the immune system decreases.
Acute appendicitis
Appendicitis is an acute inflammation of the inner lining of the appendix. It is the most common cause of acute surgical interventions and most often occurs between 10 and 30 years of age.
The pain usually starts in the center of the abdomen, then moves down to the lower right side. As a rule, it intensifies within 12-18 hours and becomes very pronounced.
Treatment for appendicitis involves immediate surgical removal of the appendix. Without surgery, it leads to serious complications.
Synonyms Russian
Inflammation of the appendix.
English synonyms
Appendicitis.
Symptoms
- Aching pain in the abdomen that begins in the navel area and then usually moves to the lower right side of the abdomen.
- Short-term nausea, vomiting.
- Loss of appetite, constipation.
- Abdominal pain that gets worse over several hours.
- Acute pain in the lower right part of the abdomen, which occurs when pressure suddenly decreases during palpation.
- Abdominal pain, aggravated by coughing, walking, or sudden movements.
- Pain in the lower right abdomen when palpated.
- Increase in body temperature to 37.7-38.3 °C.
- In children under 3 years of age, behavior changes and refusal to eat, as well as diarrhea and vomiting.
- In elderly patients, symptoms may not be expressed.
The difficulty lies in the fact that typical symptoms are characteristic of only 50% of patients. Sometimes abdominal pain may be absent, not localized to the right side, etc. Atypical symptoms are usually observed in older people and pregnant women.
General information about the disease
Appendicitis is an acute inflammation of the inner lining of the appendix - the vermiform appendix of the cecum (the cecum is the initial section of the large intestine in the lower right part of the abdomen; the appendix is a small appendix of the cecum, the function of which in the body has not yet been precisely established). It is the most common cause of acute surgical interventions and most often occurs between 10 and 30 years of age.
Inflammation of the appendix is caused by its blockage, which may be associated with increased pressure in the intestinal lumen. This may happen due to:
- lymphoid hyperplasia - an increase in lymphoid tissue located fragmentarily along the intestinal wall;
- fecal stones (fragments of hardened feces);
- parasites;
- foreign bodies, tumors.
The blockage leads to expansion of the process and infection. As a result, the outflow of venous blood from the appendix is disrupted, which causes oxygen starvation of its tissues.
Also, in some cases, appendicitis is a consequence of inflammatory or infectious bowel diseases.
The following types of appendicitis are distinguished.
- Catarrhal (simple). It occurs most easily and is characterized by minimal inflammation of the appendix. In this case, suppuration does not occur.
- Phlegmonous. The appendix ulcerates, becomes inflamed and suppurates.
- Gangrenous. It is a consequence of thrombosis of the vessels feeding the appendix, resulting in tissue necrosis, which leads to peritonitis - inflammation of the peritoneum (the membrane covering all organs of the abdominal cavity). This type of appendicitis is extremely dangerous.
- Perforated. When it occurs, suppuration of the appendix occurs, followed by melting of the tissues, a hole is formed in the appendix and its contents enter the abdominal cavity. This causes inflammation of the peritoneum, which is accompanied by systemic inflammation of the entire body. Accompanied by severe pain.
The appendix may be located in an atypical location: behind the cecum, in the pelvis, close to the liver. In this case, the symptoms will differ significantly from the classic ones and resemble the signs of other diseases. Making a diagnosis with an atypical location of the appendix can be difficult. In addition, the position of the appendix changes during pregnancy, which can also complicate diagnosis.
Appendicitis can lead to the following complications.
- Appendicular infiltrate is a formation consisting of the cecum, appendix, loops of the large intestine and omentum. It is formed at the location of the appendix on the 3-5th day from the onset of acute appendicitis and usually resolves on its own within a month. In some cases, it may suppurate with the formation of a periappendiceal abscess.
- Peritonitis is an inflammation of the peritoneum, the membrane that covers all organs of the abdominal cavity from the outside.
- Periappendicular abscess is a purulent inflammation of tissues, their melting and the formation of a purulent cavity. The appearance of an abscess requires its surgical removal.
Who is at risk?
- People aged 10-30 years.
- Suffering from inflammatory bowel disease.
- Suffering from parasitic intestinal diseases.
- Pregnant women.
Diagnostics
If classic symptoms are present, the diagnosis of appendicitis is usually not in doubt. In case of atypical or erased symptoms, additional research is required to diagnose it.
Laboratory research
- Complete blood count (without leukocyte formula and ESR). In 80-85% of patients with appendicitis, the level of white blood cells increases. At the same time, their normal number does not exclude the presence of appendicitis. Since during pregnancy there is a physiological increase in the level of leukocytes, a general blood test in this case does not help in diagnosing the disease.
- Leukocyte formula. Determines the ratio of different types of leukocytes as a percentage. With appendicitis, a significant predominance of neutrophilic leukocytes can be observed.
- C-reactive protein. It is a protein produced in the liver that quickly responds to active inflammation. A normal CRP level practically excludes the diagnosis of appendicitis, but an increase in its level is not specific for appendicitis. The test is especially reliable in combination with determining the level of leukocytes.
- General urine analysis. This is done to rule out urinary tract infections and kidney stones.
- Determination of hCG level. The study is prescribed to women to exclude ectopic pregnancy.
To exclude diseases of the liver and pancreas, the following tests are performed:
- aspartate aminotransf
Symptoms of the disease
The symptoms of acute appendicitis are pronounced, so primary diagnosis is not difficult. The attack begins suddenly, often at night or early in the morning. The pain is concentrated in the navel area and above the navel or spreads throughout the abdomen. A few hours after the onset of the attack, the pain shifts to the right side, to the iliac region (Kocher-Wolkovich syndrome).
The intensity of the pain increases, the patient rushes about, cannot find a position to reduce the pain. Minor relief occurs when you turn over on your right side and bend your knees as close to your stomach as possible. If the appendix is located atypically, the patient feels pain in the lumbar region, on the left side, in the groin. As a rule, the abdominal wall is tense.
If the pain goes away, this does not mean that independent healing has occurred. The tissues of the appendix die, the pain goes away, and a feeling of recovery is created. It is necessary to consult a doctor as soon as possible after the onset of the attack, otherwise peritonitis is highly likely to develop.
Pay attention to symptoms of acute appendicitis such as stool disorders, dry mouth, constant nausea, loss of appetite, weakness, malaise, low-grade fever, and changes in blood pressure. The appearance of a temperature above 38 degrees against the background of dull or acute pain in the abdomen is a dangerous symptom!
In older people, symptoms often appear vaguely. These are discomfort in the abdomen, weakness, minor pain and nausea. Such signs are characteristic of many chronic diseases, so patients are in no hurry to see a doctor. Under no circumstances should you take painkillers and put off calling a doctor at home, since every day without medical care greatly increases the risk of developing peritonitis.
Children under 5 years of age often easily tolerate an attack. Acute appendicitis can be suspected by a suddenly rising temperature, the development of diarrhea, and the appearance of plaque on the tongue. It is better to play it safe and call a doctor when the first symptoms appear to prevent the development of extremely dangerous complications.
Symptoms of appendicitis

The appendix is located in the lower abdomen. The first symptom is unbearable pain that appears in the navel area and spreads to the lower right side of the abdomen. The pain worsens over a short period of time when moving, taking a deep breath, coughing or sneezing.
Other typical symptoms:
- nausea, even vomiting
- decreased or complete lack of appetite
- constipation or, conversely, diarrhea
- flatulence, painful bloating
- fever, chills, symptoms of intoxication
- urge to defecate
Signs of inflammation of the appendix may differ in men and women. For example, women experience nausea, vomiting and fever. At the beginning of the development of the disease, the pain is pressing, pulling, and not even necessarily on the right side, which can be mistakenly recognized as gynecological problems.
Then the pain may become cramping, such symptoms most often occur in the evening or at night.
In men with acute inflammation, severe pain in the abdominal area and spontaneous tightening of the right testicle occur. When the scrotum is pulled back, discomfort and pain occur in the anal area and a strong urge to have a bowel movement.
In older people, the symptoms of appendicitis may appear less clearly: minor pain, mild nausea. At the same time, appendicitis in older people is often characterized by a severe course and the development of complications.
In children under 5 years of age, the symptoms of appendicitis are not as pronounced as in adults. The pain often has no clear localization. Appendicitis in a small child can be recognized by increased body temperature, diarrhea and the presence of plaque on the tongue.
Appendicitis in women during pregnancy
Appendicitis is a particular danger for pregnant women. Due to the fact that the appendix is located in close proximity to the uterine appendages, the signs of its inflammation coincide with the symptoms of diseases of the reproductive system.
Warning signs indicating appendicitis are painful palpation in the area below the navel, increased temperature, and shooting pain in the groin area. It is necessary to conduct an examination in a hospital to make a correct diagnosis and prevent complications of appendicitis.
What can appendicitis in children be confused with?
Mesenteric lymphadenitis
- enlarged lymph nodes;
- thickening of the walls of the small intestine with a small amount of free fluid between the intestinal loops and in the pouch of Douglas.
Crohn's disease
- usually a typical medical history;
— clinical course;
- predisposition to development in the final sections of the ileum.
Lymphoma
- may occur as a primary lesion of the intestinal wall (MALT lymphoma);
- enlargement of mesenteric and retroperitoneal lymph nodes.
Torsion of ovarian
- hemorrhage and typical sedimentation may occur;
- located next to the uterine appendages;
- The intestines are usually normal.
Intussusception
— typical ultrasound morphology and clinical features.
Inflammation of Meckel's diverticulum
- clinically indistinguishable;
- usually not detected during ultrasound scanning when covered with gas.
Diagnosis of the disease
Primary data - examination, questioning of the patient, palpation of the abdomen. The doctor, based on the symptoms and clinical picture, decides on the need for additional studies, which include ultrasound of the abdominal organs, CT, MRI. Laboratory tests of blood and urine are mandatory, and in addition - a stool test for helminths and a coprogram.
If there are symptoms of catarrhal appendicitis in young and middle-aged patients, tests reveal leukocytosis, increased levels of neutrophils and the level of C-reactive protein. This triad is not always detected in children and the elderly.
Acute appendicitis is similar in symptoms to diseases such as pancreatitis, perforation of gastric and duodenal ulcers, acute adnexitis, ectopic pregnancy, ovarian apoplexy (in women), renal colic, acute cholecystitis. It is necessary to carry out emergency differentiation of the diagnosis, since all of these pathologies can lead to life-threatening complications.
The appendix is a vermiform appendix of the cecum, which is located almost on the border between the small and large intestines.
Many rodents, some predators, monkeys and, of course, humans have a vermiform appendage in their bodies. The length of the human appendix is on average 5 - 15 cm, diameter - about 1 cm. Presumably, its main task is to protect the small intestine from bacteria inhabiting the cecum.
Appendicitis is an inflammation of the appendix. This disease is extremely common and requires emergency surgery.
Appendicitis can happen to anyone; the disease does not depend on age.
Symptoms of appendicitis
Clinical manifestations of acute appendicitis depend on the nature of the morphological changes in the appendix, its location, the age of the patients, and the nature of the associated complications. The initial symptom of the disease is a sudden dull pain without clear localization in the upper abdomen or navel area. After A-6 hours (with fluctuations from 1 to 12 hours), the pain moves to the right iliac region. A change in the localization of pain with the appearance of soreness in the right iliac region indicates the alarming appearance of somatic pain caused by irritation of the visceral peritoneum (i.e., inflammation has captured all layers of the wall of the appendix). The localization of pain depends on the location of the appendix: in a typical position the patient feels pain in the right iliac region, in a high position - almost in the right hypochondrium, in a retrocecal position - on the lateral surface of the abdomen or in the lumbar region, in a pelvic position - above the pubis. Nausea is a common symptom of acute appendicitis; sometimes, especially at the beginning of the disease, vomiting is possible. The stool is usually normal. When the appendage is located near the cecum or rectum or among loops of the small intestine, inflammation can spread to the intestinal wall, leading to fluid accumulation in the intestinal lumen and diarrhea.
The tongue at the first stage of the disease is moist, often covered with a white coating. Free lies on the back or right side; changes in body position, coughing, laughing, sneezing sharply increase abdominal pain. When examining the abdomen, there may be a lag in the right lower quadrant of the abdominal wall during breathing. On palpation, muscle tension and sharp pain in the right iliac region are detected. Positive symptoms of peritoneal irritation (Shchetkin-Blumberg, Razdolsky, Voskresensky symptom) can also be detected here. There are no pathognomonic symptoms of acute appendicitis; all symptoms are caused by the phenomena of local peritonitis. Pain, as a rule, intensifies when the patient is positioned on the left side (Sitkovsky's symptom), especially during palpation (Barthomier-Mikhelson's symptom). With a retrocecal location of the process, there may be a positive Obraztsov’s sign—increased pain when raising the straightened right leg. This symptom should be checked very carefully, since with rough pressure on the abdominal wall, perforation of the appendix is possible. The temperature is often elevated. In the blood - leukocytosis with a shift of the formula to the left. During a digital examination of the rectum or vaginal examination, pain is noted on palpation of the right wall of the pelvis (especially when the process is in the pelvic position). The presence of red blood cells and white blood cells in the urine does not exclude acute appendicitis.
The diagnosis of acute appendicitis in typical cases is simple, but the atypical location and peculiarities of the course of the inflammatory process sometimes make diagnosing the disease extremely difficult. Differential diagnosis is carried out with pyelitis, renal colic (see Urolithiasis), acute adnexitis, ectopic pregnancy, acute enteritis, mesadenitis, diverticulitis, acute cholecystitis, acute pancreatitis, perforated gastric and duodenal ulcers, right-sided pneumonia, herpes zoster, etc. acute simple and destructive appendicitis. In the latter case, the symptoms of acute appendicitis are more pronounced: pain is stronger, symptoms of peritoneal irritation are more clear, leukocytosis and temperature are higher. However, complete correspondence of the clinical picture of the disease with the nature of the detected morphological changes in the appendix is still not observed.
The course of acute appendicitis in different age groups and pregnant women has its own characteristics. In children, underdevelopment of the greater omentum and the body's hyperergic reaction lead to rapid progression of the inflammatory process and the development of peritonitis. Diagnosis of acute appendicitis in children in the initial stage of the disease is difficult: nausea, repeated vomiting, high fever, diffuse abdominal pain, and therefore diagnostic errors are often made. In older people, a decrease in the body's reactivity causes the clinical symptoms of the disease to fade, which can be a reason for delayed diagnosis and hospitalization. Hence the prevalence of destructive forms of acute appendicitis and often appendiceal infiltrates. In pregnant women, displacement of the dome of the cecum and the appendix by the uterus leads to a change in the typical localization of pain, and the location of the appendix behind the uterus leads to a decrease in the severity of peritoneal symptoms.
Treatment of appendicitis
Treatment is surgical. The operation is indicated not only in every clear case from a diagnostic point of view, but also in cases of reasonable suspicion of acute appendicitis, if it is impossible to exclude acute inflammation of the appendix based on clinical signs and special research methods (including laparoscopy). If signs of peritonitis are pronounced, it is advisable to administer antibiotics (aminoglycosides) and metronidazole before surgery. In thin, young patients, appendectomy is usually performed under local anesthesia with a 0.25-0.5% novocaine solution. In case of severe pain syndrome in patients with unstable psyche, children, pregnant women, elderly and senile patients, preference is given to general anesthesia.
Treatment methods
The main method of treatment is surgical removal of the appendix. The conservative method is used extremely rarely, in the presence of absolute contraindications to surgical intervention. Medications are also prescribed for sluggish progress of the process, with rare, implicit exacerbations.
The operation is performed using a traditional and minimally invasive (laparoscopic) method. Classic surgery provides open access to the surgical field (an incision in the abdominal wall). Laparoscopic surgery is performed using a special device with a video camera, inserted into the cavity through a small incision.
This is a low-traumatic intervention that avoids blood loss and also reduces the risk of internal infections and other complications. Antibiotics are prescribed before and after surgery. The method of surgery for acute appendicitis depends on the patient’s health status, the clinic’s capabilities, and the type of appendicitis (standard, complicated).
Complications of appendicitis
The most dangerous complication of the disease is a ruptured appendix with signs of suppuration. In this case, all dead tissue and purulent contents of the appendix enter directly into the abdominal cavity. Intoxication and a condition that threatens the patient’s life rapidly develops. All organs of the abdominal cavity are affected, the infection penetrates the tissues and fluids of the body. The patient rushes about, experiences a dull pain in the abdomen, the temperature rises, the heart rhythm is disturbed, and nausea and vomiting intensify.
The first symptom of peritonitis is the spread of pain to all parts of the abdomen, increasing weakness, lethargy, and drowsiness. After some time, the pain may go away, which creates the illusion of recovery. On palpation, abdominal distension is noted.
In the absence of emergency medical care (surgery), symptoms of intoxication increase: vomiting increases, headache, shortness of breath appear, and the functioning of the excretory system is disrupted.
It is possible to cope with peritonitis only in the first stages of the development of a dangerous process. Surgeons perform a classic operation to remove the appendix and purulent contents from the abdominal cavity. The operation to sanitation the abdominal organs lasts several hours. In the future, the patient is prescribed combination antibacterial therapy using strong antibiotics and detoxification drugs.
However, even successful and correct actions of surgeons are not able to prevent further complications caused by peritonitis. These include:
- septic lesions of the pelvic organs;
- renal and liver failure;
- formation of adhesions;
- infertility (in women).
Due to massive antibacterial therapy, immunity is reduced, intestinal microflora is disrupted, and vulnerability to all infectious diseases increases.
The most dangerous complication of peritonitis resulting from a ruptured appendix is pyelphlebitis, which is acute inflammation and suppuration of the portal vein. Due to the rapid development of sepsis in tissues and body fluids, death occurs in most cases.
What is the appendix and appendicitis and why is the disease difficult to diagnose?
The content of the article
The appendix, the vermiform appendage of the cecum, is an organ of variable size and location. You can roughly determine where the appendix is by drawing 2 imaginary lines:
- horizontally, from the navel to the right;
- vertically, from the right breast nipple down.
The lower right corner formed by the crosshairs of these lines is the right iliac region - the most likely location of the appendix. Due to the long mesentery, the appendix is easily displaced, therefore, where exactly the appendix is located is determined by ultrasound of the abdominal cavity.
Inflammation of the appendix is called appendicitis. The disease is characterized by the variety and complexity of symptoms. Abdominal pain associated with appendicitis is typically similar to symptoms of other abdominal and pelvic conditions, including diverticulitis, ovarian mass, ectopic pregnancy, and even kidney stones.
Every year, about 300 thousand operations to remove the appendix turn out to be erroneous due to a false diagnosis.
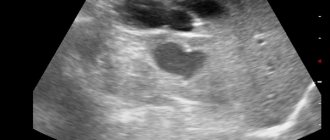
It is especially difficult to diagnose appendicitis in the initial stages, when the pain is not strictly localized and the symptoms are too vague, and in chronic forms - only ultrasound helps here. You can independently guess that appendicitis has begun only when the pain has already reached its peak and the operation may go beyond a simple one.
Prevention of appendicitis
There is no specific prevention of appendicitis, but a healthy lifestyle and proper nutrition help avoid the development of any unwanted processes in the organs of the digestive system. You should eat according to a schedule, at approximately the same hours, and avoid overeating. Smoking and drinking alcohol are incompatible with a healthy lifestyle. It is necessary to consume as many plant-based foods rich in fiber as possible and reduce the proportion of animal proteins in the daily diet.
If warning symptoms appear (sudden abdominal pain, weakness, feeling of fear), call emergency services. The doctor will quickly identify appendicitis based on the symptoms and refer you for an emergency examination. It is very important to prevent complications of the pathology, which take a long time to treat and are not always successful. Monitor your health, pay attention to any unusual symptoms, and do not delay visiting a doctor.
Removal of the appendix by laparoscopic method is the best option for treating the pathology. Recovery occurs quickly, without complications, and a barely noticeable scar remains on the body, which completely resolves over the years.