What is pneumonia?
Pneumonia, popularly called “pneumonia,” is damage to the lung tissue. Depending on the stage of the disease, it can affect the lining of the lung and various parts, including the diaphragmatic pleura. Pneumonia is a very dangerous disease, often leading to death, so if there are signs of the disease, doctors prescribe an x-ray.
Causes of the disease
In most cases, pneumonia occurs due to harmful microorganisms entering the organ: viruses, bacteria, fungi. Infection occurs by airborne droplets. Another type, eosinophilic pneumonia, is allergic in nature and requires urgent X-ray examination. Much less often, pneumonia is congestive, for example, when it occurs as a result of prolonged bed rest. It can also be a complication of other diseases. What pneumonia looks like on an X-ray largely depends on the nature and stage of the disease.
Signs of illness
Symptoms of pneumonia do not take long to appear, manifested by a dry or wet cough, with a temperature of up to 40 degrees. With a wet cough, the doctor pays attention to the nature of the sputum: “rusty”, bloody with pus, the presence or absence of odor. Other signs of pneumonia include pain in the chest, side, and even stomach—in this case, an x-ray is needed to confirm the location of the lesions in the lung.
Chronic obstructive pulmonary disease (COPD) - symptoms and treatment
If patients have cough, sputum production, shortness of breath, and risk factors for developing chronic obstructive pulmonary disease have been identified, then they should all be diagnosed with COPD.
In order to establish a diagnosis, clinical examination (complaints, anamnesis, physical examination) are taken into account.
A physical examination may reveal symptoms characteristic of long-term bronchitis: “watch glasses” and/or “drumsticks” (deformation of the fingers), tachypnea (rapid breathing) and shortness of breath, changes in the shape of the chest (emphysema is characterized by a barrel-shaped shape), small its mobility during breathing, retraction of the intercostal spaces with the development of respiratory failure, drooping of the borders of the lungs, change in percussion sound to a box sound, weakened vesicular breathing or dry wheezing, which intensifies with forced exhalation (that is, rapid exhalation after a deep inhalation). Heart sounds may be difficult to hear. In later stages, diffuse cyanosis, severe shortness of breath, and peripheral edema may occur. For convenience, the disease is divided into two clinical forms: emphysematous and bronchitis. Although in practical medicine, cases of a mixed form of the disease are more common.
The most important stage in diagnosing COPD is an analysis of pulmonary function (PRF) . It is necessary not only to determine the diagnosis, but also to establish the severity of the disease, draw up an individual treatment plan, determine the effectiveness of therapy, clarify the prognosis of the course of the disease and assess the ability to work. Establishing the percentage ratio of FEV1/FVC is most often used in medical practice. A decrease in the volume of forced expiration in the first second to the forced vital capacity of the lungs FEV1/FVC to 70% is the initial sign of airflow limitation even when FEV1>80% of the proper value is preserved. A low peak expiratory air flow rate, which varies slightly with the use of bronchodilators, also speaks in favor of COPD. For newly diagnosed complaints and changes in respiratory function indicators, spirometry is repeated throughout the year. Obstruction is defined as chronic if it occurs at least 3 times per year (despite treatment), and COPD is diagnosed.
Monitoring FEV 1 is an important method to confirm the diagnosis. Spireometric measurement of FEV1 is carried out repeatedly over several years. The rate of annual decline in FEV1 for mature adults is within 30 ml per year. For patients with COPD, a typical indicator of such a drop is 50 ml per year or more.
A bronchodilator test is a primary examination during which the maximum FEV1 value is determined, the stage and severity of COPD is established, and bronchial asthma is excluded (if the result is positive), the tactics and volume of treatment are selected, the effectiveness of therapy is assessed and the course of the disease is predicted. It is very important to distinguish COPD from bronchial asthma, since these common diseases have the same clinical manifestation - broncho-obstructive syndrome. However, the approach to treating one disease is different from another. The main distinguishing feature in diagnosis is the reversibility of bronchial obstruction, which is a characteristic feature of bronchial asthma. It has been found that in people diagnosed with COPD after taking a bronchodilator, the percentage increase in FEV1 is less than 12% of the initial value (or ≤200 ml), and in patients with bronchial asthma it usually exceeds 15%.
Chest X-ray is of auxiliary value, since changes appear only in the later stages of the disease.
An ECG can detect changes that are characteristic of cor pulmonale.
Echocardiography is necessary to identify symptoms of pulmonary hypertension and changes in the right heart.
Complete blood count - it can be used to evaluate hemoglobin and hematocrit (may be elevated due to erythrocytosis).
Determination of the level of oxygen in the blood (SpO2) - pulse oximetry, a non-invasive test to clarify the severity of respiratory failure, usually in patients with severe bronchial obstruction.
Blood oxygen saturation less than 88%, determined at rest, indicates severe hypoxemia and the need for oxygen therapy.
How is an x-ray taken for pneumonia?
For pneumonia, an X-ray of the lungs is usually taken, regardless of the cause of the disease. Before the study, it is necessary to remove everything that could distort the results: metal objects, jewelry, long hair, etc. X-ray of the lungs
done in a vertical position, having first undressed to the waist and stood in front of the machine as the radiologist says. At the doctor’s command, the patient draws air into his lungs and holds his breath, while the device takes a picture.
CT scan after coronavirus
Repeated tomography is prescribed both to monitor the current disease and to assess the condition of the lungs during the period of their recovery.

If treatment does not lead to symptom relief, secondary screening is prescribed on the third day of enhanced therapy, and then another week later. If the treatment gives results, during the rehabilitation process a repeat CT scan is done after 2-3 weeks, helping to track the dynamics of tissue regeneration. With a favorable course, complete recovery is observed after a month; a complicated form leads to the formation of fibrosis - scars in the lungs, which also require monitoring. The advisability of repeated tomography sessions is determined by the attending physician, but it is not recommended to exceed the number of screenings allowed per year - 5 CT scans.
What does pneumonia look like on an x-ray?
What pneumonia looks like on an X-ray depends on the stage of the disease and its nature. However, in any case, signs of pneumonia on x-ray are visible as disturbances in the structure of the lung. Doctors pay attention to the features of the pulmonary pattern, the roots of the lung, the pleura and the location of infiltrative foci. Light areas in the image are interpreted as airless.
Krupoznaya
Croupous pneumonia on X-ray is characterized by increased pulmonary pattern and thickening of the root, slight compaction of the pleura, as well as reduced airiness of the lung. The reduction in airiness directly depends on the stage of the disease. This disease looks like medium-intensity shading. Lobar pneumonia is one of the most dangerous.
Focal
As with lobar pneumonia, with focal pneumonia, X-rays show an increase in the pulmonary pattern and thickening of the root, as well as thickening of the pleura. Such pneumonia is characterized by focal shadows of different sizes with unclear contours. There is also a deformation of the pulmonary pattern, which is very clearly visible on x-ray. It is difficult to identify symptoms of focal pneumonia on X-rays, so only an experienced doctor can diagnose this disease.
Viral
Viral pneumonia is classified as atypical. With the strengthening of the pulmonary pattern and compaction of the pleura in this case, the roots of the lungs do not change. The appearance on x-ray of focal shadows in the lower and middle parts of the lungs with bilateral viral pneumonia confirms the diagnosis. The whole world is aware of the rapid development and danger of this form of the disease, and this is another argument in favor of examining the signs of pneumonia on an X-ray.
Typical CT manifestations of viral pneumonia (including COVID-19)
Numerous compactions of the lung tissue of the “frosted glass” type, predominantly round in shape, of varying length with or without consolidation, are localized, for the most part, in the peripheral, cortical sections, multilobar. The lesion is often bilateral (currently only isolated cases of unilateral lesions have been described).
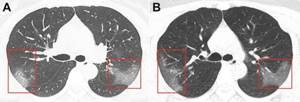
Foci of lung damage in COVID-19
Additional signs include:
- thickening of the interlobular interstitium like a “cobblestone pavement” (eng. “crazy-paving” sign)
- consolidation areas
- perilobular seals
- air bronchogram symptom
These signs are mainly determined on days 5–12 of the disease.
Manifestations that are not typical for SARS COVID-19 on a CT scan of the OGK:
- consolidation of lung tissue of the “frosted glass” type in the central and hilar localization
- single solid nodules
- presence of cavitations
- pleural effusion
- lymphadenopathy
- focal dissemination
- tree in the buds symptom
- pneumosclerosis/pneumofibrosis.
Contraindications to X-rays
X-rays should not be taken for pregnant women at any stage, as well as for children under 15 years of age. In some cases, the patient's condition may be an obstacle to conducting the study. A patient in a supine position cannot undergo the study due to the inability to assume an upright position. In an inadequate condition, when the patient cannot stand still, signs of pneumonia on an x-ray cannot be recorded properly.
How often can an x-ray be taken for pneumonia?
A confirmed diagnosis is an indication for regular x-ray examinations to monitor the course of the disease. Whether the treatment prescribed by the doctor helps will show what pneumonia looks like on an x-ray. In this regard, many patients are concerned about how often this procedure can be performed without harm to health. After the start of treatment, depending on the type of disease, an x-ray for pneumonia must be done after 6-10 days. If positive dynamics are noticed, treatment continues as it was started. The patient, who is considered to be cured, is subsequently re-examined after 1, 3 and 6 months. With favorable treatment, the patient receives a small dose of radiation, far from acceptable levels. This is possible thanks to the development of medical technologies and protective measures during the procedure.
Clinical case
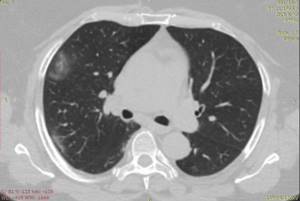
The patient developed a cough with mucous sputum, loss of taste and abdominal pain due to a rise in temperature to 38.5 within 5 days, weakness and sweating. On CT of the OGK in the cortical layer of the lungs, mainly in their posterior-basal sections, different-sized areas of compaction of the “ground glass” type and consolidation are determined, some of them are fused with the thickened costal and posterior mediastinal pleura. There is a minimal amount of fluid in the pleural cavities. No intrathoracic lymphadenopathy was detected. The volume of the affected lung parenchyma does not exceed 25%. The presence of areas of consolidation correlates with severe clinical symptoms and the addition of cough with sputum.
Lednev A.G.