The doctor prescribes a biopsy of the cervix if during a gynecological examination he notices suspicious changes in the tissues of the cervix. This small procedure allows you to determine whether these changes are benign or malignant. In this process, a piece of tissue is plucked from the surface of the cervix, which is sent for laboratory testing. A cervical biopsy is needed to detect cancer in the early stages or other pathologies that may later develop into cancer.
About the organ
The uterus is a hollow inside, female unpaired organ consisting of muscle tissue, located in the middle part of the pelvic cavity.
The organ is capable of significantly increasing in size during fetal development, and after childbirth it can return to its previous size within a couple of weeks.
Like other organs, the uterus can be subject to various pathologies. They can also cause dangerous complications. Therefore, it is important to regularly visit a gynecologist for preventive purposes.
It's sad, but statistics show that improving medical technology does not reduce the number of patients. Doctors at the Onco.Rehab integrative oncology clinic often encounter cases of advanced forms of cancer due to late detection of the disease, but treating the disease in its initial stages is a significant guarantee of successfully getting rid of the problem.
Discharge after cervical biopsy
What consequences does a cervical biopsy have for a woman? The most unpleasant thing is bloody discharge that appears due to a violation of the integrity of the mucous membrane. The discharge may be accompanied by aching pain in the lower abdomen. But these are completely acceptable consequences, and they are considered normal for such a procedure. A woman should only worry if the discharge does not stop after a few days, but, on the contrary, intensifies, and if it has an unpleasant odor, which indicates the presence of an infection. To avoid such complications, as well as uterine bleeding, a woman must follow several rules after a cervical biopsy. You cannot take a hot bath, visit a bathhouse or sauna, sunbathe in the sun, you must refrain from sexual intercourse until the mucous membranes heal, do not lift heavy objects, and avoid strenuous physical exertion. If no complications arise during the rehabilitation period, then recovery occurs within a week, and the woman can easily return to her usual lifestyle and previous activities.
Primary appointment with an obstetrician-gynecologist: 2200 RUR.
Sign up Online 5% discount when registering from the site
About the method
A variety of diseases can lead to the occurrence of uterine oncology. If a malignant tumor is suspected or detected, a biopsy is prescribed.
A biopsy of the uterus, or endometrium, is a procedure in which a sample of material is taken from the inner surface of the organ for further study. They do this to clarify existing assumptions about the disease and establish an accurate diagnosis.
The starting point of a uterine biopsy is the diagnosis of a pathological process in the organ.
As a method, biopsy is very informative; its accuracy is almost 100%.
The procedure is minimally invasive and is performed on an outpatient basis. The use of anesthesia depends on the method chosen.
Contraindications
There are not many contraindications for cervical biopsy. These are mainly poor blood clotting, inflammation of the cervix or vagina, and sexually transmitted infections (STIs).
A biopsy, although small, is still a surgical intervention, which in rare cases can lead to uterine bleeding, so it is not indicated for patients with poor blood clotting. This complication can occur due to the fact that there are many blood vessels in the cervix, and with poor clotting, they begin to bleed heavily. Women who do not have this pathology are not in danger during a cervical biopsy.
But diseases in which the blood does not clot well are quite rare, but sexually transmitted infections are a very common reason for canceling a biopsy. Therefore, before the procedure, the doctor must prescribe tests for the presence of STIs. This includes a smear and blood test. If sexually transmitted diseases such as gonorrhea, syphilis, trichomoniasis, chlamydia, etc. are detected, the biopsy is postponed until the patient has completed the necessary course of treatment and recovered. The same applies to inflammatory processes in the vagina and cervix. Such precautions are due to the fact that during the procedure the mucous membrane of the cervix is damaged, and there is a risk of infection in the wound, and this can already cause serious pathology.
Indications
A uterine biopsy is indicated in a number of cases:
- Bleeding in premenopause;
- Bleeding in menopause;
- Bloody discharge while taking hormones;
- Failure of the menstrual cycle;
- Infertility;
- Suspicion of hyperplasia, polyps
- Version of the formation of a malignant tumor.
In addition to the above, the procedure is indicated for certain diseases, including:
- Uterine fibroids;
- Chronic endometritis.
Biopsy of a lymph node in the neck for cancer
A uterine biopsy is prescribed to monitor the condition of the endometrium after hormone treatment.
What happens after a colposcopy?
You will probably have no problems after the colposcopy and biopsy. If your results show any problems, your doctor may suggest additional tests or treatment.
What should I do after the colposcopy procedure?
After a colposcopy, your vagina may feel slightly sore for a few days. If you have had a biopsy, you may also have a dark-colored vaginal discharge. Use a sanitary pad, it is not recommended to take a bath for 2 weeks (only hygienic shower).
Here are some other things to keep in mind after a colposcopy and biopsy:
- You can take a shower whenever you want.
- If you have not had a biopsy, you can have vaginal sex at any time.
- If you have had a biopsy, wait about 3 days before having vaginal sex. This allows the cervix to heal.
- If you are taking any medications, continue to take them as usual, including birth control.
Types of procedure
There are several types of uterine biopsies.
- Curettage. It is considered a classic method. Performed under local anesthesia or general anesthesia. During the procedure, the cervical canal is opened by scraping the cervical canal and its cavity. A curette is used for this.
- Curettage in the form of trains (line scrapings). A small curette is used to collect material from the fundus of the uterus to the cervical canal. This should not be done if there is uterine bleeding.
- Aspiration biopsy. Performed by suctioning areas of the mucous membrane. You may experience some discomfort while doing this. If a malignant tumor in the body of the uterus is suspected, the procedure is not used: the information content is close to zero.
- Pipelle biopsy of the endometrium. The method is modern, painless and safe. The material is collected using a pipel, a special soft tube with a piston inside. By inserting the pipe into the uterine cavity with the piston extended halfway, negative pressure is obtained in the cylinder. There is an effect of absorption of endometrial tissue inside. Important features of the procedure are that it lasts several minutes and does not require dilation of the cervical canal due to the small diameter of the pipe.
Indications for cervical biopsy
The gynecologist prescribes tissue sampling for biopsy for any abnormalities on the cervix that he discovers during an examination or colposcopy. Such changes include:
- cervical erosion;
- papillomas, polyps;
- the presence of areas on the mucous membrane with discoloration, which appear under the influence of special solutions used during colposcopy;
- poor smear cytology result.
If you need to confirm some diagnoses, such as endocervicitis, cervical dysplasia, leukoplakia, a biopsy is also required. If the smear contains papillomavirus and other sexually transmitted diseases, a cervical biopsy is also taken, since these viruses can cause cervical cancer.
When to carry out
The doctor determines the time of the uterine biopsy, guided by the most favorable days of the menstrual cycle. They differ for different diseases, for example:
- Infertility – at the very beginning of menstruation or before it;
- Heavy menstrual bleeding – on days 5–10 of the cycle;
- Absence of menstruation and absence of pregnancy - repeated procedures are carried out for 3 - 4 weeks with breaks of 1 week;
- Acyclic bleeding - after the onset of blood smearing, bleeding;
- Suspicion of cancer of the mucosal layer - any day of the cycle.
Cervical biopsy methods
There are several ways to perform a cervical biopsy. Usually, local anesthesia is used during the procedure, but some women tolerate it quite well without anesthesia. In rare cases, general anesthesia may be performed.
The most common method is a biopsy done with a scalpel. This method also gives the most reliable results. First, the cervix is exposed with special instruments, then a solution is injected that colors it and highlights pathological areas. Then one of these lesions is carefully excised - this is the material for histological examination.
Currently, cervical biopsy performed using a laser or alternating current is becoming increasingly popular. This method is considered less invasive, but has one drawback: it may damage the tissue taken for histology, which will significantly affect the results of the analysis. And the main advantage is that there is no bleeding and after the biopsy, no sutures or adhesions form on the neck. This moment is very important for those women who have yet to give birth.
The attending gynecologist decides exactly how the cervical biopsy will be performed. To do this, he takes into account all factors: the woman’s age, chronic diseases, features of the physiological state, the size of the mucosal lesion, etc. In most cases, the procedure is carried out directly in the gynecological office, but some types of biopsy may require a stay in the hospital for a couple of days.
results
As a result of the procedure and the subsequent histological examination, the doctor may discover:
- Structural changes of various kinds, for example, cysts;
- Papillomatosis;
- Endometriosis;
- Inflammatory processes;
- The tumors are benign;
- Oncological cells.
It is important to be confident in your health, and for this you need to follow preventive measures and carry out diagnostics.
The Onco.Rehab clinic has trusted partners who, using the best global experience and the latest technological developments, will safely perform the biopsy procedure.
What should I do if my colposcopy results are not normal?
If your doctor finds abnormal cells, you may not need to do anything right now. Sometimes more tests or treatment will be needed. It depends on how abnormal the cells in your cervix are.
Your doctor may recommend waiting to see if the cells repair themselves. In this case, you will have another Pap test and possibly other tests to monitor the cells.
Sometimes a biopsy is also your treatment. This is because your doctor can remove all the abnormal cells during a biopsy. If this is the case, you will no longer need treatment. You will return to regular pelvic exams, Pap tests, and/or HPV tests. Your doctor will tell you how often you should take them.
Or you may need further treatment. There are 4 procedures that are very good at removing abnormal cells and preventing cervical cancer.
- Cryotherapy : abnormal cells are frozen
- LEEP : Abnormal cells are removed using a thin wire loop that conducts an electrical current
- Laser : Abnormal cells are removed using laser
- Cone biopsy : a cone-shaped wedge is cut from the cervix to remove abnormal cells
Regardless of what treatment you receive, it is important to continue to have regular pelvic examinations after you have been treated for abnormal cells. Although these procedures are very effective, sometimes abnormal cells return.
Diagnostic methods in gynecology: pipell biopsy
Aspiration biopsy of the endometrium (pipe biopsy): how it is performed, indications.
Previously, for some gynecological diseases, only traumatic biopsy techniques of the uterine mucosa were used to collect endometrial samples, which involved curettage (i.e., a procedure similar to a classic surgical abortion). However, thanks to the advent of aspiration biopsy (or Pipelle biopsy), such an examination has become more painless and safe.
How is the Pipel test carried out:
This minimally invasive surgical technique for collecting endometrial tissue is carried out using a special plastic tube - pipel - during an examination in a gynecological chair, but first, the doctor cleans the surface of the cervix from secretions using a cotton swab. The thickness of the pipe is 3 mm, and its operating principle is similar to the syringe mechanism. There is a piston inside the tube, and at one end there is a side hole for entry by aspiration of the endometrium into the tip of the pipel.
Unlike the classical surgical method of collecting endometrial tissue, aspiration biopsy does not require dilation of the cervical canal. The tip of a disposable tube is inserted into the uterine cavity without the use of additional devices. The doctor pulls the piston toward himself, creating negative pressure for the necessary aspiration of a small area of the endometrium. At the same time, extensive wound surfaces do not form on the inner layer of the uterus, the cervix does not suffer from mechanical stress, and the patient does not experience pronounced discomfort.
Indications:
Indications for this study are pathological processes localized in the endometrium - the inner layer of the uterus.
An aspiration biopsy is prescribed in cases where, after a gynecological examination and ultrasound, the doctor suspects that the patient has pathological changes in the condition of the inner layer of the uterus - the endometrium. The obtained tissue samples make it possible to conduct a histological analysis of the mucous layer of the uterus and make a correct diagnosis.
Endometrial aspiration biopsy is prescribed in the following clinical cases:
- endometrial hyperplasia;
- menstrual irregularities (acyclic scanty bleeding, menometrorrhagia, scanty periods, amenorrhea of unknown origin);
- endometriosis;
- chronic endometritis;
- polyps in the body of the uterus;
- suspicion of infertility;
- heavy bleeding in women during menopause;
- suspicion of the presence of a benign or malignant tumor (uterine fibroids, endometrial cancer).
Pipelle biopsy can be performed not only to diagnose endometrial pathologies, but also to evaluate the effectiveness of hormone therapy.
Contraindications:
Endometrial aspiration biopsy cannot be performed in the following cases:
- inflammatory diseases of the genitourinary system in the acute phase;
- pregnancy.
Possible limitations for performing Pipelle biopsy include the following clinical cases:
- disorders of the blood coagulation system;
- severe forms of anemia;
- constant use of antiplatelet agents and anticoagulants (Clexane, Warfarin, Trental, non-steroidal anti-inflammatory drugs, etc.);
- individual intolerance to local anesthetics used.
If such conditions are detected, aspiration biopsy can be performed after special preparation of the patient or replaced with another study.
How to properly prepare for the procedure:
Although aspiration biopsy of the endometrium is a minimally invasive procedure, during it, instruments are inserted into the uterine cavity and damage to the integrity of the inner layer of this organ occurs, albeit minor. That is why, in order to exclude possible complications of such a study, the patient needs to properly prepare for the collection of material.
To exclude possible contraindications to endometrial aspiration biopsy, the following diagnostic studies must be performed:
- gynecological examination;
- microflora smear;
- cytological smear from the cervix (PAP test);
- Ultrasound of the pelvic organs;
- general blood analysis;
- blood test for hCG;
- blood test for hepatitis B and C, syphilis and HIV;
- colposcopy (preferred).
When prescribing a Pipelle biopsy, the doctor must obtain from the patient all the information about the medications she is taking. Particular attention is paid to taking blood thinners (Clopidogrel, Aspirin, Warfarin, etc.). If necessary, the doctor can change the order in which they are taken a few days before the procedure.
When prescribing endometrial aspiration biopsy, special attention is paid to choosing the date of the study. If a woman has not yet entered menopause, the timing of the procedure depends on the day of the menstrual cycle. If the patient is no longer menstruating, tissue sampling is performed depending on the onset of abnormal uterine bleeding.
Typically, endometrial aspiration biopsy is performed on the following days:
- 18-24 days - to establish the phase of the cycle;
- on the first day in case of pathological bleeding - to identify the cause of bleeding;
- on days 5-10 of the cycle - with excessively heavy periods (polymenorrhea);
- on the first day of the cycle or the day before menstruation - if infertility is suspected;
- once a week – if pregnancy does not occur and there is no menstruation;
- on days 17-25 – to monitor the effectiveness of hormonal therapy;
- any day of the cycle – if the presence of a malignant neoplasm is suspected.
Direct preparation for Pipelle biopsy is carried out 3 days before the study. During these days, a woman must follow the following doctor’s recommendations:
- Refuse sexual intercourse.
- Do not douche, do not insert suppositories, ointments and creams into the vagina.
- Exclude from the menu foods that contribute to increased gas formation.
- In the evening before the study, perform a cleansing enema.
The endometrial aspiration biopsy procedure can be performed in a specially equipped office in a clinic. As a rule, it does not require the use of local anesthesia, but sometimes this method of pain relief is performed for particularly sensitive patients. In such cases, before conducting the study, the doctor must make sure that there is no allergic reaction to the drug used (based on medical history or a test performed).
How the procedure is carried out:
During the procedure, the patient is on a gynecological chair.
On the appointed day, the patient with a referral comes to the office for an aspiration biopsy. The procedure for collecting endometrial tissue is performed as follows:
- The woman lies down on the gynecological chair, and the doctor inserts a speculum into the vagina. If necessary, local anesthesia of the cervix is performed by irrigating it with a solution of local anesthetic.
- The pipel tip is inserted into the uterine cavity through the cervical canal.
- The gynecologist pulls back the piston, and negative pressure is created in the tube. As a result of this effect, part of the endometrium enters the pipel cavity. The doctor collects material from different areas.
- Once sufficient material has been obtained, tissue samples are sent to the laboratory for histological analysis.
- The pipel is removed from the uterine cavity. The duration of the procedure is 1-3 minutes.
The results of histological analysis of endometrial tissue are obtained 7-14 days after the biopsy. After assessing them, the gynecologist makes a diagnosis and draws up a plan for further examination and treatment.
After the procedure:
After performing an aspiration biopsy of the endometrium, the patient feels satisfactory and can go home. Her performance is not impaired in any way, and there is no need for hospitalization.
In the next 1-2 days, the patient may feel minor painful pulling sensations in the lower abdomen. To eliminate cramping pain, which causes significant inconvenience, a woman can take antispasmodics (No-shpa, Papaverine, Spazmalgon). As a rule, such discomfort does not last more than 1 day.
In the first few days after the aspiration biopsy procedure, women experience light, bloody discharge from the genital tract. Most experts recommend that their patients abstain from sexual intercourse during these days. After the bleeding stops, a woman can resume sexual activity and use barrier contraception to prevent pregnancy.
After the study, menstruation may occur on time or with some delay (up to 10 days). In such cases, the woman is advised to take a pregnancy test and visit a doctor.
After an aspiration biopsy, pregnancy can occur in the current or subsequent cycle. This method of endometrial sampling does not affect the functioning of the ovaries and the remaining area of the uterine mucosa is sufficient for implantation of the fertilized egg.
Possible complications:
The endometrial aspiration biopsy procedure is minimally invasive and in rare cases leads to complications. After the examination, the gynecologist must familiarize the patient with the symptoms, when they appear, she should immediately consult a doctor:
- increased body temperature;
- bleeding from the vagina (thick, bright red discharge);
- incessant pain in the lower abdomen;
- dizziness or fainting;
- convulsions.
Advantages of endometrial aspiration biopsy:
Pipelle biopsy has a number of significant advantages:
- low risk of injury to the walls of the uterus;
- there is no need to expand the cervical canal to insert instruments;
- the possibility of obtaining endometrial tissue from inaccessible areas of the uterine cavity;
- minimal risk of infection;
- minimal risk of complications;
- no pain during the procedure;
- rapid recovery of the patient after the biopsy;
- the ability to perform the study on an outpatient basis and there is no need for hospitalization of the patient;
- high information content;
- no negative impact on the body of a woman preparing for pregnancy (for example, before IVF);
- simple preparation for the procedure;
- low cost of research.
What will the result of histological analysis after aspiration biopsy show?
In the absence of pathological abnormalities in the structure of the mucous layer of the uterus, the analysis will indicate that the endometrium corresponds to the age norm and the phase of the menstrual cycle, and no signs of atypia were identified.
If deviations in the structure of the mucous layer of the uterus are detected, the following pathological changes may be indicated in the analysis results:
- adenomatosis (or complex endometrial hyperplasia);
- simple diffuse (or glandular, glandular-cystic) endometrial hyperplasia;
- local endometrial hyperplasia with or without atypia (or polyposis, single polyps);
- simple or complex atypical endometrial hyperplasia;
- endometrial hypoplasia or atrophy;
- endometritis;
- discrepancy between the thickness of the endometrium and the phase of the menstrual cycle;
- malignant degeneration of the endometrium.
Endometrial aspiration biopsy is often used as a screening method for examining patients with questionable ultrasound results. However, this method of collecting tissue from the inner layer of the uterus does not always allow obtaining a sufficient amount of material to completely exclude the presence of malignant tumors. That is why, if a cancerous process is suspected, the examination of the patient is supplemented with a more informative diagnostic curettage.
What to do after endometrial aspiration biopsy:
After performing a Pipelle biopsy, the doctor sets a date for the patient’s next visit. Typically, histological examination tests are ready 7-14 days after the procedure, and based on their results, the gynecologist can determine further tactics for diagnostic and therapeutic measures.
If signs of atypia or cancerous processes are detected, the doctor decides on the need for additional research and surgical treatment. If the results of histological analysis indicate the presence of inflammation, then the patient is prescribed antibiotic therapy and anti-inflammatory drugs.
When determining signs of hyperplasia or insufficient response of the endometrium to hormonal changes during the menstrual cycle, the doctor conducts additional diagnostic tests to identify endocrine disorders. After this, the patient may be prescribed hormone therapy, which improves the condition of the endometrium and restores reproductive function, taking other medications and physiotherapeutic procedures.
Which doctor should I contact:
A gynecologist can prescribe an endometrial aspiration biopsy. Before the study, the patient will need to undergo a series of diagnostic examinations to exclude contraindications: ultrasound, blood tests, microflora smear, PAP test, colposcopy. If necessary, after a Pipelle biopsy of the endometrium, other studies may be prescribed to clarify the diagnosis: blood tests for hormones, CT or MRI of the pelvic organs, diagnostic curettage, etc.
Endometrial aspiration biopsy is a minimally invasive, safe, painless and informative procedure, which in many cases makes it possible to make the correct diagnosis and makes it possible to refuse more traumatic examinations. Before performing it, the patient must undergo a series of diagnostic examinations to identify possible contraindications and follow simple doctor’s recommendations to ensure the safety and information content of the biopsy and histological analysis. The procedure itself takes no more than 1-3 minutes. Further diagnostic and treatment tactics are determined by the doctor after receiving the results of histological analysis.
Preparation and execution
At its core, a biopsy is a surgical intervention, albeit a very small one. Before the operation itself, the patient’s pathological flora is checked to ensure that there are no infectious diseases. If a disease is detected, it is first cured.
As for the time when the procedure can be prescribed, this is traditionally done after menstruation has ended. The patient officially and in writing confirms that she agrees to take a biopsy.
Since there are no nerve endings in the uterine cervix, as such, the biopsy procedure is not accompanied by pain. However, patients usually still expect something scary and therefore their muscles remain tense, including the muscles of the uterus. Even cramps are possible during the period, but even such unpleasant feelings are no more terrible than an ordinary tingling sensation in the lower abdomen during menstruation. Doctors sometimes avoid spasms by injecting lidocaine. However, this is not a mandatory action.
It is mandatory to stain the uterine cervix with Lugol's solution, before it is treated with acid. This trick will help distinguish healthy skin from diseased skin, since the coloring of healthy tissue does not present any problems.
A biopsy can be done with various instruments and, accordingly, there can also be several scenarios for its implementation:
- Most often, special forceps are taken (can be replaced with a scalpel) and a three-millimeter piece of tissue is cut out. Then the uterine cervix is treated with a special solution.
- Another option involves the use of a laser. The essence of the treatment remains the same, only there is no bleeding. A kind of fusion of blood vessels occurs after the laser has acted.
Useful information on the topic:
- Calling a gynecologist to your home
- Medical abortion
- Consultation with a gynecologist
- Surgical abortion
- HCG tests
- Ultrasound during pregnancy
- Intrauterine device
- Diagnosis of sexually transmitted diseases
- Fetal ultrasound
- Pelvic ultrasound
- Ultrasound during pregnancy
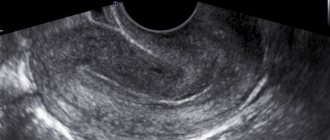
- Transvaginal ultrasound
- Abortion pills
- Discharge in women