- Causes of uterine fibroids
- Types of uterine fibroids
- Symptoms of uterine fibroids
- Why are uterine fibroids dangerous?
- How do modern gynecologists treat uterine fibroids?
- Surgery
- Consequences of removal of uterine fibroids and pregnancy
- A modern method of treating uterine fibroids is UAE.
- Do medications help?
- Are there effective measures to prevent uterine fibroids?
Uterine fibroids are a disease that, according to the Ministry of Health of the Russian Federation, affects approximately one third of women. With this pathology, nodules of smooth muscle tissue form in the wall of the organ. Fibroids do not contain malignant cells, they are not life-threatening, but they can cause some symptoms and problems with pregnancy.
“An ultrasound showed that you have fibroids in your uterus,” these words often make women very worried. It's actually not that scary.
Causes of uterine fibroids
It was previously believed that uterine fibroids are a benign tumor that grows due to an imbalance between female sex hormones - estrogen and progesterone. Modern science knows that this is not so. Scientists and doctors are forced to admit: at the moment it is impossible to name the exact causes of the development of uterine fibroids. There are two theories:
The embryonic theory states that disorders occur even before the girl is born. The fact is that smooth muscle cells in the wall of the fetal uterus mature relatively late - by the 38th week of pregnancy. In the intestines and bladder, these processes are completed by the 16th week. Due to late maturation, the smooth muscle tissue of the uterus remains in an unstable state longer, so there is a higher risk of disorders leading to fibroids.
The traumatic theory states that damage to the myometrium occurs throughout life. It can be caused by multiple periods, previous curettages and abortions, inflammatory diseases, and inaccurate actions of obstetricians during childbirth.
Uterine fibroids do not develop due to hormones, but they do affect its growth. Myomatous nodes almost never appear in girls before their first menstruation and decrease after menopause.
Several factors increase the risk of developing uterine fibroids:
- Age. The disease affects 40–60% of women aged 35 years and 70–80% by 50 years.
- First menstruation at an early age.
- Heredity. The risks are increased if uterine fibroids have been diagnosed in close relatives.
- Overweight.
Fibroids occur more often in women who have never given birth. The risks decrease with the number of pregnancies and births.
Myoma: Observe? Treat? Operate?
Having learned about the presence of fibroids, patients are often confused. Some are scared, believing that the only way out is to remove the uterus, otherwise there is a high risk of cancer.
Others believe that surgery should be avoided at all costs, regardless of medical advice received. The abundance of information on the Internet is confusing and contradictory.
We asked Nikolai Alekseevich Shevchenko, head of the gynecological department, obstetrician-gynecologist of the highest qualification category, Ph.D.
, present modern views on tactics regarding fibroids.
What is fibroid?
Myoma is a benign tumor of the uterus that occurs in 20-40% (according to various sources) of women of reproductive age. Based on the predominance of muscle or connective tissue elements in the tumor, doctors distinguish fibroids, fibroids, and leiomyomas, although more often they simply say “fibroids.” The exact medical name of the disease is “leiomyoma”.
To choose treatment tactics, the size of the tumor is important (it is indicated both in centimeters and in weeks of pregnancy), its location and the number of nodes (single and multiple fibroids are found).
The most commonly diagnosed tumors are subserous and intramural. In the first case, the nodes are located under the peritoneum and protrude above the surface of the uterus. In the second, they are located in the thickness of the uterine wall, between the muscles. Submucosal (in the uterine cavity) location is much less common, but is accompanied by a more vivid clinical picture. There are also retroperitoneal and interligamentous fibroids, but they are rare.
Who is at greatest risk?
It has been proven that the main initiators of fibroid growth are changes in the ratio of the hormones estrogen and progesterone in the body. There are embryonic and traumatic theories of the occurrence of the disease. Scientific research also confirms the role of the inflammatory factor that provokes the growth of nodes.
Women who have a hereditary predisposition, diseases of the endocrine glands, impaired fat metabolism due to low physical activity, chronic inflammatory diseases, and multiple surgical interventions on the uterus (abortion, curettage) are at greatest risk. Irregular sex life also increases the risk of developing fibroids.
In general, the tumor is more common in women living in cities, who are more susceptible to chronic stress, and in women engaged in mental work.
How is fibroid diagnosed?
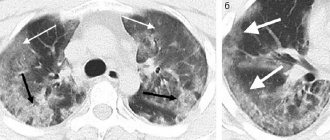
Regular gynecological examination at least once a year, which, unfortunately, is neglected by many women, is the main method of diagnosing and identifying diseases of the uterus. In many cases, even large fibroids do not cause concern to the patient and do not manifest themselves in any way. Additional diagnostic methods are ultrasound, CT, which help determine the size of the tumor, the number, location and characteristics of the nodes.
Why is fibroid dangerous? How high is the risk of a benign tumor transforming into a malignant one?
Fibroids can cause serious discomfort to a woman, worsening her quality of life. Long, heavy and painful menstruation, uterine bleeding outside the menstrual schedule contribute to the development of anemia - hemoglobin drops, general weakness, fatigue, dizziness, shortness of breath, decreased performance, and loss of appetite are observed. Large fibroids can lead to disruption of the functions of neighboring organs that they compress. As a result, frequent urination and constipation, nagging or aching pain in the lower abdomen of varying severity are possible. Fibroids are often combined with other benign diseases of the pelvic organs - endometriosis and endometrial hyperplasia, polyps of the uterine cavity, ovarian cysts and diseases of the fallopian tubes.
For women diagnosed with fibroids, it is advisable to determine the condition of the thyroid and mammary glands. Studies show that in more than 70% of patients, leiomyoma develops against the background of thyroid gland pathology, in 30-70% (according to various sources) against the background of mastopathy.
There is no need to be afraid of the degeneration of a benign tumor into a malignant one; studies show that the so-called “malignancy” of leiomyoma occurs only in 0.3 - 0.7% of cases, and mainly in the presence of cancer heredity.
Methods of treating fibroids. When is surgery necessary? Is it necessary to remove the uterus?
In addition to the size, location and characteristics of the nodes, the choice of treatment tactics is influenced by the patient’s age and her plans for reproductive function, the presence of somatic pathology, and concomitant gynecological diseases. That is why the approach to each patient is strictly individual.
Surgery is not always indicated. If the tumor is single and small in size, surgery is often not necessary. Conservative treatment may be prescribed aimed at normalizing hormonal levels. In this case, constant monitoring of the patient in the antenatal clinic and monitoring the size of the nodes using ultrasound is extremely important. During menopause, fibroids may shrink or disappear.
It is important to understand that the choice of treatment tactics depends not on one, but on many factors; sometimes surgery may be the best method. The generally accepted indications for surgical treatment are: heavy menstrual bleeding leading to anemia; chronic pelvic pain; disruption of the normal functioning of internal organs adjacent to the uterus (rectum, bladder, ureters); large tumor size - more than 6 cm (or 12 weeks); its rapid growth (more than 4 weeks of pregnancy within 1 year); tumor growth in postmenopause; submucosal, interligamentous and low (cervical and isthmus) location of fibroid nodes; reproductive dysfunction (for example, miscarriage); infertility in the absence of other reasons.
Currently, organ-saving techniques are used; the doctor’s task is to preserve the reproductive capabilities of women of childbearing age who are planning to have children. Laparoscopic and laparotomic operations with a limited and clearly justified scope of intervention are available to patients under compulsory medical insurance under high-tech care programs (HTCP) at City Clinical Hospital No. 52.
The high-tech surgical techniques for the treatment of leiomyoma and other diseases of the pelvic organs that we use will be the subject of a separate article. An alternative to surgical treatment may be uterine artery embolization, which is also carried out in City Clinical Hospital No. 52.
Types of uterine fibroids
The wall of the uterus is like a sandwich, the “filling” of which is precisely the muscle layer. The inside of the organ cavity is lined with a mucous membrane (endometrium), and the outside is covered with a serous membrane (perimetry). Myomatous nodes can grow inward or outward, depending on this they are divided into three types:
Subserous fibroids grow on the outer surface of the organ, on a broad base (like a mound) or on a stalk (like a mushroom). They most often do not cause symptoms.
Submucous fibroids protrude into the organ cavity. They are the most problematic, as they most often cause bleeding and problems with pregnancy. Submucous fibroids are divided into three types:
- Zero type - completely located in the uterine cavity.
- The first type - protrude half into the organ cavity.
- The second type - less than a third protrude.
Intramural fibroids are located inside the muscle layer and can grow more toward the uterine cavity, outward, or located in the middle.
Cervical fibroids are distinguished separately.
Symptoms of uterine fibroids

Most women experience no symptoms and are not even aware that they have uterine fibroids. Often the diagnosis is made accidentally, during an ultrasound for another reason. There are situations when a woman has a blood test, anemia (low hemoglobin level) is detected, and further examination shows that the cause is heavy periods due to uterine fibroids.
The three most common symptoms are:
- Heavy, prolonged (more than a week), painful periods.
- If the fibroid is large, it puts pressure on the bladder and rectum. There are problems with bowel movements and urination. A woman may complain that she has constant constipation and often has the urge to urinate.
- Abdominal enlargement also occurs with large uterine fibroids. Women often do not attach much importance to this symptom and believe that they have simply gained weight.
Pain in the lower abdomen, legs and lower back, pain during sexual intercourse and other symptoms are less common and are usually caused by other concomitant diseases.
Uterine fibroids are NOT a malignant tumor. But oncological diseases can manifest similar symptoms, so you need to visit a gynecologist and undergo an examination.
When to do an ultrasound to get the right result
The study can be carried out on any day of the cycle, but the most accurate will be in its first half. To identify uterine fibroids, diagnostics are prescribed 5-7 days after menstruation, when the thickness of the endometrium still allows one to examine the condition of the walls of the organ and notice small myomatous nodes.
After the 10th day, the endometrium thickens, forming folds, and the production of progesterone increases, which provokes a temporary increase in tumors. Both factors distort the real picture of the disease. An exception is possible for sumbucous fibroids - it is better diagnosed on days 19-24 of the cycle.
Preparation for an ultrasound scan for fibroids depends on the chosen diagnostic method: half an hour before the transabdominal examination, it is recommended to drink 2 glasses of water, and before the transvaginal examination, the bladder, on the contrary, needs to be emptied. The day before the procedure, exclude foods that cause gas formation from the diet, and empty your intestines on the morning of the procedure.
Why are uterine fibroids dangerous?
There are many myths about this. Even some gynecologists continue to believe in them, although serious scientific research has long been carried out and all the i’s have been dotted.
The main misconception is that “over time, fibroids will definitely turn into cancer.” And from here the conclusion follows: “the terrible tumor must be removed as quickly as possible.” In fact, uterine fibroids have nothing to do with cancer. Malignant tumors of the myometrium are called leiomyosarcoma. The causes of their occurrence are unknown, and there is no evidence that it can occur due to uterine fibroids.
Myomatous nodes degenerate into malignant tumors no more often than normal myometrium.
The second common myth is that a woman with uterine fibroids will not be able to get pregnant. In fact, this is not always the case. And even if fibroids cause infertility or miscarriage, in most cases this can be corrected with treatment.
Some gynecologists of the “old school” intimidate women, saying that they are no longer allowed to visit bathhouses, solariums, vacation in warm countries, work out in the gym, do massages and physiotherapy, or have sex. This has been proven not to be the case. A woman with uterine fibroids can lead a full, active life if there is no heavy bleeding.
None of these factors will cause the nodes to begin to grow rapidly. In general, the growth of uterine fibroids is an unpredictable thing. In each specific case, it is impossible to say how the disease will behave over time, no matter what lifestyle the woman adheres to, and no matter what restrictions she observes. Therefore, it is important to regularly undergo ultrasound and monitor the condition of the nodes.
For example, in one study, women with uterine fibroids were followed for a year. The results were very different. During this time, some nodes decreased by 25%, while others increased by 138%.
Why are uterine fibroids actually dangerous? Some women develop complications:
- Anemia is a decrease in the level of hemoglobin in the blood due to severe bleeding. Manifests itself in the form of pallor, increased fatigue, weakness, headaches and dizziness.
- Some uterine fibroids lead to infertility and miscarriage.
- Women with uterine fibroids have a 2–2.5 times increased risk of menopausal syndrome, a set of symptoms that occur shortly before, during and after menopause.
How are uterine fibroid sizes determined in weeks?
The size of uterine fibroids depends directly on the woman’s hormonal background, mainly the amount of sex hormones in the woman’s blood.
When their concentration increases, the tumor begins to increase in size. Obstetrician-gynecologists compare the size of fibroids with the size of the uterus at a certain stage of pregnancy. But such a method for assessing the size of fibroids is today considered far outdated, since during an ultrasound examination the fibroid can be measured in centimeters. Depending on their size, fibroids are divided into three categories:
- A small neoplasm is uterine fibroids 5-6 weeks old
. The tumor size is up to 2.5 centimeters. - A medium-sized neoplasm is uterine fibroids up to 13 weeks
. - A large tumor corresponds to more than 12-15 weeks of pregnancy.
An equally important parameter as the size of the fibroid body is its growth rate. So, if during the year small or medium-sized fibroids have increased by more than five weeks (for example, uterine fibroids 7 weeks
has grown to 12), then it is growing rapidly. The reasons for the rapid increase are constant hormonal disorders in a woman’s body.
The size of the fibroids is especially important when a woman is pregnant. So, with a small and small size ( uterine fibroids up to 11 weeks
) pregnancy often proceeds completely normally, without any abnormalities.
In the case of large fibroids (12-15 weeks or more), in most situations, fertilization and further bearing of the child becomes impossible due to blockage of the fallopian tubes, miscarriage or premature birth. With uterine fibroids from 10 weeks
during childbirth, severe bleeding may occur, the course of labor may be disrupted, an infectious-inflammatory process may appear, etc.
How do modern gynecologists treat uterine fibroids?
In modern gynecology, not only the understanding of the mechanism of development of uterine fibroids has changed, but also approaches to its treatment. Different methods are used, each of them has its own advantages and indications. First of all, you need to figure out whether the woman needs treatment. If uterine fibroids are small, do not grow and do not cause symptoms, monitoring over time is sufficient.
So, a woman with uterine fibroids needs to be treated if:
- There is one of the three symptoms that we talked about above.
- The last two or three ultrasounds, performed at intervals of 4-6 months, showed that the fibroids were constantly growing.
- A woman wants to have a child, and fibroids can interfere with pregnancy.
Surgery
Since uterine fibroids were previously considered a tumor (even benign), they fought it radically. Often, doctors immediately suggested that women have their uterus removed. “Are you planning on getting pregnant again? Then why do you need this bag of knots?” Previously, you could often hear this from doctors. And if a modern gynecologist says so, it’s better to stay away from him. The operation of surgical removal of the uterus (hysterectomy) is a last resort; it is permissible when there is absolutely no other way.
The uterus is needed not only for bearing offspring. This organ performs other important functions in the female body. After removal of the uterus, posthysterectomy syndrome develops and can lead to serious complications.
Another surgical option is myomectomy. During the operation, the surgeon removes only the fibroids, the uterus remains in place, and the woman can become pregnant in the future. Surgical intervention can be performed in different ways: through an incision, a puncture (laparoscopically), using robotic installations, without an incision through the vagina.
Consequences of removal of uterine fibroids and pregnancy
After myomectomy, the symptoms of uterine fibroids disappear, and the woman can become pregnant and give birth to a child. But the main disadvantage of surgical treatment is the high risk of relapse. After 4–5 years, fibroids will be detected again in approximately half of the women operated on. Therefore, the operation is indicated in cases where a woman is planning a pregnancy in the near future, and not sometime later.
Other conditions under which fibroid removal may be performed:
- If the doctor is sure that during the operation the uterine cavity will not be opened and the organ will not have to be removed.
- If there are not many large scars left on the uterus.
However, even one scar can create problems during pregnancy and become an indication for a caesarean section. Another possible complication is adhesions, which can lead to infertility. Not to mention that any surgical procedure involves certain risks. In recent years, the list of indications for myomectomy has been greatly reduced because new, minimally invasive techniques have appeared.
What causes fibroids to appear?
The main reasons for the appearance of fibroids are as follows:
- frequent physical activity and stressful situations;
- failures in the production of sex hormones due to ovarian disease;
- ailments of the endocrine system (adrenal glands, thyroid gland);
- the presence of chronic infections (tonsillitis, pyelonephritis, etc.);
- heredity;
- obesity.
The main reasons for the development of an existing neoplasm:
- frequent abortions;
- by the age of thirty, the woman did not experience pregnancy or childbirth, and she also did not have lactation;
- chronic inflammatory processes in the reproductive system;
- long-term use of hormonal contraceptives;
- frequent sunbathing and visiting the solarium.
A modern method of treating uterine fibroids is UAE.
A procedure called uterine artery embolization—UAE for short—has been around for decades, but it has only recently become widely used to treat uterine fibroids. Because of this, even some gynecologists treat her with distrust. But scientific research has conclusively proven that it is an effective and safe method, and it is suitable for most women with uterine fibroids who are eligible for treatment.
The essence of the procedure is that, under X-ray control, a catheter is inserted into the vessel feeding the uterine fibroids, and through it a special embolic drug is inserted. This drug consists of microscopic particles that clog the lumen of small vessels. The myomatous node ceases to receive oxygen and nutrients, dies and is replaced by connective tissue. If the fibroid is located inside the organ cavity on a pedicle, it separates and comes out.
Uterine artery embolization has some advantages over surgical methods for treating fibroids:
- This is a non-invasive procedure. No anesthesia needed. There is no incision - the catheter is inserted into the femoral artery through a small puncture in the upper thigh.
- There is no risk of complications associated with surgery.
- After UAE, recovery occurs quickly. On the second or third day after the procedure, the woman is discharged home.
- The rehabilitation period is much shorter than after myomectomy.
And the most important thing is the result. Studies show that 98% of women after UAE do not need any additional types of treatment. At the same time, after myomectomy, due to the high probability of fibroid recurrence, women are prescribed hormonal drugs.
The risk of recurrence after UAE is less than 1%. If the myomatous node is detected again, the procedure can be repeated.
Uterine artery embolization is the preferred method of treating fibroids if a woman plans to become pregnant in the long term, if many nodes are found in the uterus.
Why don’t gynecologists always tell women about this type of treatment? Firstly, some doctors themselves are poorly informed about the UAE procedure for fibroids. They act on the principle “what if this has not yet been sufficiently studied and is dangerous.” Although, as we have already said, there is no basis for such thoughts: the effectiveness and safety of UAE have been proven in serious clinical studies.
Secondly, not all doctors are proficient in the UAE technique, and not all clinics have the equipment to perform it. Gynecologists work the old fashioned way and are reluctant to refer “their” patients to other specialists.
What should a woman who has been diagnosed with uterine fibroids do? Become a well-informed patient. You can find a lot of information on the Internet about uterine artery embolization. If there is no specialist in your city who practices this type of treatment, you can come to the European clinic or get a consultation with our doctor remotely - to do this, send the results of your research to our email.
Causes and risk factors for the development of uterine fibroids
To date, no obvious causes of this disease have been identified. Probable causes include hormonal imbalance in the body towards the predominance of estrogen over progesterone. This happens in the following cases:
- Early menarche
– increases the number of cell divisions, which increases the risk of mutations in genes that control myometrial proliferation. - Reproductive dysfunction (absence of childbirth)
. Anovulation - with infertility, there is a continuous exposure of estrogens to the myometrium, while pregnancy reduces the time of free exposure of estrogens to the myometrium. - Obesity leads to insulin resistance of body cells
- the fraction of free estrogens increases. At the same time, the conversion of androgens to estrogens in adipose tissue increases - this mechanism is more important in postmenopause.
The growth of nodes (fibroids) is stimulated by such physical factors as insolation, physiotherapeutic procedures in the pelvic area, massages, that is, everything that increases blood circulation in this area. Hereditary predisposition plays a certain role (the presence of fibroids in a mother, sister, grandmother, etc.). There is also an immune theory of the occurrence of these formations: rapid growth of fibroids is observed with severe immune disorders, which contribute to increased cell growth, angiogenesis and inflammation. Various growth factors play an important role. Damage to the structure of the uterus: curettage, inflammation, mutations - lead to the expression of growth factors and increase the risk of uterine fibroids and endometrial pathology. Uterine fibroids can occur for a long time without significant clinical manifestations.
Do medications help?
Drug treatment of uterine fibroids is possible, but indications for its use are limited. It is advisable to use only one drug - ulipristal acetate. It blocks receptors for the hormone progesterone and stops the growth of fibroids. Nodes shrink in 60% of cases. It is recommended to carry out two or three cycles of treatment at intervals of 2 months, while regularly performing ultrasound and monitoring the growth of nodes.
This therapy is indicated only for young women with uterine fibroids up to 3 cm. Its disadvantage is that it has only a temporary effect. It is impossible to predict when fibroids will begin to grow again after treatment.
Is it possible to treat uterine fibroids without surgery?
Naturally, if a woman discovers certain symptoms, she should consult a doctor. After examination and a thorough examination, the gynecologist will decide what treatment needs to be applied - whether it will be conservative treatment or removal of fibroids. The woman’s health status, her age, and desire to have children in the future are also taken into account. In the latter case, the most gentle therapy is selected.
If we are talking about small nodes (less than twelve weeks), which do not increase and do not give serious symptoms, then the doctor can limit the woman to regular examinations every six months and ultrasound examinations, without prescribing any medications. You should also refrain from sunbathing, visiting baths and saunas, and limit physical activity.
If the nodes grow slowly or the fibroids were already diagnosed at medium size, then the doctor prescribes treatment with hormonal drugs that inhibit the growth of estrogen and, in fact, the nodes themselves. With the proper effect, this method of treating uterine fibroids will help avoid surgery to remove it. Usually, combined oral contraceptives are prescribed for these purposes, for example, Mercilon, Novinet, or Rigevidon, Ovidon. Taking these drugs significantly reduces symptoms of uterine fibroids such as bleeding and pain. It is worth noting, however, that drugs in this group do not always help reduce the size of fibroids; they are effective only in cases where initially the nodes were no more than one and a half centimeters.
In other cases, drugs from the group of antiprogestogens - Mifeprestone - are prescribed. It is used both as a therapeutic agent for treatment and as preparation for surgery.
But the most modern, effective and gentle method of treating uterine fibroids today is considered to be FUS ablation. This is not an operation, but a non-invasive method of removing fibroid nodes, which is performed with an ultrasound beam. The doctor directs such a beam only to those places where the tumor is localized and eliminates the nodes themselves. The advantages of this method of treating uterine fibroids are quite obvious:
- with FUS ablation there is no blood loss, no anesthesia is used, and no damage is caused to the organ;
- the reproductive functions of the woman’s body are preserved, the uterus remains intact;
- high efficiency in the treatment of large nodes and multiple fibroids;
- absence of any negative side effects, i.e. no pain, fever, intoxication;
- after the use of FUS ablation, no relapses of the disease were observed;
- rehabilitation and recovery take place in the shortest possible time; the procedure can be performed on an outpatient basis.