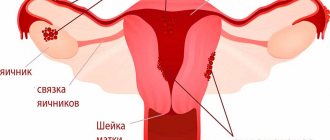
Uterine polyps are local benign neoplasms growing from the endometrial mucosa. They look like tubercles located on a wide base, or round or oval formations on a thin stalk. There may be one or several of them in the uterine cavity; in the latter case they speak of polyposis. The size of polyps varies from a few millimeters to 8 or more centimeters.
- Signs of a polyp in the uterine cavity and their diagnosis
- When is polyp removal necessary?
- Methods for removing endometrial polyps
- What is hysteroscopy of the uterus for polyps
- Types of hysteroscopy
- Indications for hysteroscopy
- Features of the event
- Preparation
- Basic recovery recommendations
- Complications after polyp removal
- Contraindications
Signs of a polyp in the uterine cavity and their diagnosis
Often uterine polyps do not manifest themselves, but some patients have the following symptoms:
- Menorrhagia - heavy menstruation.
- Bleeding outside of menstruation.
- Spotting after sexual intercourse.
- Bleeding during menopause.
- Infertility and miscarriages.
- With large polyps, women may notice copious whitish discharge, discomfort and pain during intercourse, as well as periodic cramping pain in the lower abdomen.
To make a diagnosis, it is necessary to undergo a comprehensive examination, which includes the following procedures:
- Gynecological examination - particularly large polyps can be palpated during manual examination; cervical polyps can be detected during examination in the speculum.
- Ultrasound of the pelvis - in the uterus, growth of the endometrium with a local increase in its mucous layer is detected. The structure of this neoplasm is homogeneous.
- Separate diagnostic curettage followed by histological examination of the obtained material.
- Hysteroscopy - allows you to examine the endometrium from the inside, visualize single or multiple polyps and determine their location. The procedure is also therapeutic in nature, since it allows for the simultaneous removal of all identified tumors and their subsequent histological examination. This is the most effective method for diagnosing a polyp in the uterus.
When is polyp removal necessary?
The choice of patient management tactics and determination of the need to remove the polyp is determined individually. If a woman is of reproductive age and has no symptoms of a polyp, conservative management tactics can be chosen. In this case, the patient should undergo regular monitoring.
In all other cases, removal of polyps is indicated:
- Presence of symptoms of the disease.
- Pre- and postmenopausal periods, even if there are no symptoms.
Methods for removing endometrial polyps
Surgical removal of endometrial polyps is called polypectomy. It involves curettage of the endometrium followed by histological examination of the resulting material. Curettage can be performed blindly, under visual control using ultrasound or hysteroscopy. The latter method is the most preferable because it allows you to control the completeness of polyp removal and avoid the development of surgical complications (uterine perforation, excessive curettage with damage to the basal layer of the endometrium, etc.).

If treatment does not help, and the patient is in menopause, she may be offered surgery to remove the uterus in the following cases:
- Persistent relapses of multiple polyposis.
- High risk of malignancy of polyps.
- The presence of severe symptoms that significantly worsen a woman’s quality of life.
Types of hysteroscopy
There are diagnostic or surgical hysteroscopy. Diagnostic involves only examining the endometrium and endocervix for the presence of pathologies. The study is performed on an outpatient basis and does not require serious anesthesia (local anesthesia and sedation are sufficient) and a long recovery period. Therefore, it was called office hysteroscopy. Based on its results, the doctor draws up a plan for further management of the patient.
Surgical hysteroscopy allows for diagnosis and immediate treatment of identified pathologies. It is performed in an operating room and requires full anesthesia. The procedure is prescribed either when the diagnosis has already been established, or when the likelihood of detecting a pathology is extremely high.
We specialize in surgical hysteroscopy because we believe that invasive diagnostic techniques can be successfully replaced by safer tests. This will help make the correct diagnosis without the risk of surgical complications.
Treatment methods
When treating, doctors use conservative and surgical methods. The choice depends on a number of factors. These are the presence of an inflammatory process and the results of histological examination, the severity of symptoms, the woman’s desire to preserve reproductive function and use hormonal contraceptives.
Minimally invasive hysteroresectoscopy is used for treatment.
The gentle procedure is performed on an outpatient basis under anesthesia and takes about 20 minutes. During the operation, a camera and monitor are used, so the doctor clearly sees the polyp and removes it completely along with the stem. This reduces the likelihood of relapse. Electrodes and a laser are used for removal, leaving no burns or scars on the mucous membrane. The decision about surgery is made after a balanced assessment of the situation - symptoms, size of the polyp and pregnancy planning. The doctor may choose a wait-and-see approach. It is also important that small polyps often spontaneously stop developing.
Drug treatment
The role of conservative therapy is limited. As a rule, it is used to prevent the appearance of polyps, prevent relapses and treat concomitant gynecological and endocrine diseases. For example, in the treatment of chronic endometritis, to restore the cycle, correct estrogen and progesterone levels
Features of the event
Therapeutic hysteroscopy is carried out on a hospital basis, including a one-day hospital in an operating room. An hour before the start of the intervention, premedication is performed - a sedative injection is given. After being delivered to the operating room, the patient is placed in a gynecological chair and given intravenous anesthesia. Next, proceed to the operation:
- Dilation of the cervical canal.
- A certain amount of sterile liquid is injected into the uterine cavity to “straighten” its walls.
- A hysteroscope is inserted through the cervical canal. As it is introduced, a step-by-step examination of all parts of the uterus is performed. First, the cervical canal is examined, then the uterine cavity and its angles.
- If necessary, surgical procedures are performed - taking a biopsy, removing polyps, dissecting synechiae, etc.
- At the end of the operation, fluid is removed from the uterine cavity.

How is the hysteroscopy procedure performed?
Modern medicine knows many different diseases of the genital area. And in some cases, to make a final diagnosis, the doctor needs to carefully examine the inner wall of the uterus. Hysteroscopy provides exactly this opportunity. What is this procedure?
Its essence is quite simple - a hysteroscope is inserted into the uterus through the cervical canal through the external genitalia, with a backlight and a video camera, which transmits to the monitor an enlarged image of the cervical canal and the internal cavity of the uterus, which allows the doctor to carefully examine the structure and, if present, pathology the inner wall of the uterus, viewing them on a large screen.
Hysteroscopy is performed under intravenous anesthesia, which is painless and comfortable for patients.
Preparation
Preparation for hysteroscopy is similar to other surgical interventions in gynecology. First, an examination and, if necessary, certain treatment are carried out. The following tests are performed:
- General blood and urine analysis.
- Coagulogram.
- Blood type and Rh factor.
- Vaginal smear for flora.
- ECG.
- Test for STIs.
- Tests for HIV and parenteral hepatitis.
Hysteroscopy is planned at the beginning of the menstrual cycle (before day 10), since endometrial tumors are clearly visible during this period.

Immediately before surgery, it is recommended to follow these rules:
- Two days before hysteroscopy, avoid sexual contact.
- On the day of the operation, take a shower and then put on underwear made from natural fabrics.
- Remove jewelry and contact lenses.
- Immediately before entering the operating room, empty your bladder.
- Do not eat for at least 6 hours before anesthesia.
How to prepare for hysteroscopy
The woman first undergoes the necessary tests (the list of tests is provided by the attending physician).
In addition, before undergoing hysteroscopy, a woman must inform the doctor about the medications she is taking and the presence of any health complaints.
Before hysteroscopy, it is recommended to cleanse the intestines (this can be done in the evening with a cleansing enema or laxative), as well as empty the bladder and remove hair on the external genitalia.
Basic recovery recommendations
- If an antibiotic is prescribed, take it for as long as your doctor recommends.
- To relieve pain after hysteroscopy, you can take antispasmodics or analgesics.
- Avoid sexual intercourse and heavy physical activity until the bleeding stops, but not less than 10 days.
- Perform hygiene measures in the shower. Taking a bath is not recommended.
- Toilet your genitals as needed, but at least 2 times a day.
- During the recovery period, it is not recommended to use tampons and menstrual cups; discharge should come out of the vagina freely.
Most women generally feel satisfactory after therapeutic hysteroscopy. The main complaints are nagging pain in the lower abdomen and weakness. The full recovery period takes about two weeks. However, if complications develop - fever, heavy bleeding, foul-smelling discharge, you should immediately consult a doctor.
Some useful tips
There are some rules that need to be followed after. Hysteroscopy of the uterus is still a surgical intervention. For some time after the examination, the first two to three days the woman may be bothered by small amounts of blood discharge from the vagina. Usually these symptoms disappear on their own and do not pose a threat to the patient’s health.
Pain in the lower abdomen can last up to ten days. They are felt in the lower abdomen and can sometimes radiate to the lumbosacral region. The intensity of pain ranges from mild to moderate. In cases where the pain is severe or continues after the specified period, a doctor’s consultation is necessary.
There are restrictions, for example, women should not take hot baths - a warm shower would be the best option. It is also strictly forbidden to visit saunas, baths and solariums, as this can lead to uterine bleeding and some other complications. For a while, you should give up vaginal tampons and replace them with sanitary pads. Douching is also prohibited.
Among other things, after hysteroscopy, the gynecologist prescribes sexual rest. If the examination was diagnostic in nature - several days, if there was surgery - about three weeks.
Carefully monitor the condition of your body. Any deterioration in health, fever, or abdominal pain is a reason to visit a doctor. You need to sound the alarm if there is heavy bloody and purulent discharge - in such cases, a gynecological examination is also required.
Hysteroscopy is an effective diagnostic or treatment method that is successfully used in modern gynecology. To obtain a high-quality result and prevent complications, the patient must follow all the doctor’s recommendations both before and after the procedure.
Complications after polyp removal
As after any gynecological operation, the following complications may develop after hysteroscopy:
- Damage to the wall or cervix - treatment may require additional surgery to close the perforation.
- Damage to the cervix - may require stitches.
- Bleeding.
- Infectious complications.
It should be noted that complications after hysteroscopy are much less common than after other gynecological interventions performed “blindly”. But the possibility of their development cannot be completely excluded.
Contraindications to hysteroscopy
Despite the fact that hysteroscopy is considered one of the safest procedures, it has some contraindications:
- To begin with, it is worth noting that examination or surgery is not performed in the presence of inflammatory diseases of the external genitalia. In such cases, you first need to carry out a course of treatment.
- Also, pregnancy is an absolute contraindication to the procedure, as this can lead to its termination.
- Patients suffering from any acute infectious diseases do not undergo hysteroscopy. First you need to carry out appropriate treatment and wait until the main symptoms disappear.
- Contraindications also include heavy uterine bleeding
- Hysteroscopy is contraindicated in women with cervical cancer
Contraindications
- The presence of decompensated chronic diseases that may interfere with anesthesia, for example, cardiovascular pathology.
- Presence of STIs and vulvovaginitis.
- The presence of diseases accompanied by a tendency to bleeding.
Euroonco specialists closely monitor the condition of patients not only in the postoperative period, but also at the initial stage. In this regard, we perform the procedure only after we are convinced that the patient has no contraindications. You can make an appointment for a consultation about uterine polyps by calling:
Book a consultation 24 hours a day
+7+7+78
Causes
There are several factors that can serve as an impetus for their development:
- chronic infections and long-term inflammatory processes that cause changes in endometrial cells;
- hormonal disorders, in particular high levels of estrogen and insufficient production of progesterone;
- injury to the cervix and body of the uterus as a result of abortions, diagnostic curettages and other intrauterine interventions.
Uterine polyps can occur not only independently, but also in combination with endometriosis.