When we take tests in paid laboratories, we receive a form with the result indicated, and there is also a column with an interval of values - intermediate indicators. Not all patients know how to “read” their results correctly. Therefore, in this article we will talk about what reference values mean in analyses.
It is worth noting that medical specialists easily understand test results. Moreover, they focus not only on the value itself, but also on its approximation to the boundaries of the norm.
Why are antibody tests taken?
Tests are performed for the presence of antibodies (immunoglobulins) IgA, IgM and IgG.
- IgA antibodies are the first to be produced by our immune system in response to a virus invasion - if the test for them is positive, it means that the person is in the acute phase of the disease (even if he has no symptoms).
- IgM antibodies begin to be produced later, somewhere on the 3-4th day after the onset of symptoms - this type of antibody is also a marker of primary infection. Typically, testing for IgM antibodies is used as an auxiliary test to clarify the phase of the infectious process.
- IgG antibodies begin to be produced approximately 10-14 days after the onset of symptoms. Their appearance indicates that a person has developed long-term immunity. That is, we are talking either about the late phase of the disease, when the patient is already recovering, or about the fact that the person had COVID-19 earlier.
What test can be done before vaccination?
Currently, IgG antibody tests are most often performed by people about to get vaccinated to ensure they have not previously had COVID-19 asymptomatically or have naturally acquired immunity. If the test shows a positive IgG antibody titer, vaccination can be postponed.
What if a person wants to check the level of antibodies after vaccination? Now many people compare their performance.
You need to understand that the tests used in laboratories are different and the scales they use are also different. Therefore, if you try to compare results (although there is not much point in this), then you must at least be sure that you tested with the same test.
Where to look for references
The simplest and most obvious way to find references is to use a Google or Yandex search engine. The main thing is to write an accurate and specific request. If you need to find Bran Castle in Romania by moonlight, then it’s not enough to type “castle” or “castle in Romania” into the search bar.
Sometimes search engines are not enough. Then special services come to the rescue. One of the most popular is Pinterest, which contains an indescribably huge collection of images, videos, and drawings.
If you don’t like this site, use others, for example: Pixabay, Deviantart, Tumblr. They store many images, illustrations and photographs.
The reference source can be thematic groups and pages on VKontakte, Facebook, Instagram and other social networks. There is especially a lot of suitable material in the profiles of artists, photographers and bloggers.
Movies, TV series, cartoons, music videos and YouTube videos also contain a lot of useful information, sketches and layouts.
Unexpectedly, online stores can also help in your search. You will find photographs of furniture, clothing, interior items and much more on the websites.
For designers and illustrators, the platforms Behance and Dribbble have become a treasure trove of references, for photographers – Art Partner and Kinfolk, for directors and animators – Vimeo.
It doesn’t matter which resource you choose to search for, the main thing is don’t stop at just one. The greater the coverage of sites, the higher the chance of finding something truly worthwhile.
What is the "positivity rate"?
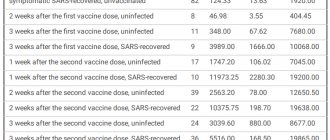
Semi-quantitative tests are used in most cases to determine antibody levels after vaccination. They do not show the exact amount of antibodies formed. But with their help, you can assess the intensity of the immune response - by the brightness of the sample, if the test is carried out using the enzyme-linked immunosorbent assay (ELISA).
Tests from different manufacturers have different scales. In most cases, state laboratories use Vector-best test systems, and their cut-off level is 1. That is, if the indicator is lower, there are no antibodies. From 1 to 1.1 is the so-called gray zone. If the result is higher than 1.1, it means that we have a strong positive reaction of the immune system.
The “positivity rate” shows how many times the level of antibodies in the sample exceeds the threshold level for their recognition. So, for example, the indicator of 15, which the president recently spoke about, is a good result. The majority of those vaccinated with Sputnik V or CoviVac have approximately the same or even higher rate of positive immune response.
At the same time, I would like to note once again that other test manufacturers may have a different scale and, accordingly, different indicators. At the same time, when you receive the test result in the laboratory, you can always see the reference values on the form and compare the result with them.
Sergey Malgavko/TASS
Children
Many parents wonder what are reference values in urine and blood tests in children? Does it differ from adult indicators? Collection of material for analysis can be carried out even from a newborn patient. This helps neonatologists begin treatment immediately if necessary.
The indicators immediately after birth and some time after it are not similar to those to which we are accustomed. A blood test can be alarming with too high levels of hemoglobin, red blood cells and other blood parameters. But it normal. Over time they gradually decrease.
For children in the first day of life, the values of the main blood parameters look like this:
- Red blood cells - 4-8;
- Hemoglobin 179-241;
- Platelets - 180-500
- Leukocytes 9-25;
- Reticulocytes 30-51;
- Lymphocytes 13-37.
And now, closer to 12 months, the reference values change significantly:
- Red blood cells - 4-5;
- Hemoglobin 110-137;
- Platelets - 180-390;
- Leukocytes 6-12;
- Reticulocytes 3-15;
- Lymphocytes 39-73.
What test can be used to check post-vaccination immunity?
This test is called “Quantitative determination of antibodies to the RBD domain of the S1 protein of the coronavirus (IgG antibodies)” (performed by chemiluminescent immunoassay of serum and plasma, Abbot).
This is a quantitative test for IgG antibodies. It will help assess the immune response both in case of infection (or previous COVID-19) and to monitor post-vaccination immunity.
When to do it:
- for a current or past infection no earlier than three weeks after the onset of symptoms or a positive PCR test result;
— to assess post-vaccination immunity three weeks after the second dose of the vaccine.
What the results say:
< 50.0 AU/mL negative:
antibodies to the pathogen are absent or at very low levels.
This may be a period of early infection or the patient may have impaired immune system function.
≥ 50.0 AU/mL positive:
there is an immune response to the infection or a post-vaccination response has formed.
Reference values in blood tests
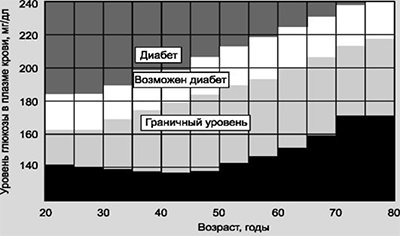
If necessary, in addition to biochemical parameters, other blood components are taken into account. For example, to detect the level of enzymes of specific proteins that are secreted only by malignant tumors, you need to be tested for tumor markers. A diagnostic test of blood from a vein helps to establish hormone levels and reference glucose values for the presence of diabetes mellitus. All these studies have their own generally accepted transcripts.

For tumor markers
To carry out the analysis, blood is taken from a vein. Tumor markers are found in small quantities even in healthy patients, but significant deviations from the norm indicate the presence of a tumor or an inflammatory process in soft tissue cells. The average limits of normal are:
- CA-125 up to 35 IU/ml;
- prostatic antigen 0 – 4 ng/ml;
- CEA 0 – 5 ng/ml;
- CA-15-3 – 9.2-39 IU/ml;
- ACE up to 15 IU/ml;
- CA-19-9 – 9.2-39 IU/ml.
For diabetes
Glucose levels must be analyzed in the morning on an empty stomach; 8 hours before the scheduled date, it is recommended to drink only mineral or plain water. To identify deviations, specialists compare a person’s own reference values with the norms indicated on the analysis form. To carry out the assessment, the average data is taken:
- sugar – from 4 to 6 mmol/l;
- C-septide – 0.9-4 ng/ml;
- immunoreactive insulin – from 4.5 to 15 µU/ml;
- lactate from 0.5 to 2 mmol/l;
- fructosamine - 205-285 mmol/l.
Hormone testing
Preparing for a blood test for hormones applies more to those who are forced to take medications: diuretics or oral contraceptives. To obtain reliable data, you will have to stop taking medications for a certain period of time or reduce their intake to minimum values. It should be noted that the concentration of hormones in women during menstruation is unstable, so this result cannot be considered reliable. The normal limits for hormones are shown in the table.
| Hormone | Normal range |
| TSH | 0.3 – 4.2 µIU/ml |
| TT3 | 1.3 – 3.2 nmol/l |
| Free triiodothyronine | 3.1 – 6.8 pmol/l |
| TT4 | 66 – 181 nmol/l |
| Thyroxine | 10.8 – 22.0 pmol/l |
| Antibodies to thyroglobulin | 0 – 115 IU/ml |
| Antibodies to thyroid peroxidase | 0 – 34 IU/ml |
Are repeat studies needed?
Over time, the intensity of immunity, both in the case of a previous illness and after vaccination, decreases. According to infectious disease specialists, the higher the level of antibodies, the lower the risk of re-infection, as well as the likelihood of severe course and complications of COVID-19.
At the same time, it is recommended to do a repeat test to assess how the antibody level is falling no more than once every six months.

Sergey Karpukhin/TASS
Are there antibody tests that do not show post-vaccination immunity?
Yes. This is, for example, a test for “Antibodies to the nucleocapsid protein (N) of coronavirus IgG (performed by chemiluminescent immunoassay of serum and plasma, Abbot).
This test is not used to assess immune status after vaccination. The fact is that antibodies to the nucleocapsid protein (N) of the SARS-CoV-2 virus are produced only after an illness. Vaccination does not stimulate the production of these antibodies, so this test is useless for assessing post-vaccination immunity.
This test is prescribed:
- to assess the patient’s expected immune status after suffering or in the late phase (recovery) of COVID-19 disease;
- to assess the patient’s immune status, as an auxiliary method for diagnosing coronavirus infection, together with the results of other laboratory tests and clinical data about the patient.
What the results say
negative < 1.4 - negative (antibodies not detected);
positive > 1.4 – positive (antibodies detected).
Why do you need to take a PCR test for COVID-19?
This test is taken to check whether a person is sick or possibly a carrier of the virus (even if he does not have any symptoms of illness), whether he is currently excreting the virus from the upper respiratory tract, that is, is a source of infection for others.
This is the only test for tourists that has already become standard: upon entry, almost all countries require you to present a certificate of the test taken before departure. After returning from the trip, you will have to take the test twice more and upload the result to the government services portal.
In addition, you can take a PCR test to make sure that you are healthy, that is, to exclude an asymptomatic course of the disease. This may be necessary if, for example, you are going to meet elderly relatives and you do not want to risk their health. In addition, with the help of such testing you can check whether you have become infected with coronavirus if you know for sure that you have been in contact with someone who is sick.
Interpretation of the results obtained. Normal or pathological?
When establishing a reference interval, mathematical statistics methods are used, according to which the values of a particular indicator in 95% of healthy people fall within the interval. And the values of the remaining 5% of healthy people are NOT included, interpreted as being outside the reference range, and therefore classified as pathological values. This must be taken into account when interpreting the results. And this is explained by the convention of dividing the population of people into “sick” and “healthy”.
In addition, there is a clear dependence of a number of laboratory parameters on human biological rhythms, time of day, food and drinking regime, which cannot always be taken into account when determining the reference range. From this we can conclude that the limits of normal values may vary. Therefore, what is “norm” for some will be defined as “pathology” for others. Therefore, reference range limits are not absolute indicators of health or disease.
On the other hand, any disease, as a rule, develops unnoticed, characterized by a gradual increase in deviations of the indicator from the “norm” as the disease progresses. This makes clear the importance of assessing the dynamics of changes in this particular laboratory indicator in this particular patient.